Endocrine Drugs
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-
Frequently Asked Questions for Addison Patients
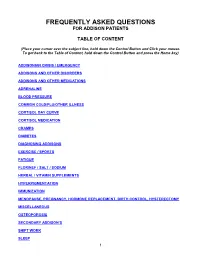
FREQUENTLY ASKED QUESTIONS FOR ADDISON PATIENTS TABLE OF CONTENT (Place your cursor over the subject line, hold down the Control Button and Click your mouse. To get back to the Table of Content, hold down the Control Button and press the Home key) ADDISONIAN CRISIS / EMERGENCY ADDISONS AND OTHER DISORDERS ADDISONS AND OTHER MEDICATIONS ADRENALINE BLOOD PRESSURE COMMON COLD/FLU/OTHER ILLNESS CORTISOL DAY CURVE CORTISOL MEDICATION CRAMPS DIABETES DIAGNOSING ADDISONS EXERCISE / SPORTS FATIGUE FLORINEF / SALT / SODIUM HERBAL / VITAMIN SUPPLEMENTS HYPERPIGMENTATION IMMUNIZATION MENOPAUSE, PREGNANCY, HORMONE REPLACEMENT, BIRTH CONTROL, HYSTERECTOMY MISCELLANEOUS OSTEOPOROSIS SECONDARY ADDISON’S SHIFT WORK SLEEP 1 STRESS DOSING SURGICAL, MEDICAL, DENTAL PROCEDURES THYROID TRAVEL WEIGHT GAIN 2 ADDISONIAN CRISIS / EMERGENCY How do you know when to call an ambulance? If you are careful, you should not have to call an ambulance. If someone with adrenal insufficiency has gastrointestinal problems and is unable to keep down their cortisol or other glucocorticoid for more than 24 hrs, they should be taken to an emergency department so they can be given intravenous solucortef and saline. It is not appropriate to wait until they are so ill that they cannot be taken to the hospital by a family member. If the individual is unable to retain anything by mouth and is very ill, or if they have had a sudden stress such as a fall or an infection, then it would be necessary for them to go by ambulance as soon as possible. It is important that you should have an emergency kit at home and that someone in the household knows how to use it. -

Effect of Chronic Treatment with Rosiglitazone on Leydig Cell Steroidogenesis in Rats
Couto et al. Reproductive Biology and Endocrinology 2010, 8:13 http://www.rbej.com/content/8/1/13 RESEARCH Open Access Effect of chronic treatment with Rosiglitazone on Leydig cell steroidogenesis in rats: In vivo and ex vivo studies Janaína A Couto1, Karina LA Saraiva2, Cleiton D Barros3, Daniel P Udrisar4, Christina A Peixoto2, Juliany SB César Vieira4, Maria C Lima3, Suely L Galdino3, Ivan R Pitta3, Maria I Wanderley4* Abstract Background: The present study was designed to examine the effect of chronic treatment with rosiglitazone - thiazolidinedione used in the treatment of type 2 diabetes mellitus for its insulin sensitizing effects - on the Leydig cell steroidogenic capacity and expression of the steroidogenic acute regulatory protein (StAR) and cholesterol side-chain cleavage enzyme (P450scc) in normal adult rats. Methods: Twelve adult male Wistar rats were treated with rosiglitazone (5 mg/kg) administered by gavage for 15 days. Twelve control animals were treated with the vehicle. The ability of rosiglitazone to directly affect the production of testosterone by Leydig cells ex vivo was evaluated using isolated Leydig cells from rosiglitazone- treated rats. Testosterone production was induced either by activators of the cAMP/PKA pathway (hCG and dbcAMP) or substrates of steroidogenesis [22(R)-hydroxy-cholesterol (22(R)-OH-C), which is a substrate for the P450scc enzyme, and pregnenolone, which is the product of the P450scc-catalyzed step]. Testosterone in plasma and in incubation medium was measured by radioimmunoassay. The StAR and P450scc expression was detected by immunocytochemistry. Results: The levels of total circulating testosterone were not altered by rosiglitazone treatment. A decrease in basal or induced testosterone production occurred in the Leydig cells of rosiglitazone-treated rats. -

6. Endocrine System 6.1 - Drugs Used in Diabetes Also See SIGN 116: Management of Diabetes, 2010
1 6. Endocrine System 6.1 - Drugs used in Diabetes Also see SIGN 116: Management of Diabetes, 2010 http://www.sign.ac.uk/guidelines/fulltext/116 Insulin Prescribing Guidance in Type 2 Diabetes http://www.fifeadtc.scot.nhs.uk/media/6978/insulin-prescribing-in-type-2-diabetes.pdf 6.1.1 Insulins (Type 2 Diabetes) 6.1.1.1 Short Acting Insulins 1st Choice S – Insuman ® Rapid (Human Insulin) S – Humulin S ® S – Actrapid ® 2nd Choice S – Insulin Aspart (NovoRapid ®) (Insulin Analogues) S – Insulin Lispro (Humalog ®) 6.1.1.2 Intermediate and Long Acting Insulins 1st Choice S – Isophane Insulin (Insuman Basal ®) (Human Insulin) S – Isophane Insulin (Humulin I ®) S – Isophane Insulin (Insulatard ®) 2nd Choice S – Insulin Detemir (Levemir ®) (Insulin Analogues) S – Insulin Glargine (Lantus ®) Biphasic Insulins 1st Choice S – Biphasic Isophane (Human Insulin) (Insuman Comb ® ‘15’, ‘25’,’50’) S – Biphasic Isophane (Humulin M3 ®) 2nd Choice S – Biphasic Aspart (Novomix ® 30) (Insulin Analogues) S – Biphasic Lispro (Humalog ® Mix ‘25’ or ‘50’) Prescribing Points For patients with Type 1 diabetes, insulin will be initiated by a diabetes specialist with continuation of prescribing in primary care. Insulin analogues are the preferred insulins for use in Type 1 diabetes. Cartridge formulations of insulin are preferred to alternative formulations Type 2 patients who are newly prescribed insulin should usually be started on NPH isophane insulin, (e.g. Insuman Basal ®, Humulin I ®, Insulatard ®). Long-acting recombinant human insulin analogues (e.g. Levemir ®, Lantus ®) offer no significant clinical advantage for most type 2 patients and are much more expensive. In terms of human insulin. The Insuman ® range is currently the most cost-effective and preferred in new patients. -

Systolic Blood Pressure
Iatrogenic Cushing’s Syndrome secondary to the Combined Oral Contraceptive Pill in a patient with Congenital Adrenal Hyperplasia Satish Artham, Yaasir Mamoojee, Simon Ashwell. Department of Diabetes and Endocrinology, The James cook University Hospital, Middlesbrough, UK Introduction: Systolic blood pressure: Congenital Adrenal Hyperplasia (CAH) is a rare genetic disorder characterised by deficiency of cortisol and/or mineralocorticoid hormones with over production of sex steroids. 21-hydroxylase deficiency is the commonest cause of CAH accounting for 95% of cases1,2. Severe form of classic CAH occurs in 1 in 15,000 livebirths worldwide3,4. The goals of treating 21-hydroxylase deficiency in women is to replace the deficient steroid hormones, to lower the adrenal precursors and sex steroids. Most commonly used regimens are prednisolone once a day or hydrocortisone split into two or three doses. Case: Discussion: A 30 year old women with CAH diagnosed at birth was on replacement with hydrocortisone and fludrocortisone. She was investigated for ongoing diarrhoea Cortisol is the main glucocorticoid hormone, the majority of by the gastroenterologist and was subsequently diagnosed with Irritable Bowel which is circulated bound to Cortisol Binding Globulin (CBG). Syndrome (IBS). She was then started on buscopan and codeine phosphate for Only about 5% of the circulating cortisol is free. Cortisol action symptom relief. However during her menstrual cycle her abdominal symptoms is terminated by conversion into inactive forms by various were not sufficiently controlled. She was thus commenced on Microgynon, enzymes. It is mainly metabolised in the liver. It is reduced, a Combined Oral Contraceptive Pill (COCP). Within a year of initiation she oxidised and hydroxylated, the products of which are made developed cushingoid features, became hypertensive and started gaining weight. -

Us Anti-Doping Agency
2019U.S. ANTI-DOPING AGENCY WALLET CARDEXAMPLES OF PROHIBITED AND PERMITTED SUBSTANCES AND METHODS Effective Jan. 1 – Dec. 31, 2019 CATEGORIES OF SUBSTANCES PROHIBITED AT ALL TIMES (IN AND OUT-OF-COMPETITION) • Non-Approved Substances: investigational drugs and pharmaceuticals with no approval by a governmental regulatory health authority for human therapeutic use. • Anabolic Agents: androstenediol, androstenedione, bolasterone, boldenone, clenbuterol, danazol, desoxymethyltestosterone (madol), dehydrochlormethyltestosterone (DHCMT), Prasterone (dehydroepiandrosterone, DHEA , Intrarosa) and its prohormones, drostanolone, epitestosterone, methasterone, methyl-1-testosterone, methyltestosterone (Covaryx, EEMT, Est Estrogens-methyltest DS, Methitest), nandrolone, oxandrolone, prostanozol, Selective Androgen Receptor Modulators (enobosarm, (ostarine, MK-2866), andarine, LGD-4033, RAD-140). stanozolol, testosterone and its metabolites or isomers (Androgel), THG, tibolone, trenbolone, zeranol, zilpaterol, and similar substances. • Beta-2 Agonists: All selective and non-selective beta-2 agonists, including all optical isomers, are prohibited. Most inhaled beta-2 agonists are prohibited, including arformoterol (Brovana), fenoterol, higenamine (norcoclaurine, Tinospora crispa), indacaterol (Arcapta), levalbuterol (Xopenex), metaproternol (Alupent), orciprenaline, olodaterol (Striverdi), pirbuterol (Maxair), terbutaline (Brethaire), vilanterol (Breo). The only exceptions are albuterol, formoterol, and salmeterol by a metered-dose inhaler when used -

Steroid Use in Prednisone Allergy Abby Shuck, Pharmd Candidate
Steroid Use in Prednisone Allergy Abby Shuck, PharmD candidate 2015 University of Findlay If a patient has an allergy to prednisone and methylprednisolone, what (if any) other corticosteroid can the patient use to avoid an allergic reaction? Corticosteroids very rarely cause allergic reactions in patients that receive them. Since corticosteroids are typically used to treat severe allergic reactions and anaphylaxis, it seems unlikely that these drugs could actually induce an allergic reaction of their own. However, between 0.5-5% of people have reported any sort of reaction to a corticosteroid that they have received.1 Corticosteroids can cause anything from minor skin irritations to full blown anaphylactic shock. Worsening of allergic symptoms during corticosteroid treatment may not always mean that the patient has failed treatment, although it may appear to be so.2,3 There are essentially four classes of corticosteroids: Class A, hydrocortisone-type, Class B, triamcinolone acetonide type, Class C, betamethasone type, and Class D, hydrocortisone-17-butyrate and clobetasone-17-butyrate type. Major* corticosteroids in Class A include cortisone, hydrocortisone, methylprednisolone, prednisolone, and prednisone. Major* corticosteroids in Class B include budesonide, fluocinolone, and triamcinolone. Major* corticosteroids in Class C include beclomethasone and dexamethasone. Finally, major* corticosteroids in Class D include betamethasone, fluticasone, and mometasone.4,5 Class D was later subdivided into Class D1 and D2 depending on the presence or 5,6 absence of a C16 methyl substitution and/or halogenation on C9 of the steroid B-ring. It is often hard to determine what exactly a patient is allergic to if they experience a reaction to a corticosteroid. -

AVANDIA® (Rosiglitazone Maleate) Tablets
PRESCRIBING INFORMATION AVANDIA® (rosiglitazone maleate) Tablets WARNING: CONGESTIVE HEART FAILURE ● Thiazolidinediones, including rosiglitazone, cause or exacerbate congestive heart failure in some patients (see WARNINGS). After initiation of AVANDIA, and after dose increases, observe patients carefully for signs and symptoms of heart failure (including excessive, rapid weight gain, dyspnea, and/or edema). If these signs and symptoms develop, the heart failure should be managed according to current standards of care. Furthermore, discontinuation or dose reduction of AVANDIA must be considered. ● AVANDIA is not recommended in patients with symptomatic heart failure. Initiation of AVANDIA in patients with established NYHA Class III or IV heart failure is contraindicated. (See CONTRAINDICATIONS and WARNINGS.) DESCRIPTION AVANDIA (rosiglitazone maleate) is an oral antidiabetic agent which acts primarily by increasing insulin sensitivity. AVANDIA is used in the management of type 2 diabetes mellitus (also known as non-insulin-dependent diabetes mellitus [NIDDM] or adult-onset diabetes). AVANDIA improves glycemic control while reducing circulating insulin levels. Pharmacological studies in animal models indicate that rosiglitazone improves sensitivity to insulin in muscle and adipose tissue and inhibits hepatic gluconeogenesis. Rosiglitazone maleate is not chemically or functionally related to the sulfonylureas, the biguanides, or the alpha-glucosidase inhibitors. Chemically, rosiglitazone maleate is (±)-5-[[4-[2-(methyl-2- pyridinylamino)ethoxy]phenyl]methyl]-2,4-thiazolidinedione, (Z)-2-butenedioate (1:1) with a molecular weight of 473.52 (357.44 free base). The molecule has a single chiral center and is present as a racemate. Due to rapid interconversion, the enantiomers are functionally indistinguishable. The structural formula of rosiglitazone maleate is: The molecular formula is C18H19N3O3S•C4H4O4. -

Inhibition of Mitochondrial Fatty Acid Oxidation in Drug-Induced Hepatic Steatosis*
Liver Research 3 (2019) 157e169 Contents lists available at ScienceDirect Liver Research journal homepage: http://www.keaipublishing.com/en/journals/liver-research Review Article Inhibition of mitochondrial fatty acid oxidation in drug-induced hepatic steatosis* Bernard Fromenty INSERM, UMR 1241, Universite de Rennes 1, Rennes, France article info abstract Article history: Mitochondrial fatty acid oxidation (mtFAO) is a key metabolic pathway required for energy production in Received 17 April 2019 the liver, in particular during periods of fasting. One major consequence of drug-induced impairment of Received in revised form mtFAO is hepatic steatosis, which is characterized by an accumulation of triglycerides and other lipid 16 May 2019 species, such as acyl-carnitines. Actually, the severity of this liver lesion is dependent on the residual Accepted 14 June 2019 mitochondrial b-oxidation flux. Indeed, a severe inhibition of mtFAO leads to microvesicular steatosis, hypoglycemia and liver failure. In contrast, moderate impairment of mtFAO can cause macrovacuolar Keywords: steatosis, which is a benign lesion in the short term. Because some drugs can induce both microvesicular Drug-induced liver injury (DILI) Steatosis and macrovacuolar steatosis, it is surmised that severe mitochondrial dysfunction could be favored in Mitochondria some patients by non-genetic factors (e.g., high doses and polymedication), or genetic predispositions b-Oxidation involving genes that encode proteins playing directly or indirectly a role in the mtFAO pathway. Example Acetaminophen (APAP) of drugs inducing steatosis include acetaminophen (APAP), amiodarone, ibuprofen, linezolid, nucleoside Troglitazone reverse transcriptase inhibitors, such as stavudine and didanosine, perhexiline, tamoxifen, tetracyclines, troglitazone and valproic acid. Because several previous articles reviewed in depth the mechanism(s) whereby most of these drugs are able to inhibit mtFAO and induce steatosis, the present review is rather focused on APAP, linezolid and troglitazone. -

Conjugated Estrogens Sustained Release Tablets) 0.3 Mg, 0.625 Mg, and 1.25 Mg
PRODUCT MONOGRAPH PrPREMARIN® (conjugated estrogens sustained release tablets) 0.3 mg, 0.625 mg, and 1.25 mg ESTROGENIC HORMONES ® Wyeth Canada Date of Revision: Pfizer Canada Inc., Licensee December 1, 2014 17,300 Trans-Canada Highway Kirkland, Quebec H9J 2M5 Submission Control No: 177429 PREMARIN (conjugated estrogens sustained release tablets) Page 1 of 46 Table of Contents PART I: HEALTH PROFESSIONAL INFORMATION .........................................................3 SUMMARY PRODUCT INFORMATION ...........................................................................3 INDICATIONS AND CLINICAL USE ................................................................................3 CONTRAINDICATIONS ......................................................................................................4 WARNINGS AND PRECAUTIONS ....................................................................................4 ADVERSE REACTIONS ....................................................................................................14 DRUG INTERACTIONS ....................................................................................................20 DOSAGE AND ADMINISTRATION ................................................................................23 OVERDOSAGE ...................................................................................................................25 ACTION AND CLINICAL PHARMACOLOGY ...............................................................25 STORAGE AND STABILITY ............................................................................................28 -

Guidance for Industry Drug-Induced Liver Injury: Premarketing Clinical Evaluation, Final, July 2009
Guidance for Industry Drug-Induced Liver Injury: Premarketing Clinical Evaluation U.S. Department of Health and Human Services Food and Drug Administration Center for Drug Evaluation and Research (CDER) Center for Biologics Evaluation and Research (CBER) July 2009 Drug Safety Guidance for Industry Drug-Induced Liver Injury: Premarketing Clinical Evaluation Additional copies are available from: Office of Communications, Division of Drug Information Center for Drug Evaluation and Research Food and Drug Administration 10903 New Hampshire Ave., Bldg. 51, rm. 2201 Silver Spring, MD 20993-0002 Tel: 301-796-3400; Fax: 301-847-8714; E-mail: [email protected] http://www.fda.gov/Drugs/GuidanceComplianceRegulatoryInformation/Guidances/default.htm or Office of Communication, Outreach, and Development, HFM-40 Center for Biologics Evaluation and Research Food and Drug Administration 1401 Rockville Pike, Rockville, MD 20852-1448 Tel: 800-835-4709 or 301-827-1800 http://www.fda.gov/BiologicsBloodVaccines/GuidanceComplianceRegulatoryInformation/Guidances/default.htm U.S. Department of Health and Human Services Food and Drug Administration Center for Drug Evaluation and Research (CDER) Center for Biologics Evaluation and Research (CBER) July 2009 Drug Safety TABLE OF CONTENTS I. INTRODUCTION............................................................................................................. 1 II. BACKGROUND: DILI ................................................................................................... 2 III. SIGNALS OF DILI AND HY’S -

Hepatobiliary Disposition of Troglitazone and Metabolites in Rat
0022-3565/10/3321-26–34$20.00 THE JOURNAL OF PHARMACOLOGY AND EXPERIMENTAL THERAPEUTICS Vol. 332, No. 1 Copyright © 2010 by The American Society for Pharmacology and Experimental Therapeutics 156653/3540910 JPET 332:26–34, 2010 Printed in U.S.A. Hepatobiliary Disposition of Troglitazone and Metabolites in Rat and Human Sandwich-Cultured Hepatocytes: Use of Monte Carlo Simulations to Assess the Impact of Changes in Biliary Excretion on Troglitazone Sulfate Accumulation Jin Kyung Lee, Tracy L. Marion, Koji Abe, Changwon Lim, Gary M. Pollock, and Kim L. R. Brouwer Division of Pharmacotherapy and Experimental Therapeutics, The University of North Carolina at Chapel Hill Eshelman School of Pharmacy, Chapel Hill, North Carolina (J.K.L., K.A., G.M.P., K.L.R.B.); Curriculum in Toxicology, School of Medicine, The University of North Carolina at Chapel Hill, Chapel Hill, North Carolina (T.L.M., G.M.P., K.L.R.B.); and Department of Statistics and Operations Research, College of Arts and Sciences, The University of North Carolina at Chapel Hill, Chapel Hill, North Carolina (C.L.) Received May 25, 2009; accepted October 1, 2009 ABSTRACT This study examined the hepatobiliary disposition of troglita- TS and TGZ concentrations ranged from 136 to 160 M and zone (TGZ) and metabolites [TGZ sulfate (TS), TGZ glucuronide from 49.4 to 84.7 M, respectively. Pharmacokinetic modeling (TG), and TGZ quinone (TQ)] over time in rat and human sand- and Monte Carlo simulations were used to evaluate the impact wich-cultured hepatocytes (SCH). Cells were incubated with of modulating the biliary excretion rate constant (Kbile) for TS on TGZ; samples were analyzed for TGZ and metabolites by liquid TS accumulation in hepatocytes and medium. -

Advice for Patients Who Take Replacement Steroids (Hydrocortisone, Prednisolone, Dexamethasone Or Plenadren) for Pituitary/Adrenal Insufficiency
Advice for patients who take replacement steroids (hydrocortisone, prednisolone, dexamethasone or plenadren) for pituitary/adrenal insufficiency A number of you have been in touch looking for advice relating to the global coronavirus (also known as COVID-19) outbreak. If you are on steroid replacement therapy for pituitary or adrenal disease, or care for someone who is, and you’re worried about coronavirus, we’ve brought together a number of resources that we hope you will find useful. Coronavirus Adrenal Insufficiency Advice for Patients Primary adrenal insufficiency refers to all patients with loss of function of the adrenal itself, mostly either due to autoimmune Addison’s disease, or other causes such as congenital adrenal hyperplasia, bilateral adrenalectomy and adrenoleukodystrophy. The overwhelming majority of primary adrenal insufficiency patients suffer from both glucocorticoid and mineralocorticoid deficiency and usually take hydrocortisone (or prednisolone) and fludrocortisone. Our guidance similarly applies to patients with secondary adrenal insufficiency mostly due to pituitary tumours or previous high-dose glucocorticoid treatment. These patients take hydrocortisone for glucocorticoid deficiency As you will be aware it is important for patients with adrenal insufficiency to increase their steroids if unwell as per the usual sick day rules. Please ensure you have sufficient supplies to cover increased doses if you become unwell and an up to date emergency injection of hydrocortisone 100mg. Patients who suffer from a suspected or confirmed infection with coronavirus usually have high fever for many hours of the day, which results in the need for larger than usual steroid doses, so we advise slightly different sick day rules, which are listed below.