BP503T UNIT-IV Topic: 1. Pharmacology Of
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Endocrine Drugs
PharmacologyPharmacologyPharmacology DrugsDrugs thatthat AffectAffect thethe EndocrineEndocrine SystemSystem TopicsTopicsTopics •• Pituitary Pituitary DrugsDrugs •• Parathyroid/Thyroid Parathyroid/Thyroid DrugsDrugs •• Adrenal Adrenal DrugsDrugs •• Pancreatic Pancreatic DrugsDrugs •• Reproductive Reproductive DrugsDrugs •• Sexual Sexual BehaviorBehavior DrugsDrugs FunctionsFunctionsFunctions •• Regulation Regulation •• Control Control GlandsGlandsGlands ExocrineExocrine EndocrineEndocrine •• Secrete Secrete enzymesenzymes •• Secrete Secrete hormoneshormones •• Close Close toto organsorgans •• Transport Transport viavia bloodstreambloodstream •• Require Require receptorsreceptors NervousNervous EndocrineEndocrine WiredWired WirelessWireless NeurotransmittersNeurotransmitters HormonesHormones ShortShort DistanceDistance LongLong Distance Distance ClosenessCloseness ReceptorReceptor Specificity Specificity RapidRapid OnsetOnset DelayedDelayed Onset Onset ShortShort DurationDuration ProlongedProlonged Duration Duration RapidRapid ResponseResponse RegulationRegulation MechanismMechanismMechanism ofofof ActionActionAction HypothalamusHypothalamusHypothalamus HypothalamicHypothalamicHypothalamic ControlControlControl PituitaryPituitaryPituitary PosteriorPosteriorPosterior PituitaryPituitaryPituitary Target Actions Oxytocin Uterus ↑ Contraction Mammary ↑ Milk let-down ADH Kidneys ↑ Water reabsorption AnteriorAnteriorAnterior PituitaryPituitaryPituitary Target Action GH Most tissue ↑ Growth TSH Thyroid ↑ TH secretion ACTH Adrenal ↑ Cortisol Cortex -

Vocabulario De Morfoloxía, Anatomía E Citoloxía Veterinaria
Vocabulario de Morfoloxía, anatomía e citoloxía veterinaria (galego-español-inglés) Servizo de Normalización Lingüística Universidade de Santiago de Compostela COLECCIÓN VOCABULARIOS TEMÁTICOS N.º 4 SERVIZO DE NORMALIZACIÓN LINGÜÍSTICA Vocabulario de Morfoloxía, anatomía e citoloxía veterinaria (galego-español-inglés) 2008 UNIVERSIDADE DE SANTIAGO DE COMPOSTELA VOCABULARIO de morfoloxía, anatomía e citoloxía veterinaria : (galego-español- inglés) / coordinador Xusto A. Rodríguez Río, Servizo de Normalización Lingüística ; autores Matilde Lombardero Fernández ... [et al.]. – Santiago de Compostela : Universidade de Santiago de Compostela, Servizo de Publicacións e Intercambio Científico, 2008. – 369 p. ; 21 cm. – (Vocabularios temáticos ; 4). - D.L. C 2458-2008. – ISBN 978-84-9887-018-3 1.Medicina �������������������������������������������������������������������������veterinaria-Diccionarios�������������������������������������������������. 2.Galego (Lingua)-Glosarios, vocabularios, etc. políglotas. I.Lombardero Fernández, Matilde. II.Rodríguez Rio, Xusto A. coord. III. Universidade de Santiago de Compostela. Servizo de Normalización Lingüística, coord. IV.Universidade de Santiago de Compostela. Servizo de Publicacións e Intercambio Científico, ed. V.Serie. 591.4(038)=699=60=20 Coordinador Xusto A. Rodríguez Río (Área de Terminoloxía. Servizo de Normalización Lingüística. Universidade de Santiago de Compostela) Autoras/res Matilde Lombardero Fernández (doutora en Veterinaria e profesora do Departamento de Anatomía e Produción Animal. -
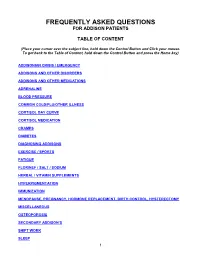
Frequently Asked Questions for Addison Patients
FREQUENTLY ASKED QUESTIONS FOR ADDISON PATIENTS TABLE OF CONTENT (Place your cursor over the subject line, hold down the Control Button and Click your mouse. To get back to the Table of Content, hold down the Control Button and press the Home key) ADDISONIAN CRISIS / EMERGENCY ADDISONS AND OTHER DISORDERS ADDISONS AND OTHER MEDICATIONS ADRENALINE BLOOD PRESSURE COMMON COLD/FLU/OTHER ILLNESS CORTISOL DAY CURVE CORTISOL MEDICATION CRAMPS DIABETES DIAGNOSING ADDISONS EXERCISE / SPORTS FATIGUE FLORINEF / SALT / SODIUM HERBAL / VITAMIN SUPPLEMENTS HYPERPIGMENTATION IMMUNIZATION MENOPAUSE, PREGNANCY, HORMONE REPLACEMENT, BIRTH CONTROL, HYSTERECTOMY MISCELLANEOUS OSTEOPOROSIS SECONDARY ADDISON’S SHIFT WORK SLEEP 1 STRESS DOSING SURGICAL, MEDICAL, DENTAL PROCEDURES THYROID TRAVEL WEIGHT GAIN 2 ADDISONIAN CRISIS / EMERGENCY How do you know when to call an ambulance? If you are careful, you should not have to call an ambulance. If someone with adrenal insufficiency has gastrointestinal problems and is unable to keep down their cortisol or other glucocorticoid for more than 24 hrs, they should be taken to an emergency department so they can be given intravenous solucortef and saline. It is not appropriate to wait until they are so ill that they cannot be taken to the hospital by a family member. If the individual is unable to retain anything by mouth and is very ill, or if they have had a sudden stress such as a fall or an infection, then it would be necessary for them to go by ambulance as soon as possible. It is important that you should have an emergency kit at home and that someone in the household knows how to use it. -

6. Endocrine System 6.1 - Drugs Used in Diabetes Also See SIGN 116: Management of Diabetes, 2010
1 6. Endocrine System 6.1 - Drugs used in Diabetes Also see SIGN 116: Management of Diabetes, 2010 http://www.sign.ac.uk/guidelines/fulltext/116 Insulin Prescribing Guidance in Type 2 Diabetes http://www.fifeadtc.scot.nhs.uk/media/6978/insulin-prescribing-in-type-2-diabetes.pdf 6.1.1 Insulins (Type 2 Diabetes) 6.1.1.1 Short Acting Insulins 1st Choice S – Insuman ® Rapid (Human Insulin) S – Humulin S ® S – Actrapid ® 2nd Choice S – Insulin Aspart (NovoRapid ®) (Insulin Analogues) S – Insulin Lispro (Humalog ®) 6.1.1.2 Intermediate and Long Acting Insulins 1st Choice S – Isophane Insulin (Insuman Basal ®) (Human Insulin) S – Isophane Insulin (Humulin I ®) S – Isophane Insulin (Insulatard ®) 2nd Choice S – Insulin Detemir (Levemir ®) (Insulin Analogues) S – Insulin Glargine (Lantus ®) Biphasic Insulins 1st Choice S – Biphasic Isophane (Human Insulin) (Insuman Comb ® ‘15’, ‘25’,’50’) S – Biphasic Isophane (Humulin M3 ®) 2nd Choice S – Biphasic Aspart (Novomix ® 30) (Insulin Analogues) S – Biphasic Lispro (Humalog ® Mix ‘25’ or ‘50’) Prescribing Points For patients with Type 1 diabetes, insulin will be initiated by a diabetes specialist with continuation of prescribing in primary care. Insulin analogues are the preferred insulins for use in Type 1 diabetes. Cartridge formulations of insulin are preferred to alternative formulations Type 2 patients who are newly prescribed insulin should usually be started on NPH isophane insulin, (e.g. Insuman Basal ®, Humulin I ®, Insulatard ®). Long-acting recombinant human insulin analogues (e.g. Levemir ®, Lantus ®) offer no significant clinical advantage for most type 2 patients and are much more expensive. In terms of human insulin. The Insuman ® range is currently the most cost-effective and preferred in new patients. -

Systolic Blood Pressure
Iatrogenic Cushing’s Syndrome secondary to the Combined Oral Contraceptive Pill in a patient with Congenital Adrenal Hyperplasia Satish Artham, Yaasir Mamoojee, Simon Ashwell. Department of Diabetes and Endocrinology, The James cook University Hospital, Middlesbrough, UK Introduction: Systolic blood pressure: Congenital Adrenal Hyperplasia (CAH) is a rare genetic disorder characterised by deficiency of cortisol and/or mineralocorticoid hormones with over production of sex steroids. 21-hydroxylase deficiency is the commonest cause of CAH accounting for 95% of cases1,2. Severe form of classic CAH occurs in 1 in 15,000 livebirths worldwide3,4. The goals of treating 21-hydroxylase deficiency in women is to replace the deficient steroid hormones, to lower the adrenal precursors and sex steroids. Most commonly used regimens are prednisolone once a day or hydrocortisone split into two or three doses. Case: Discussion: A 30 year old women with CAH diagnosed at birth was on replacement with hydrocortisone and fludrocortisone. She was investigated for ongoing diarrhoea Cortisol is the main glucocorticoid hormone, the majority of by the gastroenterologist and was subsequently diagnosed with Irritable Bowel which is circulated bound to Cortisol Binding Globulin (CBG). Syndrome (IBS). She was then started on buscopan and codeine phosphate for Only about 5% of the circulating cortisol is free. Cortisol action symptom relief. However during her menstrual cycle her abdominal symptoms is terminated by conversion into inactive forms by various were not sufficiently controlled. She was thus commenced on Microgynon, enzymes. It is mainly metabolised in the liver. It is reduced, a Combined Oral Contraceptive Pill (COCP). Within a year of initiation she oxidised and hydroxylated, the products of which are made developed cushingoid features, became hypertensive and started gaining weight. -

Us Anti-Doping Agency
2019U.S. ANTI-DOPING AGENCY WALLET CARDEXAMPLES OF PROHIBITED AND PERMITTED SUBSTANCES AND METHODS Effective Jan. 1 – Dec. 31, 2019 CATEGORIES OF SUBSTANCES PROHIBITED AT ALL TIMES (IN AND OUT-OF-COMPETITION) • Non-Approved Substances: investigational drugs and pharmaceuticals with no approval by a governmental regulatory health authority for human therapeutic use. • Anabolic Agents: androstenediol, androstenedione, bolasterone, boldenone, clenbuterol, danazol, desoxymethyltestosterone (madol), dehydrochlormethyltestosterone (DHCMT), Prasterone (dehydroepiandrosterone, DHEA , Intrarosa) and its prohormones, drostanolone, epitestosterone, methasterone, methyl-1-testosterone, methyltestosterone (Covaryx, EEMT, Est Estrogens-methyltest DS, Methitest), nandrolone, oxandrolone, prostanozol, Selective Androgen Receptor Modulators (enobosarm, (ostarine, MK-2866), andarine, LGD-4033, RAD-140). stanozolol, testosterone and its metabolites or isomers (Androgel), THG, tibolone, trenbolone, zeranol, zilpaterol, and similar substances. • Beta-2 Agonists: All selective and non-selective beta-2 agonists, including all optical isomers, are prohibited. Most inhaled beta-2 agonists are prohibited, including arformoterol (Brovana), fenoterol, higenamine (norcoclaurine, Tinospora crispa), indacaterol (Arcapta), levalbuterol (Xopenex), metaproternol (Alupent), orciprenaline, olodaterol (Striverdi), pirbuterol (Maxair), terbutaline (Brethaire), vilanterol (Breo). The only exceptions are albuterol, formoterol, and salmeterol by a metered-dose inhaler when used -

Steroid Use in Prednisone Allergy Abby Shuck, Pharmd Candidate
Steroid Use in Prednisone Allergy Abby Shuck, PharmD candidate 2015 University of Findlay If a patient has an allergy to prednisone and methylprednisolone, what (if any) other corticosteroid can the patient use to avoid an allergic reaction? Corticosteroids very rarely cause allergic reactions in patients that receive them. Since corticosteroids are typically used to treat severe allergic reactions and anaphylaxis, it seems unlikely that these drugs could actually induce an allergic reaction of their own. However, between 0.5-5% of people have reported any sort of reaction to a corticosteroid that they have received.1 Corticosteroids can cause anything from minor skin irritations to full blown anaphylactic shock. Worsening of allergic symptoms during corticosteroid treatment may not always mean that the patient has failed treatment, although it may appear to be so.2,3 There are essentially four classes of corticosteroids: Class A, hydrocortisone-type, Class B, triamcinolone acetonide type, Class C, betamethasone type, and Class D, hydrocortisone-17-butyrate and clobetasone-17-butyrate type. Major* corticosteroids in Class A include cortisone, hydrocortisone, methylprednisolone, prednisolone, and prednisone. Major* corticosteroids in Class B include budesonide, fluocinolone, and triamcinolone. Major* corticosteroids in Class C include beclomethasone and dexamethasone. Finally, major* corticosteroids in Class D include betamethasone, fluticasone, and mometasone.4,5 Class D was later subdivided into Class D1 and D2 depending on the presence or 5,6 absence of a C16 methyl substitution and/or halogenation on C9 of the steroid B-ring. It is often hard to determine what exactly a patient is allergic to if they experience a reaction to a corticosteroid. -

Advice for Patients Who Take Replacement Steroids (Hydrocortisone, Prednisolone, Dexamethasone Or Plenadren) for Pituitary/Adrenal Insufficiency
Advice for patients who take replacement steroids (hydrocortisone, prednisolone, dexamethasone or plenadren) for pituitary/adrenal insufficiency A number of you have been in touch looking for advice relating to the global coronavirus (also known as COVID-19) outbreak. If you are on steroid replacement therapy for pituitary or adrenal disease, or care for someone who is, and you’re worried about coronavirus, we’ve brought together a number of resources that we hope you will find useful. Coronavirus Adrenal Insufficiency Advice for Patients Primary adrenal insufficiency refers to all patients with loss of function of the adrenal itself, mostly either due to autoimmune Addison’s disease, or other causes such as congenital adrenal hyperplasia, bilateral adrenalectomy and adrenoleukodystrophy. The overwhelming majority of primary adrenal insufficiency patients suffer from both glucocorticoid and mineralocorticoid deficiency and usually take hydrocortisone (or prednisolone) and fludrocortisone. Our guidance similarly applies to patients with secondary adrenal insufficiency mostly due to pituitary tumours or previous high-dose glucocorticoid treatment. These patients take hydrocortisone for glucocorticoid deficiency As you will be aware it is important for patients with adrenal insufficiency to increase their steroids if unwell as per the usual sick day rules. Please ensure you have sufficient supplies to cover increased doses if you become unwell and an up to date emergency injection of hydrocortisone 100mg. Patients who suffer from a suspected or confirmed infection with coronavirus usually have high fever for many hours of the day, which results in the need for larger than usual steroid doses, so we advise slightly different sick day rules, which are listed below. -

Histology Histology
HISTOLOGY HISTOLOGY ОДЕСЬКИЙ НАЦІОНАЛЬНИЙ МЕДИЧНИЙ УНІВЕРСИТЕТ THE ODESSA NATIONAL MEDICAL UNIVERSITY Áiáëiîòåêà ñòóäåíòà-ìåäèêà Medical Student’s Library Серія заснована в 1999 р. на честь 100-річчя Одеського державного медичного університету (1900–2000 рр.) The series is initiated in 1999 to mark the Centenary of the Odessa State Medical University (1900–2000) 1 L. V. Arnautova O. A. Ulyantseva HISTÎLÎGY A course of lectures A manual Odessa The Odessa National Medical University 2011 UDC 616-018: 378.16 BBC 28.8я73 Series “Medical Student’s Library” Initiated in 1999 Authors: L. V. Arnautova, O. A. Ulyantseva Reviewers: Professor V. I. Shepitko, MD, the head of the Department of Histology, Cytology and Embryology of the Ukrainian Medical Stomatologic Academy Professor O. Yu. Shapovalova, MD, the head of the Department of Histology, Cytology and Embryology of the Crimean State Medical University named after S. I. Georgiyevsky It is published according to the decision of the Central Coordinational Methodical Committee of the Odessa National Medical University Proceedings N1 from 22.09.2010 Навчальний посібник містить лекції з гістології, цитології та ембріології у відповідності до програми. Викладено матеріали теоретичного курсу по всіх темах загальної та спеціальної гістології та ембріології. Посібник призначений для підготовки студентів до практичних занять та ліцензійного екзамену “Крок-1”. Arnautova L. V. Histology. A course of lectures : a manual / L. V. Arnautova, O. A. Ulyantseva. — Оdessa : The Оdessa National Medical University, 2010. — 336 p. — (Series “Medical Student’s Library”). ISBN 978-966-443-034-7 The manual contains the lecture course on histology, cytology and embryol- ogy in correspondence with the program. -

Pharmacology/Therapeutics II Block III Lectures 2013-14
Pharmacology/Therapeutics II Block III Lectures 2013‐14 66. Hypothalamic/pituitary Hormones ‐ Rana 67. Estrogens and Progesterone I ‐ Rana 68. Estrogens and Progesterone II ‐ Rana 69. Androgens ‐ Rana 70. Thyroid/Anti‐Thyroid Drugs – Patel 71. Calcium Metabolism – Patel 72. Adrenocorticosterioids and Antagonists – Clipstone 73. Diabetes Drugs I – Clipstone 74. Diabetes Drugs II ‐ Clipstone Pharmacology & Therapeutics Neuroendocrine Pharmacology: Hypothalamic and Pituitary Hormones, March 20, 2014 Lecture Ajay Rana, Ph.D. Neuroendocrine Pharmacology: Hypothalamic and Pituitary Hormones Date: Thursday, March 20, 2014-8:30 AM Reading Assignment: Katzung, Chapter 37 Key Concepts and Learning Objectives To review the physiology of neuroendocrine regulation To discuss the use neuroendocrine agents for the treatment of representative neuroendocrine disorders: growth hormone deficiency/excess, infertility, hyperprolactinemia Drugs discussed Growth Hormone Deficiency: . Recombinant hGH . Synthetic GHRH, Recombinant IGF-1 Growth Hormone Excess: . Somatostatin analogue . GH receptor antagonist . Dopamine receptor agonist Infertility and other endocrine related disorders: . Human menopausal and recombinant gonadotropins . GnRH agonists as activators . GnRH agonists as inhibitors . GnRH receptor antagonists Hyperprolactinemia: . Dopamine receptor agonists 1 Pharmacology & Therapeutics Neuroendocrine Pharmacology: Hypothalamic and Pituitary Hormones, March 20, 2014 Lecture Ajay Rana, Ph.D. 1. Overview of Neuroendocrine Systems The neuroendocrine -

Application of Prioritization Approaches to Optimize Environmental Monitoring and Testing of Pharmaceuticals
This is a repository copy of Application of prioritization approaches to optimize environmental monitoring and testing of pharmaceuticals. White Rose Research Online URL for this paper: https://eprints.whiterose.ac.uk/130449/ Article: Burns, Emily E orcid.org/0000-0003-4236-6409, Carter, Laura J, Snape, Jason R. et al. (2 more authors) (2018) Application of prioritization approaches to optimize environmental monitoring and testing of pharmaceuticals. Journal of Toxicology and Environmental Health, Part B: Critical Reviews. pp. 115-141. ISSN 1521-6950 https://doi.org/10.1080/10937404.2018.1465873 Reuse Items deposited in White Rose Research Online are protected by copyright, with all rights reserved unless indicated otherwise. They may be downloaded and/or printed for private study, or other acts as permitted by national copyright laws. The publisher or other rights holders may allow further reproduction and re-use of the full text version. This is indicated by the licence information on the White Rose Research Online record for the item. Takedown If you consider content in White Rose Research Online to be in breach of UK law, please notify us by emailing [email protected] including the URL of the record and the reason for the withdrawal request. [email protected] https://eprints.whiterose.ac.uk/ Application of prioritization approaches to optimize environmental monitoring and testing of pharmaceuticals Emily E. Burns,† Laura J. Cater,‡ Jason Snape,§ Jane Thomas-Oates,† Alistair B.A. Boxall*‡ †Chemistry Department, University of York, Heslington, YO10 5DD, United Kingdom ‡Environment Department, University of York, Heslington, YO10 5DD, United Kingdom §AstraZeneca UK, Global Safety, Health and Environment, Macclesfield, SK10 4TG, United Kingdom *Address correspondence to [email protected] Emily E. -

Observations on the Histology and Ultrastructure
OBSERVATIONS ON THE HISTOLOGY AND ULTRASTRUCTURE OF THE PARS DISTALIS OF THE RABBIT HYPOPHYSIS IN ORGAN CULTURE A Thesis submitted for the degree of Doctor of Philosophy in the University of London by SNEHLATA PATHAK Department of Cellular Biology 1970 and Histology, St. Mary's Hospital Medical School, London W.2. ABSTRACT The histology and ultrastrueture of the pars distalis of the rabbit hypophysis was studied after different periods of organ culture, and the best technique for the maintenance of the maximum proportion of the explant was assessed by comparing cultures grown in different conditions. Explants in air with a medium buffered. with N.2-hydroxyethylpiperazine-N1-2- ethanesulphonic acid (HEPES), not previously used in organ culture, proved more satisfactory than explants in carbogen with bicarbonate buffered 199, and cultures were maintained for more than 3 weeks. Material from young animals survived better than from old. The survival of cells was assessed on the basis of their cytological integrity when explants were examined by light microscopy after specific staining and by electron microscopy; DNA and RNA fluorescence with acridine orange was a valuable indicator. Also, cell multiplication was identified by direct observation of mitosis, by the application of the colchicine technique and by autoradiography. During culture, prolactin cells showed physiological signs of secretion (demonstrated by combined culture with mammary gland) and morphological signs of an increase of secretory activity. Morphological signs of reduced secretory activity appeared in the presence of hypothalamic tissue (combined culture) or extract. Somatotrophs and gonadotrophs. showed signs of low-level secretory activity in solitary pars distalis culture and of increased activity in combined culture with hypothalamus.