Illustrated Clinical Anatomy, Second Edition
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Gross Anatomy
www.BookOfLinks.com THE BIG PICTURE GROSS ANATOMY www.BookOfLinks.com Notice Medicine is an ever-changing science. As new research and clinical experience broaden our knowledge, changes in treatment and drug therapy are required. The authors and the publisher of this work have checked with sources believed to be reliable in their efforts to provide information that is complete and generally in accord with the standards accepted at the time of publication. However, in view of the possibility of human error or changes in medical sciences, neither the authors nor the publisher nor any other party who has been involved in the preparation or publication of this work warrants that the information contained herein is in every respect accurate or complete, and they disclaim all responsibility for any errors or omissions or for the results obtained from use of the information contained in this work. Readers are encouraged to confirm the infor- mation contained herein with other sources. For example and in particular, readers are advised to check the product information sheet included in the package of each drug they plan to administer to be certain that the information contained in this work is accurate and that changes have not been made in the recommended dose or in the contraindications for administration. This recommendation is of particular importance in connection with new or infrequently used drugs. www.BookOfLinks.com THE BIG PICTURE GROSS ANATOMY David A. Morton, PhD Associate Professor Anatomy Director Department of Neurobiology and Anatomy University of Utah School of Medicine Salt Lake City, Utah K. Bo Foreman, PhD, PT Assistant Professor Anatomy Director University of Utah College of Health Salt Lake City, Utah Kurt H. -
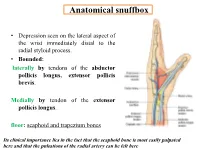
Anatomical Snuffbox
Anatomical snuffbox • Depression seen on the lateral aspect of the wrist immediately distal to the radial styloid process. • Bounded: laterally by tendons of the abductor pollicis longus, extensor pollicis brevis. Medially by tendon of the extensor pollicis longus. floor: scaphoid and trapezium bones Its clinical importance lies in the fact that the scaphoid bone is most easily palpated here and that the pulsations of the radial artery can be felt here Anatomical snuffbox Anatomical snuffbox • Contents: 2) Origin of the 1) The radial artery cephalic vein pass subcutaneously over the snuffbox. 3) Superficial branch of the radial nerve pass subcutaneously over the snuffbox. Blood supply of the hand Anastomoses occur between the radial and ulnar arteries via the superficial and deep palmar arches The Deep palmar arch is formed mainly by the radial artery while the superficial palmar arch is formed mainly by the ulnar artery 3-On entering the palm, it curves laterally behind (deep) the palmar 4-The arch is aponeurosis and in front completed on (superficial) of the long flexor the lateral side tendons forming by the the superficial palmar arch superficial branch of the radial artery. 2-Then it gives off its deep branch of which runs in front of the FR , and joins the radial artery to complete the deep palmar arch 1-Enters the hand anterior (superficial) to the Superficial flexor retinaculum palmar branch of radial artery through Guyon’s canal Radial artery 5-The superficial palmar arch gives off digital arteries from its convexity which pass to the fingers and supply them Superficial palmar arch Deep palmar branch of ulnar artery Superficial palmar branch of radial artery Ulnar artery Radial artery Radial Artery first dorsal interosseous muscle 1-From the floor of the anatomical snuff-box the radial artery leaves the dorsum of the hand by turning forward between the two heads of the first dorsal interosseous muscle. -

Comparative Anatomy of the Lower Respiratory Tract of the Gray Short-Tailed Opossum (Monodelphis Domestica) and North American Opossum (Didelphis Virginiana)
University of Tennessee, Knoxville TRACE: Tennessee Research and Creative Exchange Doctoral Dissertations Graduate School 12-2001 Comparative Anatomy of the Lower Respiratory Tract of the Gray Short-tailed Opossum (Monodelphis domestica) and North American Opossum (Didelphis virginiana) Lee Anne Cope University of Tennessee - Knoxville Follow this and additional works at: https://trace.tennessee.edu/utk_graddiss Part of the Animal Sciences Commons Recommended Citation Cope, Lee Anne, "Comparative Anatomy of the Lower Respiratory Tract of the Gray Short-tailed Opossum (Monodelphis domestica) and North American Opossum (Didelphis virginiana). " PhD diss., University of Tennessee, 2001. https://trace.tennessee.edu/utk_graddiss/2046 This Dissertation is brought to you for free and open access by the Graduate School at TRACE: Tennessee Research and Creative Exchange. It has been accepted for inclusion in Doctoral Dissertations by an authorized administrator of TRACE: Tennessee Research and Creative Exchange. For more information, please contact [email protected]. To the Graduate Council: I am submitting herewith a dissertation written by Lee Anne Cope entitled "Comparative Anatomy of the Lower Respiratory Tract of the Gray Short-tailed Opossum (Monodelphis domestica) and North American Opossum (Didelphis virginiana)." I have examined the final electronic copy of this dissertation for form and content and recommend that it be accepted in partial fulfillment of the equirr ements for the degree of Doctor of Philosophy, with a major in Animal Science. Robert W. Henry, Major Professor We have read this dissertation and recommend its acceptance: Dr. R.B. Reed, Dr. C. Mendis-Handagama, Dr. J. Schumacher, Dr. S.E. Orosz Accepted for the Council: Carolyn R. -

Redalyc.Accessory Hepatic Artery: Incidence and Distribution
Jornal Vascular Brasileiro ISSN: 1677-5449 [email protected] Sociedade Brasileira de Angiologia e de Cirurgia Vascular Brasil Dutta, Sukhendu; Mukerjee, Bimalendu Accessory hepatic artery: incidence and distribution Jornal Vascular Brasileiro, vol. 9, núm. 1, 2010, pp. 25-27 Sociedade Brasileira de Angiologia e de Cirurgia Vascular São Paulo, Brasil Available in: http://www.redalyc.org/articulo.oa?id=245016483014 How to cite Complete issue Scientific Information System More information about this article Network of Scientific Journals from Latin America, the Caribbean, Spain and Portugal Journal's homepage in redalyc.org Non-profit academic project, developed under the open access initiative ORIGINAL ARTICLE Accessory hepatic artery: incidence and distribution Artéria hepática acessória: incidência e distribuição Sukhendu Dutta,1 Bimalendu Mukerjee2 Abstract Resumo Background: Anatomic variations of the hepatic arteries are com- Contexto: As variações anatômicas das artérias hepáticas são co- mon. Preoperative identification of these variations is important to pre- muns. A identificação pré-operatória dessas variações é importante para vent inadvertent injury and potentially lethal complications during open prevenir lesão inadvertida e complicações potencialmente letais durante and endovascular procedures. procedimentos abertos e endovasculares. Objective: To evaluate the incidence, extra-hepatic course, and Objetivo: Avaliar a incidência, o trajeto extra-hepático e a presen- presence of side branches of accessory hepatic arteries, defined as an ad- ça de ramos laterais das artérias hepáticas acessórias definidas como um ditional arterial supply to the liver in the presence of normal hepatic ar- suprimento arterial adicional para o fígado na presença de artéria hepática tery. normal. Métodos: Oitenta e quatro cadáveres humanos masculinos foram Methods: Eighty-four human male cadavers were dissected using dissecados através de laparotomia mediana transperitoneal. -
Penile Circular Fasciocutaneous Flaps for Complex Anterior Urethral Strictures K.J
18 Penile Circular Fasciocutaneous Flaps for Complex Anterior Urethral Strictures K.J. Carney, J.W. McAninch 18.1 Penile Fascial Anatomy – 146 18.2 Flap Anatomy – 148 18.3 Patient Selection – 148 18.4 Preoperative Preparation – 148 18.5 Patient Positioning – 148 18.6 Flap Harvest – 149 18.7 Stricture Exposure – 150 18.8 Anastomosis – 151 18.9 Postoperative Care – 152 References – 152 146 Chapter 18 · Penile Circular Fasciocutaneous Flaps for Complex Anterior Urethral Strictures Surgical reconstruction of complex anterior urethral stric- Buck’s fascia is a well-defined fascial layer that is close- tures, 2.5–6 cm long, frequently requires tissue-transfer ly adherent to the tunica albuginea. Despite this intimate techniques [1–8]. The most successful are full-thickness association, a definite plane of cleavage exists between the free grafts (genital skin, bladder mucosa, or buccal muco- two, permitting separation and mobilization. Buck’s fascia sa) or pedicle-based flaps that carry a skin island. Of acts as the supporting layer, providing the foundation the latter, the penile circular fasciocutaneous flap, first for the circular fasciocutaneous penile flap. Dorsally, the described by McAninch in 1993 [9], produces excel- deep dorsal vein, dorsal arteries, and dorsal nerves lie in a lent cosmetic and functional results [10]. It is ideal for groove just deep to the superficial lamina of Buck’s fascia. reconstruction of the distal (pendulous) urethra, where The circumflex vessels branch from the dorsal vasculature the decreased substance of the corpus spongiosum may and lie just deep to Buck’s fascia over the lateral aspect jeopardize graft viability. -

Research Proposal
THE EFFECTS OF MINOCYCLINE ON SPINAL ROOT AVULSION INJURY IN RODENT MODEL: A HISTOLOGICAL STUDY By DR. TAN YEW CHIN MSurg Neurosurgery (Universiti Sains Malaysia) Dissertation Submitted in Partial Fulfillment of the Requirement for the Degree of Master of Surgery (Neurosurgery) UNIVERSITI SAINS MALAYSIA 2015 i Abstrak Pengenalan: Kecederaan saraf brakial adalah sesuatu kecederaan yang memudaratkan. Kecederaan tersebut melibatkan 5% kes-kes politrauma yang diakibatkan oleh kemalangan trafik. Matlamat utama rawatan kecederaan saraf brakial adalah pemulihan tenaga motor. Perawatan kecederaan saraf brakial secara pemindahan graf saraf boleh memberikan perlindungan kepada saraf motor. Namun begitu kesan rawatan pembedahan adalah sangat terhad. Rawatan secara perubatan perlu diberikan untuk mengekalkan fungsi yang wujud pada saraf motor. Minocycline sudah terbukti untuk membekalkan perlindungan kepada sel-sel saraf dalam penyakit angin ahmar dan penyakit pengelupasan selaput saraf. Minocycline adalah antibiotik yang mudah didapati, ekonomik, dan berupaya untuk merawat radangan dan kerosakan sel sel saraf. Literasi saintifik telah menunjukkan bahawa Minocycline berupaya untuk menghasilkan kesan perlindungan kepada sel-sel saraf motor dengan prencatan sel microglia dan Nitric Oxide Synthase. Kedua-dua kesan terapiutik ini dapat mengurangkan radangan dan degenerasi saraf setelah mendapat kecederaan ‘avulsion’ saraf brakial. Objektif: Kajian ini adalah untuk mengkaji kesan Minocycline yang selama ini digunakan sebagai antibiotik kepada hayat sel saraf motor dan juga penghasilan sel Microglia. Metodologi: Kajian eksperimental ini menggunakan tikus dewasa Sprague Dawley di mana urat saraf segmen C7 tikus ditarik sehingga putus daripada saraf tunjang. Transeksi fizikal ini akan dipastikan untuk berlaku sebelum ganglion saraf. Untuk mendapatkan validasi saintifik, saraf yang terputus telah diperhatikan di bawah ii Mikroskop untuk memastikan akar-akar saraf dicabut bersama-sama dengan tangkainya. -

Arterial Arcades of Pancreas and Their Variations Chavan NN*, Wabale RN**
International J. of Healthcare and Biomedical Research, Volume: 03, Issue: 02, January 2015, Pages 23-33 Original article: Arterial arcades of Pancreas and their variations Chavan NN*, Wabale RN** [*Assistant Professor, ** Professor and Head] Department of Anatomy, Rural Medical College, PIMS, Loni , Tal. Rahata, Dist. Ahmednagar, Maharashtra, Pin - 413736. Corresponding author: Dr Chavan NM Abstract: Introduction : Pancreas is a highly vascular organ supplied by number of arteries and arterial arcades which provide blood supply to the organ. Arteries contributing to the arterial arcades are celiac and superior mesenteric arteries forming anterior and posterior arcades. These vascular arcades lie upon the surface of the pancreas but also supply the duodenal wall and are the chief obstacles to complete pancreatectomy without duodenectomy. Knowledge of variations of upper abdominal arteries is important while dealing with gastric and duodenal ulcers, biliary tract surgeries and mobilization of the head of the pancreas, as bleeding is one of the complications of these surgeries. During pancreaticoduodenectomies or lymph node resection procedures, these arcades are liable to injuries. Material and methods : Study was conducted on 50 specimens of pancreas removed enbloc from cadavers to study variations in the arcade. Observation and result : Anterior arterial arcade was present in 98% specimens and absent in 2%. It was formed by anterior superior pancreaticoduodenal artery(ASPDA) and anterior inferior pancreaticoduodenal artery(AIPDA) in 92%, Anterior superior pancreaticoduodenal artery (ASPDA), Anterior inferior pancreaticoduodenal artery (AIPDA) and Right dorsal pancreatic artery (Rt.DPA) in 2%, Anterior superior pancreaticoduodenal artery (ASPDA) only in 2%, Anterior superior pancreaticoduodenal artery (ASPDA) and Posterior inferior pancreaticoduodenal artery (PIPDA) in 2%, Arcade was absent and Anterior superior pancreaticoduodenal artery (ASPDA) gave branches in 2%. -

E Pleura and Lungs
Bailey & Love · Essential Clinical Anatomy · Bailey & Love · Essential Clinical Anatomy Essential Clinical Anatomy · Bailey & Love · Essential Clinical Anatomy · Bailey & Love Bailey & Love · Essential Clinical Anatomy · Bailey & Love · EssentialChapter Clinical4 Anatomy e pleura and lungs • The pleura ............................................................................63 • MCQs .....................................................................................75 • The lungs .............................................................................64 • USMLE MCQs ....................................................................77 • Lymphatic drainage of the thorax ..............................70 • EMQs ......................................................................................77 • Autonomic nervous system ...........................................71 • Applied questions .............................................................78 THE PLEURA reections pass laterally behind the costal margin to reach the 8th rib in the midclavicular line and the 10th rib in the The pleura is a broelastic serous membrane lined by squa- midaxillary line, and along the 12th rib and the paravertebral mous epithelium forming a sac on each side of the chest. Each line (lying over the tips of the transverse processes, about 3 pleural sac is a closed cavity invaginated by a lung. Parietal cm from the midline). pleura lines the chest wall, and visceral (pulmonary) pleura Visceral pleura has no pain bres, but the parietal pleura covers -

Distal Radial Approach Through the Anatomical Snuff Box for Coronary Angiography and Percutaneous Coronary Intervention
Korean Circ J. 2018 Dec;48(12):1131-1134 https://doi.org/10.4070/kcj.2018.0293 pISSN 1738-5520·eISSN 1738-5555 Editorial Distal Radial Approach through the Anatomical Snuff Box for Coronary Angiography and Percutaneous Coronary Intervention Jae-Hyung Roh, MD, PhD, and Jae-Hwan Lee , MD, PhD Division of Cardiology, Department of Internal Medicine, Chungnam National University Hospital, Chungnam National University School of Medicine, Daejeon, Korea ► See the article “Feasibility of Coronary Angiography and Percutaneous Coronary Intervention via Left Snuffbox Approach” in volume 48 on page 1120. Received: Aug 27, 2018 The anatomical snuffbox, also known as the radial fossa, is a triangular-shaped depression Accepted: Sep 17, 2018 on the radial, dorsal aspect of the hand at the level of the carpal bones. It is clearly observed Figure 1 1)2) Correspondence to when the thumb is extended ( ). The bottom of the snuffbox is supported by carpal Jae-Hwan Lee, MD, PhD bones composed of the scaphoid and trapezium. The medial and lateral borders are bounded Division of Cardiology, Department of Internal by tendons of the extensor pollicis longus and the extensor pollicis brevis, respectively. The Medicine, Chungnam National University proximal border is formed by the styloid process of the radius. Within this narrow triangular Hospital, Chungnam National University space, various structures are located, including the distal radial artery (RA), a branch of the School of Medicine, 282, Munhwa-ro, Jung-gu, radial nerve, and the cephalic vein. Daejeon 35015, Korea. E-mail: [email protected] The anatomy of the hand arteries is illustrated in Figure 2. -

Ultrasound-Guided Access of the Distal Radial Artery at the Anatomical Snuffbox for Catheter-Based Vascular Interventions: a Technical Guide
Title: Ultrasound-guided access of the distal radial artery at the anatomical snuffbox for catheter-based vascular interventions: A technical guide. Authors: Anastasia Hadjivassiliou, MBBS, BSc; Ferdinand Kiemeneij, M.D, PhD; Sandeep Nathan, M.D, MSc; Darren Klass, M.D, PhD DOI: 10.4244/EIJ-D-19-00555 Citation: Hadjivassiliou A, Kiemeneij F, Nathan S, Klass D. Ultrasound-guided access of the distal radial artery at the anatomical snuffbox for catheter-based vascular interventions: A technical guide. EuroIntervention 2019; Jaa-625 2019, doi: 10.4244/EIJ-D-19-00555 Manuscript submission date: 10 June 2019 Revisions received: 24 July 2019 Accepted date: 01 August 2019 Online publication date: 06 August 2019 Disclaimer: This is a PDF file of a "Just accepted article". This PDF has been published online early without copy editing/typesetting as a service to the Journal's readership (having early access to this data). Copy editing/typesetting will commence shortly. Unforeseen errors may arise during the proofing process and as such Europa Digital & Publishing exercise their legal rights concerning these potential circumstances. Ultrasound-guided access of the distal radial artery at the anatomical snuffbox for catheter-based vascular interventions: A technical guide Anastasia Hadjivassiliou, MBBS, BSc1; Ferdinand Kiemeneij, MD, PhD2; Sandeep Nathan, MD, MSc3; Darren Klass, MD, PhD1 1. Department of Interventional Radiology, Vancouver General Hospital, University of British Columbia, Canada 2. Department of Cardiology, Tergooi Hospital, Blaricum, the Netherlands 3. University of Chicago Medicine, Chicago, IL, USA Short title: Ultrasound guided distal radial artery access at the anatomical snuffbox Corresponding author: Dr Darren Klass Department of Radiology, Vancouver General Hospital 899 West 12th Avenue, V5Z 1M9, Vancouver, BC, Canada Email address: [email protected] Disclaimer : As a public service to our readership, this article -- peer reviewed by the Editors of EuroIntervention - has been published immediately upon acceptance as it was received. -
Chapter 22 *Lecture Powerpoint
Chapter 22 *Lecture PowerPoint The Respiratory System *See separate FlexArt PowerPoint slides for all figures and tables preinserted into PowerPoint without notes. Copyright © The McGraw-Hill Companies, Inc. Permission required for reproduction or display. Introduction • Breathing represents life! – First breath of a newborn baby – Last gasp of a dying person • All body processes directly or indirectly require ATP – ATP synthesis requires oxygen and produces carbon dioxide – Drives the need to breathe to take in oxygen, and eliminate carbon dioxide 22-2 Anatomy of the Respiratory System • Expected Learning Outcomes – State the functions of the respiratory system – Name and describe the organs of this system – Trace the flow of air from the nose to the pulmonary alveoli – Relate the function of any portion of the respiratory tract to its gross and microscopic anatomy 22-3 Anatomy of the Respiratory System • The respiratory system consists of a system of tubes that delivers air to the lung – Oxygen diffuses into the blood, and carbon dioxide diffuses out • Respiratory and cardiovascular systems work together to deliver oxygen to the tissues and remove carbon dioxide – Considered jointly as cardiopulmonary system – Disorders of lungs directly effect the heart and vice versa • Respiratory system and the urinary system collaborate to regulate the body’s acid–base balance 22-4 Anatomy of the Respiratory System • Respiration has three meanings – Ventilation of the lungs (breathing) – The exchange of gases between the air and blood, and between blood and the tissue fluid – The use of oxygen in cellular metabolism 22-5 Anatomy of the Respiratory System • Functions – Provides O2 and CO2 exchange between blood and air – Serves for speech and other vocalizations – Provides the sense of smell – Affects pH of body fluids by eliminating CO2 22-6 Anatomy of the Respiratory System Cont. -

Latin Language and Medical Terminology
ODESSA NATIONAL MEDICAL UNIVERSITY Department of foreign languages Latin Language and medical terminology TextbookONMedU for 1st year students of medicine and dentistry Odessa 2018 Authors: Liubov Netrebchuk, Tamara Skuratova, Liubov Morar, Anastasiya Tsiba, Yelena Chaika ONMedU This manual is meant for foreign students studying the course “Latin and Medical Terminology” at Medical Faculty and Dentistry Faculty (the language of instruction: English). 3 Preface Textbook “Latin and Medical Terminology” is designed to be a comprehensive textbook covering the entire curriculum for medical students in this subject. The course “Latin and Medical Terminology” is a two-semester course that introduces students to the Latin and Greek medical terms that are commonly used in Medicine. The aim of the two-semester course is to achieve an active command of basic grammatical phenomena and rules with a special stress on the system of the language and on the specific character of medical terminology and promote further work with it. The textbook consists of three basic parts: 1. Anatomical Terminology: The primary rank is for anatomical nomenclature whose international version remains Latin in the full extent. Anatomical nomenclature is produced on base of the Latin language. Latin as a dead language does not develop and does not belong to any country or nation. It has a number of advantages that classical languages offer, its constancy, international character and neutrality. 2. Clinical Terminology: Clinical terminology represents a very interesting part of the Latin language. Many clinical terms came to English from Latin and people are used to their meanings and do not consider about their origin.