Diagnostic Approach to Anemia
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Predictors of Autoimmune Hemolytic Anemia in Beta-Thalassemia
Blood Cells, Molecules and Diseases 79 (2019) 102342 Contents lists available at ScienceDirect Blood Cells, Molecules and Diseases journal homepage: www.elsevier.com/locate/bcmd Predictors of autoimmune hemolytic anemia in beta-thalassemia patients with underlying red blood cells autoantibodies T ⁎ Monia Ben Khaleda,b, , Monia Ouedernia,b, Nessrine Sahlia,b, Nawel Dhouibb, Ahmed Ben Abdelazizc, Samia Rekayaa,b, Ridha Koukia,b, Houda Kaabid, Hmida Slamad, Fethi Melloulia,b, Mohamed Bejaouia,b a Faculty of Medicine, University of Tunis El Manar, Tunis, Tunisia b Pediatric Immuno-Hematology Unit, Bone Marrow Transplantation Center Tunis, Tunis, Tunisia c Information System Directions, Sahloul University Hospital, Sousse, Tunisia d National Center of Blood Transfusion, Tunis, Tunisia ARTICLE INFO ABSTRACT Editor: Mohandas Narla In beta-thalassemia patients, erythrocyte autoantibodies can remain silent or lead to Autoimmune Hemolytic Keywords: Anemia (AIHA).The aim of this study was to identify predictors of AIHA in beta-thalassemia patients with Autoimmune hemolytic anemia positive Direct Antiglobulin Test (DAT), in Tunisia. Thalassemia This longitudinal prognosis study was carried out on beta-thalassemia patients with a positive confirmed Transfusion DAT. Predictors of AIHA were identified the Kaplan-Meier method. A Cox model analysis was used to identify Autoantibodies independent predictors. Red blood cells Among 385 beta thalassemia patients, 87 developed positive DAT (22.6%). Autoimmune hemolytic anemia Direct antiglobulin test was occurred in 25 patients. Multivariate analysis showed that AIHA was independently associated with beta- thalassemia intermedia and similar family history of AIHA. Splenectomy in patients with positive DAT was independently associated with an increased risk of AIHA (HR = 6.175, CI: 2.049–18.612, p < 0.001). -

The Role of Methemoglobin and Carboxyhemoglobin in COVID-19: a Review
Journal of Clinical Medicine Review The Role of Methemoglobin and Carboxyhemoglobin in COVID-19: A Review Felix Scholkmann 1,2,*, Tanja Restin 2, Marco Ferrari 3 and Valentina Quaresima 3 1 Biomedical Optics Research Laboratory, Department of Neonatology, University Hospital Zurich, University of Zurich, 8091 Zurich, Switzerland 2 Newborn Research Zurich, Department of Neonatology, University Hospital Zurich, University of Zurich, 8091 Zurich, Switzerland; [email protected] 3 Department of Life, Health and Environmental Sciences, University of L’Aquila, 67100 L’Aquila, Italy; [email protected] (M.F.); [email protected] (V.Q.) * Correspondence: [email protected]; Tel.: +41-4-4255-9326 Abstract: Following the outbreak of a novel coronavirus (SARS-CoV-2) associated with pneumonia in China (Corona Virus Disease 2019, COVID-19) at the end of 2019, the world is currently facing a global pandemic of infections with SARS-CoV-2 and cases of COVID-19. Since severely ill patients often show elevated methemoglobin (MetHb) and carboxyhemoglobin (COHb) concentrations in their blood as a marker of disease severity, we aimed to summarize the currently available published study results (case reports and cross-sectional studies) on MetHb and COHb concentrations in the blood of COVID-19 patients. To this end, a systematic literature research was performed. For the case of MetHb, seven publications were identified (five case reports and two cross-sectional studies), and for the case of COHb, three studies were found (two cross-sectional studies and one case report). The findings reported in the publications show that an increase in MetHb and COHb can happen in COVID-19 patients, especially in critically ill ones, and that MetHb and COHb can increase to dangerously high levels during the course of the disease in some patients. -

Section 8: Hematology CHAPTER 47: ANEMIA
Section 8: Hematology CHAPTER 47: ANEMIA Q.1. A 56-year-old man presents with symptoms of severe dyspnea on exertion and fatigue. His laboratory values are as follows: Hemoglobin 6.0 g/dL (normal: 12–15 g/dL) Hematocrit 18% (normal: 36%–46%) RBC count 2 million/L (normal: 4–5.2 million/L) Reticulocyte count 3% (normal: 0.5%–1.5%) Which of the following caused this man’s anemia? A. Decreased red cell production B. Increased red cell destruction C. Acute blood loss (hemorrhage) D. There is insufficient information to make a determination Answer: A. This man presents with anemia and an elevated reticulocyte count which seems to suggest a hemolytic process. His reticulocyte count, however, has not been corrected for the degree of anemia he displays. This can be done by calculating his corrected reticulocyte count ([3% × (18%/45%)] = 1.2%), which is less than 2 and thus suggestive of a hypoproliferative process (decreased red cell production). Q.2. A 25-year-old man with pancytopenia undergoes bone marrow aspiration and biopsy, which reveals profound hypocellularity and virtual absence of hematopoietic cells. Cytogenetic analysis of the bone marrow does not reveal any abnormalities. Despite red blood cell and platelet transfusions, his pancytopenia worsens. Histocompatibility testing of his only sister fails to reveal a match. What would be the most appropriate course of therapy? A. Antithymocyte globulin, cyclosporine, and prednisone B. Prednisone alone C. Supportive therapy with chronic blood and platelet transfusions only D. Methotrexate and prednisone E. Bone marrow transplant Answer: A. Although supportive care with transfusions is necessary for treating this patient with aplastic anemia, most cases are not self-limited. -

A Distant Gene Deletion Affects Beta-Globin Gene Function in an Atypical Gamma Delta Beta-Thalassemia
A distant gene deletion affects beta-globin gene function in an atypical gamma delta beta-thalassemia. P Curtin, … , A D Stephens, H Lehmann J Clin Invest. 1985;76(4):1554-1558. https://doi.org/10.1172/JCI112136. Research Article We describe an English family with an atypical gamma delta beta-thalassemia syndrome. Heterozygosity results in a beta-thalassemia phenotype with normal hemoglobin A2. However, unlike previously described cases, no history of neonatal hemolytic anemia requiring blood transfusion was obtained. Gene mapping showed a deletion that extended from the third exon of the G gamma-globin gene upstream for approximately 100 kilobases (kb). The A gamma-globin, psi beta-, delta-, and beta-globin genes in cis remained intact. The malfunction of the beta-globin gene on a chromosome in which the deletion is located 25 kb away suggests that chromatin structure and conformation are important for globin gene expression. Find the latest version: https://jci.me/112136/pdf A Distant Gene Deletion Affects ,8-Globin Gene Function in an Atypical '6y5-Thalassemia Peter Curtin, Mario Pirastu, and Yuet Wai Kan Howard Hughes Medical Institute and Department ofMedicine, University of California, San Francisco, California 94143 John Anderson Gobert-Jones Department ofPathology, West Suffolk County Hospital, Bury St. Edmunds IP33-2QZ, Suffolk, England Adrian David Stephens Department ofHaematology, St. Bartholomew's Hospital, London ECIA-7BE, England Herman Lehmann Department ofBiochemistry, University ofCambridge, Cambridge CB2-lQW, England Abstract tologic picture of f3-thalassemia minor in adult life. Globin syn- thetic studies reveal a ,3 to a ratio of -0.5, but unlike the usual We describe an English family with an atypical 'yS6-thalassemia fl-thalassemia heterozygote, the levels of HbA2 (and HbF) are syndrome. -

Anemia in Heart Failure - from Guidelines to Controversies and Challenges
52 Education Anemia in heart failure - from guidelines to controversies and challenges Oana Sîrbu1,*, Mariana Floria1,*, Petru Dascalita*, Alexandra Stoica1,*, Paula Adascalitei, Victorita Sorodoc1,*, Laurentiu Sorodoc1,* *Grigore T. Popa University of Medicine and Pharmacy; Iasi-Romania 1Sf. Spiridon Emergency Hospital; Iasi-Romania ABSTRACT Anemia associated with heart failure is a frequent condition, which may lead to heart function deterioration by the activation of neuro-hormonal mechanisms. Therefore, a vicious circle is present in the relationship of heart failure and anemia. The consequence is reflected upon the pa- tients’ survival, quality of life, and hospital readmissions. Anemia and iron deficiency should be correctly diagnosed and treated in patients with heart failure. The etiology is multifactorial but certainly not fully understood. There is data suggesting that the following factors can cause ane- mia alone or in combination: iron deficiency, inflammation, erythropoietin levels, prescribed medication, hemodilution, and medullar dysfunc- tion. There is data suggesting the association among iron deficiency, inflammation, erythropoietin levels, prescribed medication, hemodilution, and medullar dysfunction. The main pathophysiologic mechanisms, with the strongest evidence-based medicine data, are iron deficiency and inflammation. In clinical practice, the etiology of anemia needs thorough evaluation for determining the best possible therapeutic course. In this context, we must correctly treat the patients’ diseases; according with the current guidelines we have now only one intravenous iron drug. This paper is focused on data about anemia in heart failure, from prevalence to optimal treatment, controversies, and challenges. (Anatol J Cardiol 2018; 20: 52-9) Keywords: anemia, heart failure, intravenous iron, ferric carboxymaltose, quality of life Introduction g/dL in men) (2). -

A Rapid and Quantitative D-Dimer Assay in Whole Blood and Plasma on the Point-Of-Care PATHFAST Analyzer ARTICLE in PRESS
MODEL 6 TR-03106; No of Pages 7 ARTICLE IN PRESS Thrombosis Research (2007) xx, xxx–xxx intl.elsevierhealth.com/journals/thre REGULAR ARTICLE A rapid and quantitative D-Dimer assay in whole blood and plasma on the point-of-care PATHFAST analyzer Teruko Fukuda a,⁎, Hidetoshi Kasai b, Takeo Kusano b, Chisato Shimazu b, Kazuo Kawasugi c, Yukihisa Miyazawa b a Department of Clinical Laboratory Medicine, Teikyo University School of Medical Technology, 2-11-1 Kaga, Itabashi, Tokyo 173-8605, Japan b Department of Central Clinical Laboratory, Teikyo University Hospital, Japan c Department of Internal Medicine, Teikyo University School of Medicine, Japan Received 11 July 2006; received in revised form 7 December 2006; accepted 28 December 2006 KEYWORDS Abstract The objective of this study was to evaluate the accuracy indices of the new D-Dimer; rapid and quantitative PATHFAST D-Dimer assay in patients with clinically suspected Deep-vein thrombosis; deep-vein thrombosis (DVT). Eighty two consecutive patients (34% DVT, 66% non-DVT) Point-of-care testing; with suspected DVT of a lower limb were tested with the D-Dimer assay with a Chemiluminescent PATHFAST analyzer. The diagnostic value of the PATHFAST D-Dimer assay (which is immunoassay based on the principle of a chemiluminescent enzyme immunoassay) for DVT was evaluated with pre-test clinical probability, compression ultrasonography (CUS). Furthermore, each patient underwent contrast venography and computed tomogra- phy, if necessary. The sensitivity and specificity of the D-Dimer assay using 0.570 μg/ mL FEU as a clinical cut-off value was found to be 100% and 63.2%, respectively, for the diagnosis of DVT, with a positive predictive value (PPV) and negative predictive value (NPV) of 66.7% and 100%, respectively. -
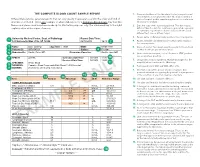
The Complete Blood Count Sample Report 1
THE COMPLETE BLOOD COUNT SAMPLE REPORT 1. Name and address of the lab where the test was performed. Tests may be run in a physician office lab, a lab located in a Different laboratories generate reports that can vary greatly in appearance and in the order and kind of The Complete Blood Count Sample Report clinic or hospital, and/or samples may be sent to a reference information included. This is one example of what a lab report for a Complete Blood Count may look like. laboratory for analysis. NamesDifferent and laboratories places used generate have been reports made that up can for vary illustrative greatly inpurposes appearance only. andThe innumbered the order keyand tokind the of right 2. Date this copy of the report was printed. This date may be explainsinformation a few included. of the reportThis is elements.one exampl e of what a lab report for a Complete Blood Count may look like. different than the date the results were generated, especially Names and places used have been made up for illustrative purposes only. Point your cursor at a number on cumulative reports (those that include results of several to learn about the different report elements. different tests run on different days). 3. Patient name or identifier. Links results to the correct person. 1 University Medical Center, Dept. of Pathology Report Date/Time: 123 University Way, City, ST 12345 02/10/2014 16:40 2 4. Patient identifier and identification number. Links results to the correct person. 3 Name: Doe, John Q. Age/Sex: 73/M DOB: 01/01/1941 5. -

Severe Aplastic Anemia
Severe AlAplas tic AiAnemia Monica S. Thakar, MD Pediatric BMT Medical College of Wisconsin Outline of Talk 1. Clinical description of aplastic anemia 2. Data collection forms And a couple of quizzes in between… CLINICAL DESCRIPTIONS What is aplastic anemia? • More than just anemia – Involves low counts in 2 of 3 cell lines: red blood cells (RBC), white blood cells (WBC), pltltlatelets • Should NOT involve dysplasia – EiException: RBC can sometimes be dlidysplastic • Should have NORMAL cytogenetics • If dysplasia (beyond RBCs) or abnormal cytogenetics seen, think myelodysplastic syndrome (MDS) What is “severe” aplastic anemia? • Marrow cellularity ≤25% AND • Two of the following peripheral blood features: – Absolute neutrophil count (ANC) < 0.5 x 109/L – Platelet count <20 x 109/L – Absolute reticulocyte count < 40 x 109/L • “Very” severe aplastic anemia – Same as above except ANC <0.2 x 109/L NORMAL BttBottom Li ne: Severely Reduced HtitiHematopoietic Stem Cell Precursors SEVERE APLASTIC ANEMIA IBIn Bone M arrow Epidemiology • Half of cases seen in first 3 decades of life • Incidence: – 2 cases/m illion in WtWestern countitries – 2‐3 fold higher in Asia • Ethnic predisposition: – Asian • Genetics vs different environmental exposures? • Sex predisposition: M:F is 1:1 Pathoppyhysiology : 3 Main Mechanisms Proposed 1. Immune‐mediated – HthiHypothesis: RdRevved‐up T cells dtdestroy stem cells – Observation: Immunosuppression improves blood counts 2. Stem‐cell “depletion” or “defect” – Hypothesis: Drugs or viruses directly destroy stem cells -

Erythrocytes: Overview, Morphology, Quantity by AH Rebar Et
In: A Guide to Hematology in Dogs and Cats, Rebar A.H., MacWilliams P.S., Feldman B.F., Metzger F.L., Pollock R.V.H. and Roche J. (Eds.). Publisher: Teton NewMedia, Jackson WY (www.veterinarywire.com). Internet Publisher: International Veterinary Information Service, Ithaca NY (www.ivis.org), 8-Feb-2005; A3304.0205 Erythrocytes: Overview, Morphology, Quantity A.H. Rebar1, P.S. MacWilliams2, B.F. Feldman 3, F.L. Metzger 4, R.V.H. Pollock 5 and J. Roche 6 1Dept of Veterinary Pathobiology, School of Veterinary Medicine, Purdue University, IN,USA. 2Dept of Pathobiological Sciences, School of Veterinary Medicine, University of Wisconsin, WI, USA. 3Dept of Biomedical Sciences & Pathobiology, VA-MD - Regional College of Veterinary Medicine, Virginia Tech, VA, USA. 4Metzger Animal Hospital,State College,PA, USA. 5Fort Hill Company, Montchanin, DE, USA. 6 Hematology Systems, IDEXX Laboratories, Westbrook, ME, USA. Overview Production Red blood cells (RBC) are produced in the bone marrow. Numbers of circulating RBCs are affected by changes in plasma volume, rate of RBC destruction or loss, splenic contraction, erythropoietin (EPO) secretion, and the rate of bone marrow production. A normal PCV is maintained by an endocrine loop that involves generation and release of erythropoietin (EPO) from the kidney in response to renal hypoxia. Erythropoietin stimulates platelet production as well as red cell production. However, erythropoietin does not stimulate white blood cell (WBC) production. Erythropoiesis and RBC numbers are also affected by hormones from the adrenal cortex, thyroid, ovary, testis, and anterior pituitary. Destruction Red cells have a finite circulating lifespan. In dogs, the average normal red cell circulates approximately 100 days. -

Kawasaki Disease with Glucose-6-Phosphate Dehydrogenase Deficiency, Case Report
Saudi Pharmaceutical Journal (2014) xxx, xxx–xxx King Saud University Saudi Pharmaceutical Journal www.ksu.edu.sa www.sciencedirect.com CASE REPORT Kawasaki disease with Glucose-6-Phosphate Dehydrogenase deficiency, case report Hesham Radi Obeidat a,*, Sahar Al-Dossary b, Abdulsalam Asseri a a Pharmacy Department, Saad Specialist Hospital, Alkhobar 31952, Saudi Arabia b Pediatric and Neonatology Department, Saad Specialist Hospital, Alkhobar 31952, Saudi Arabia Received 28 August 2014; accepted 11 November 2014 KEYWORDS Abstract Kawasaki disease (KD) is an acute, self-limited vasculitis of unknown etiology that Kawasaki disease; occurs predominantly in infants and children younger than 5 years of age. Coronary artery abnor- G6PD; malities are the most serious complication. Aspirin Based on the literatures infusion of Intravenous Immunoglobulin of 2 g/kg and a high dose of oral aspirin up to 100 mg/kg/day are the standard treatment for Kawasaki disease in the acute stage, and should be followed by antiplatelet dose of aspirin for thrombocytosis. Glucose-6-Phos- phate Dehydrogenase (G6PD) deficiency is an inherited X-linked hereditary disorder, and aspirin can induce hemolysis in patients with G6PD deficiency. We report a case of a 5 year and 8 month old male with KD and G6PD deficiency. ª 2014 The Authors. Production and hosting by Elsevier B.V. on behalf of King Saud University. This is an open access article under the CC BY-NC-ND license (http://creativecommons.org/licenses/by-nc-nd/3.0/). 1. Introduction genetic predisposition or infectious agents are likely to be the cause. Kawasaki disease was first described in 1967 by Tomisaku Recently, guidelines were published by the American Heart Kawasaki and has replaced acute rheumatic fever as the lead- Association (AHA) to aid in the diagnosis and management of ing cause of acquired heart disease among children in devel- Kawasaki disease. -
Evaluation of Complete Blood Count Parameters for Diagnosis In
Original Investigation / Özgün Araştırma DOI: 10.5578/ced.68886 • J Pediatr Inf 2020;14(2):e55-e62 Evaluation of Complete Blood Count Parameters for Diagnosis in Children with Sepsis in the Pediatric Intensive Care Unit Pediatrik Yoğun Bakım Ünitesinde Sepsisli Çocuklarda Tanı İçin Tam Kan Sayımı Parametrelerinin Değerlendirilmesi Fatih Aygün1(İD), Cansu Durak1(İD), Fatih Varol1(İD), Haluk Çokuğraş2(İD), Yıldız Camcıoğlu2(İD), Halit Çam1(İD) 1 Department of Pediatric Intensive Care, Istanbul University School of Cerrahpasa Medicine, Istanbul, Turkey 2 Department of Pediatric Infectious Diseases, Istanbul University School of Cerrahpasa Medicine, Istanbul, Turkey Cite this article as: Aygün F, Durak C, Varol F, Çokuğraş H, Camcıoğlu Y, Çam H. Evaluation of complete blood count parameters for diagnosis in children with sepsis in the pediatric intensive care unit. J Pediatr Inf 2020;14(2):e55-e62. Abstract Öz Objective: Early diagnosis of sepsis is important for effective treatment Giriş: Erken tanı sepsiste etkili tedavi ve iyi prognoz için önemlidir. C-re- and improved prognosis. C-reactive protein (CRP) and procalcitonin aktif protein (CRP) ve prokalsitonin (PKT) sepsiste en sık kullanılan bi- (PCT) are the most commonly used biomarkers for sepsis. However, their yobelirteçlerdir. Fakat rutinde kullanımı maliyet etkin değildir. Tam kan routine usage is not cost-effective. Complete Blood Count (CBC) param- sayımı (TKS) parametrelerinden eritrosit dağılım genişliği (EDG), nötrofil eters including red cell distribution width (RDW), neutrophil to lympho- lenfosit oranı (NLO), trombosit lenfosit oranı (TLO), ortalama trombosit cyte ratios (NLR), platelet to lymphocyte ratios (PLR), mean platelet vol- hacmi (OTH) basit ve kolay olarak hesaplanmaktadır. Bu çalışmanın ama- ume (MPV), and hemoglobin are simple and easily calculated. -

Hemolytic Anemia Caused by Hereditary Pyruvate Kinase Deficiency in a West Highland White Terrier Dog
Arch Med Vet 44, 195-200 (2012) COMMUNICATION Hemolytic anemia caused by hereditary pyruvate kinase deficiency in a West Highland White Terrier dog Anemia hemolítica causada por la deficiencia de piruvato quinasa hereditaria en un perro West Highland White Terrier NRC Hlavaca, LA Lacerdaa*, FO Conradob, PS Hünninga, M Seibertc, FHD Gonzálezd, U Gigere aPostgraduate Program in Veterinary Sciences, Universidade Federal Rio Grande do Sul, Porto Alegre, RS, Brasil. bVeterinary Clinic Pathology, Universidade Federal Rio Grande do Sul, Porto Alegre, RS, Brasil. cClinic Pathology, PetLab Ltda, Porto Alegre, Brasil. dDepartment of Veterinary Clinic Pathology, Faculty of Veterinary, Universidade Federal Rio Grande do Sul, Porto Alegre, RS, Brasil. eLaboratory of Genetic Diseases, University of Pennsilvania, Philadelphia, United States. RESUMEN La deficiencia de piruvato quinasa (PK) es un desorden hemolítico autosómico recesivo descrito en perros y gatos. La piruvato quinasa es una de las enzimas regulatorias esenciales de la glicólisis anaeróbica, la deficiencia de esta enzima causa una destrucción prematura de los eritrocitos. El presente es un estudio de caso y relata los hallazgos clínicos y paraclínicos en un perro brasileño de la raza West Highland White Terrier (WHWT) con historia de debilidad e intolerancia al ejercicio. El paciente presentaba mucosas pálidas, anemia hemolítica bastante regenerativa y osteoclerosis. La deficiencia de PK fue confirmada a través de una prueba de ADN raza específica para la inserción 6bp en el extremo 3’ del exón 10 de la secuencia del gen de la piruvato quinasa eritrocitaria (R-PK) como fue descrito. Al perro se le practicó eutanasia a los 20 meses de edad debido al deterioro de su estado clínico, el cual incluyó anemia e incompatibilidad sanguínea.