Vol 42 Iss S1 April 2021 Vol 42 | Iss S1 | April 2021 Abstracts
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-
EMBASE Find Quick, Relevant Answers to Your Biomedical Questions
EMBASE Find quick, relevant answers to your biomedical questions Piotr Golkiewicz Solution Sales Manager Life Sciences Central and Eastern Europe and Russia Embase® is a registered trademark of Elsevier BV. WHAT IS EMBASE? THE WORLD’S MOST COMPREHENSIVE BIOMEDICAL RESEARCH TOOL Reliable and authoritative content to help the drug and drug-related research community advance new biomedical and pharmaceutical discoveries. Confidence Find all relevant articles that may not otherwise be found by using alternative databases Deep Biomedical Indexing All relevant, up-to-date, biomedical information from the research literature Precise Retrieval Deep and focused research using the most powerful retrieval tools 2 HOW EMBASE DELIVERS VALUE ...by including literature and Conference Scientific In Press We make sure you information resources in a proceedings Journals (unpublished) don’t miss any timely manner biomedical literature ...by reading full-text to The only close identify drugs, diseases, Deep indexing using own taxonomy alternative is adverse affects, clinical (EMTREE) reading trials, drug trade names etc. all the articles ...by enabling advanced search filters to drill down a Very powerful Good precision and comprehensive search to a recall balance relevant and manageable record Search Environment set ...by allowing users to automate Automation and searching and result management documentation E-mail Alerting API Interoperability 3 EMBASE CONTENT 4 EMBASE IS AS COMPREHENSIVE AS POSSIBLE SOURCE TEXT MINING EMBASE SCOPUS Effort / tools required / tools Effort PUBMED GOOGLE 0 % 50 % 100 % Percentage of relevant articles retrieved 5 COMPREHENSIVE CONTENT COVERAGE ON AVERAGE >5000 RECORDS ADDED EACH WORKDAY! Embase: Now covers over 8,400 journals Indexed at Embase (over 5,700 titles) Indexed by MEDLINE (e.g. -

CLINICA CHIMICA ACTA International Journal of Clinical Chemistry and Diagnostic Laboratory Medicine
CLINICA CHIMICA ACTA International Journal of Clinical Chemistry and Diagnostic Laboratory Medicine AUTHOR INFORMATION PACK TABLE OF CONTENTS XXX . • Description p.1 • Audience p.1 • Impact Factor p.1 • Abstracting and Indexing p.2 • Editorial Board p.2 • Guide for Authors p.4 ISSN: 0009-8981 DESCRIPTION . Clinica Chimica Acta is a high-quality journal which publishes original Research Communications in the field of clinical chemistry and laboratory medicine, defined as the diagnosticapplication of chemistry, biochemistry, immunochemistry, biochemical aspects of hematology, toxicology, and molecular biology to the study of human disease in body fluids and cells. The objective of the journal is to publish novel information leading to a better understanding of biological mechanisms of human diseases, their prevention, diagnosis, and patient management. Reports of an applied clinical character are also welcome. Papers concerned with normal metabolic processes or with constituents of normal cells or body fluids, such as reports of experimental or clinical studies in animals, are only considered when they are clearly and directly relevant to human disease. Evaluation of commercial products have a low priority for publication, unless they are novel or represent a technological breakthrough. Studies dealing with effects of drugs and natural products and studies dealing with the redox status in various diseases are not within the journal's scope. Development and evaluation of novel analytical methodologies where applicable to diagnostic clinical chemistry and laboratory medicine, including point-of-care testing, and topics on laboratory management and informatics will also be considered. Studies focused on emerging diagnostic technologies and (big) data analysis procedures including digitalization, mobile Health, and artificial Intelligence applied to Laboratory Medicine are also of interest. -

View December 2013 Report
MOBILE SMART FUNDAMENTALS MMA MEMBERS EDITION DECEMBER 2013 messaging . advertising . apps . mcommerce www.mmaglobal.com NEW YORK • LONDON • SINGAPORE • SÃO PAULO MOBILE MARKETING ASSOCIATION DECEMBER 2013 REPORT A Year of Transformation The new-year invariably kicks off with a slew of predictions, many of which are being usefully defined and shared by our global and regional board members, and many of which are likely to come to fruition or certainly build in momentum. The one area that we feel is certain to gain momentum and have a huge impact on how the mobile industry develops in 2014 is the number of brands that we will see moving from the sidelines and fully into the game. The impact of this will be seen both in the gains in mobile spend as brands move away from the 1% average that we’ve been seeing and start moving towards 10-15% mobile spend with increased ROIs as a result. We will also start to see how mobile is driving both innovation in marketing and transformation of business. As always, the MMA will be providing support and guidance for the entire industry, shining a light on inspiration, capability development, measurement and advocacy allowing all constituents to continue building their businesses, with mobile at its core. We look forward to supporting you and the industry. I wish you much success in 2014. Onwards, Greg Stuart INTRODUCTION 2 MOBILE MARKETING ASSOCIATION DECEMBER 2013 REPORT Table of Contents EXECUTIVE MOVES 4 PUBLIC COMPANY ANALYSIS 7 M&A TRANSACTIONS 9 FINANCING TRANSACTIONS 13 MMA OVERVIEW 25 HIDDEN RIVER OVERVIEW 26 Greg Stuart Todd Parker CEO, Mobile Marketing Association Managing Director, Hidden River [email protected] [email protected] MOBILE MARKETING ASSOCIATION DECEMBER 2013 REPORT Executives on the Move Name New Company Old Company New Company Summary Date T-Mobile is a mobile telephone operator headquartered in Gary King Chief Information Officer, T-Mobile Chief Information Officer, Chico's FAS 12/20/13 Bonn, Germany. -
Searching EMBASE (Elsevier)
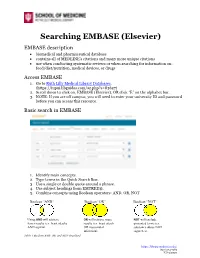
Searching EMBASE (Elsevier) EMBASE description • biomedical and pharmaceutical database • contains all of MEDLINE’s citations and many more unique citations • use when conducting systematic reviews or when searching for information on: food/diet/nutrition, medical devices, or drugs Access EMBASE 1. Go to Ruth Lilly Medical Library Databases. (https://iupui.libguides.com/az.php?s=83627) 2. Scroll down to click on, EMBASE (Elsevier), OR click “E” on the alphabet bar. 3. NOTE: If you are off campus, you will need to enter your university ID and password before you can access this resource. Basic search in EMBASE 1. Identify main concepts. 2. Type terms in the Quick Search Box. 3. Use a single or double quote around a phrase. 4. Use subject headings from EMTREE®. 5. Combine concepts using Boolean operators: AND, OR, NOT Boolean “AND” Boolean “OR” Boolean “NOT” Using AND will retrieve OR will retrieve more NOT will exclude fewer results (ex. heart attacks results (ex. heart attack unwanted terms (ex. AND aspirin) OR myocardial substance abuse NOT infarction) cigarettes). Table 1 Boolean AND, OR, and NOT visualized https://library.mednet.iu.edu/ (317) 274-7182 JCS 5/2020 Results page: Fine-tune your search Filter Results: Beneath the search box: If you click on Quick limits, you will have the options to limit your search to Human subjects and English language. Left-side bar: From most recent search, click each filter to see how many articles are in that subset: e.g. age, gender, drugs used, and other diseases. Work with Search History: • Combine searches using AND; OR • Select any search in History to recall the results. -

Adolescent Victims' Experiences with Cyberbullying: a Grounded Theory Study Melvina S
University of North Dakota UND Scholarly Commons Theses and Dissertations Theses, Dissertations, and Senior Projects January 2016 Adolescent Victims' Experiences With Cyberbullying: A Grounded Theory Study Melvina S. Brandau Follow this and additional works at: https://commons.und.edu/theses Recommended Citation Brandau, Melvina S., "Adolescent Victims' Experiences With Cyberbullying: A Grounded Theory Study" (2016). Theses and Dissertations. 1879. https://commons.und.edu/theses/1879 This Dissertation is brought to you for free and open access by the Theses, Dissertations, and Senior Projects at UND Scholarly Commons. It has been accepted for inclusion in Theses and Dissertations by an authorized administrator of UND Scholarly Commons. For more information, please contact [email protected]. ADOLESCENT VICTIMS’ EXPERIENCES WITH CYBERBULLYING: A GROUNDED THEORY STUDY by Melvina Sue Brandau Associate of Applied Science, University of Rio Grande, 1999 Bachelor of Science, Indiana Wesleyan University, 2005 Master of Science, Indiana Wesleyan University, 2007 A Dissertation Submitted to the Graduate Faculty of the University of North Dakota in partial fulfillment of the requirements for the degree of Doctor of Philosophy Grand Forks, North Dakota May 2016 Copyright 2016 Melvina Brandau ii PERMISSION Title Adolescent Victims’ Experiences with Cyberbullying: A Grounded Theory Study Department College of Nursing and Professional Disciplines Degree Doctor of Philosophy In presenting this dissertation in partial fulfillment of the requirements for a graduate degree from the University of North Dakota, I agree that the library of this University shall make it freely available for inspection. I further agree that permission for extensive copying for scholarly purposes may be granted by the professor who supervised my dissertation work or, in her absence, by the Chairperson of the department or the dean of the School of Graduate Studies. -

Journals 2016 Catalog Directors’ Letter
MIT Press Journals 2016 catalog Directors’ Letter Dear Friends, The MIT Press celebrated its 50th anniversary in 2012, and the inclination to ponder our distinguished history remains strong, perhaps even more so this year with the change in Press leadership—Amy Brand was named Director of the MIT Press in July of 2015. The Press’s journals division, which was founded in 1972, ten years after the books division, also has a significant publishing legacy to consider, with over 80 journals published since the division’s inception. Some, such as Linguistic Inquiry and The Journal of Interdisciplinary History, have grown with us from the very beginning. Other core titles like International Security, October, The Review of Economics and Statistics and Journal of Cognitive Neuroscience joined the Press over the following decades, providing a solid base for the high-quality and innovative scholarship that our journals division is well known for. Today, we continue to push the boundaries of scholarly publishing and communication. We relish discovering new fields to publish in, and working with scholars who are establishing new domains of research and inquiry. In keeping with that spirit, the Press is proud to launch a new open access journal in 2016, Computational Psychiatry, to serve a burgeoning field that brings together experts in neuroscience, decision sciences, psychiatry, and computation modeling to apply new quantitative techniques to our understanding of psychiatric disorders. Developing new ways of delivering journal articles and providing a richer range of metrics around their usage and impact is another current effort. On our mitpressjournals.org site, the Press is providing Altmetric badges for select titles to give an improved sense of the breadth of a journal article’s reach. -

View Document
11/07/2017 Embase Select Language ▼ Logout Session Results / Record 4 of 173 Full record Record 4 Similar records | Add to Clipboard | Email Record The utilisation of modern transport and telecommunications platforms to assist in the remote provision of paediatric cancer diagnostics in Tanzania Mcdermott M., O'Hare K., Scanlon P., Grehan D., Rooney S., Laiti R., Kaijage J., Jumanne S., O'Sullivan M. Pediatric Blood and Cancer 2016 63 Supplement 3 (S71) Go to publisher for the full text Abstract Background/Objectives: The acquisition of a pathologic diagnosis represents a critical point in the management of children with malignant disease, allowing staff to plan a therapeutic pathway. In resource poor settings, diagnoses help to identify children who will benefit from the limited interventions available and those who will not. Access to timely diagnoses can be a challenge in low and middle income countries. While enhanced local laboratory capacity is the ultimate answer, interim solutions are needed to assist programs with existing deficits. Modern transport and telecommunications technology can facilitate this process. Design/Methods: Muhimbili University, Dar es Salaam, provides a paediatric cancer program for Tanzania. As part of a formal twinning arrangement, laboratory staff in Dublin have provided interim diagnostic services while helping to develop local paediatric cancer diagnostic capacity in Tanzania. Samples are transported free via DHL® couriers. Preliminary reports are communicated to local clinical staff via WhatsApp with final reports scanned and e-mailed. Results: Since 2008, almost 1000 cancer samples have been transported from Dar to Dublin. Transport time is two working days. In 92% of cases, a preliminary communication regarding specimen adequacy and provisional diagnosis was communicated via WhatsApp the day after receipt. -

Social Media Skills Dominique Jackson
13 Must-Have Social Media Skills by Dominique Jackson on January 19, 2016 What are the ingredients of an ideal social media manager? If you were to ask this question 10 years ago, it would probably be a fairly short list. But as social media marketing evolved over the years with new technology and a wider audience, we’ve been able to see certain skills and traits that separate the top marketers from the rest. Learning and sharpening these skills can help propel your social media efforts into elite status, and avoid being one of the many brands that can’t seem to make any progress. Whether you’re looking to hire a new social media manager or simply want to improve your own strategy, focus on building up these 13 social media skills: 1. Community Management When you look at the top brands on social media, you’ll notice something they all have in common is a community aspect. Social media marketing is all about connecting with your audience. Once you’re able to build that connection and grow a community, your audience will start creating user generated content (UGC) and your reach will spread organically. Start by acknowledging your top sharers. These are the people who are consistently engaging with you and your content on social media. You can find this in the Sprout Social Trends report. Want to know what other pieces should be a part of your social team? We partnered with HubSpot to create a free guide on how to build a social media dream team from scratch, including some of the key positions you should fill.Download it here. -
How to Catch a Unicorn
How to Catch a Unicorn An exploration of the universe of tech companies with high market capitalisation Author: Jean Paul Simon Editor: Marc Bogdanowicz 2016 EUR 27822 EN How to Catch a Unicorn An exploration of the universe of tech companies with high market capitalisation This publication is a Technical report by the Joint Research Centre, the European Commission’s in-house science service. It aims to provide evidence-based scientific support to the European policy-making process. The scientific output expressed does not imply a policy position of the European Commission. Neither the European Commission nor any person acting on behalf of the Commission is responsible for the use which might be made of this publication. JRC Science Hub https://ec.europa.eu/jrc JRC100719 EUR 27822 EN ISBN 978-92-79-57601-0 (PDF) ISSN 1831-9424 (online) doi:10.2791/893975 (online) © European Union, 2016 Reproduction is authorised provided the source is acknowledged. All images © European Union 2016 How to cite: Jean Paul Simon (2016) ‘How to catch a unicorn. An exploration of the universe of tech companies with high market capitalisation’. Institute for Prospective Technological Studies. JRC Technical Report. EUR 27822 EN. doi:10.2791/893975 Table of Contents Preface .............................................................................................................. 2 Abstract ............................................................................................................. 3 Executive Summary .......................................................................................... -

Search Worksheet
Search Worksheet Search Steps 1. State the research topic/clinical question as an answerable question – use a consistent method to frame the question, such as PICO(M) or its variants. Refer to Tables 2 and 3 on the back side. 2. Identify appropriate databases – refer to Table 4 on the back side. Do not rely on a single database. 3. Identify possible search terms, keywords, and synonyms based on concepts identified in step 1. 4. Conduct the search in the selected databases – search each concept separately. Use: OR – Combines synonyms, related terms, or spelling variations for each concept. (OR means more.) AND – Combine concepts to find citations which are “about” all of the concepts. (AND means less.) 5. Apply limits to narrow search results to relevant citations 6. Refine and save search Table 1 – Organize your search plan. State the research topic/clinical question as an answerable question. Concepts Concept 1 Concept 2 Concept 3 Concept 4 Identify key concepts Identify subject headings for each key concept Identify keywords for each key concept Apply limits, i.e., Publication Types, Age Groups, Years, Language, etc. 213 - Dec-20 Table 2 – PICO(M) Components P Patient or Problem What is the important patient problem or condition? How would you describe the important characteristics of the patient? Intervention, Indicator, What do you want to do to help the patient? Do you want to consider a specific treatment, diagnostic test, exposure or risk I Exposure, Prognostic Factor factor? Is there a prognostic factor that might affect the -

Cleveland Police Are Dedicated to Promoting Safer and More
Cleveland Police are dedicated to promoting Cyber Bullying safer and more responsible use of online Cyber bullying is bullying that takes place technology and mobile phones. While the using electronic technology. Electronic internet and the technology used to access it technology includes devices and equipment is rapidly evolving, providing exciting new such as mobile phones, computers, and experiences and methods of communicating, tablets as well as communication tools it is important that children and professionals including social media sites, text messages, alike do not forget the risks that are chat, and websites. associated with it. 5 Types of Cyber bullying As a result of cultural developments like cyber bullying being a relatively recent Harassing Someone phenomenon, ethics are still being Using text messaging, instant established by both those who create messaging and email to harass, legislation based on this concept and how to threaten or embarrass the target. regulate it. Nevertheless, the law currently Posting rumours, threats or views any sexual pictures of anyone under embarrassing information on social the age of 18 years as illegal due to the networking sites such as Facebook, inherent risks to children being exploited and Twitter, and Instagram. their pictures being distributed. Engaging in “warning wars.” Many This booklet is an opportunity to provide Internet Service Providers offer a way children and professionals with the to report a user who is saying knowledge and awareness of how to utilise something inappropriate. Kids use the the technology available to them in an “warn” button as a way to get the victim informed way to keep themselves and each in trouble or kicked offline. -

Driving Change: a Marketing Model
Driving Change:! A Marketing Model" Howard Jacobson, PhD" Natural Human Impulses" • Judge" • Push" © howieConnect, Inc. All Rights Reserved Natural Human Responses" • To being judged?" • To being pushed?" © howieConnect, Inc. All Rights Reserved Manifestations of Power" • Command " • Control" © howieConnect, Inc. All Rights Reserved Power is" “Asymmetric control over valued resources in social relations” – Magee & Galinsky, 2008" © howieConnect, Inc. All Rights Reserved If You Had Power…" • We wouldn’t be talking about this today" © howieConnect, Inc. All Rights Reserved Powerless Persuaders" • Marketers!" © howieConnect, Inc. All Rights Reserved Marketing Mindsets" • Understand" • Align" © howieConnect, Inc. All Rights Reserved Agenda" 1. The Goal" 2. A Marketing Model of Driving Change" 3. Strategies" © howieConnect, Inc. All Rights Reserved The Goal" • Give you some approaches and tools to bring about change" • Enable you to work more effectively with people who are acting like obstacles" " © howieConnect, Inc. All Rights Reserved A Marketing Model of Change" © howieConnect, Inc. All Rights Reserved Irony" • “I’ve been beating my head against a wall trying to get them to change for five years now.”" © howieConnect, Inc. All Rights Reserved Why Do People Resist Change?" • We don’t" • We resist losing control" • Unpredictability is an evolutionary risk" • When change brings uncertainty, we cling to the familiar" © howieConnect, Inc. All Rights Reserved An Ocean of Unknowns" • Regulatory" • Legal" • Scope of required investment" • Cost of future abandonment" • Appropriate metrics" • Potential ROI" • Lost opportunity costs" © howieConnect, Inc. All Rights Reserved The Funny Thing About Control" • It doesn’t really exist" • We have it until we don’t" © howieConnect, Inc. All Rights Reserved Our Task" • To let go of control" • Stop judging" • Stop pushing" • Not about being “spiritual” or “good”" • About acknowledging reality" © howieConnect, Inc.