RS 2011 GE 44 SLB Eng.Pdf
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Mangroves Occurring on the Many Islands in the South Pacific Are Only a Small Component When Compared to the Worldwide Inventory of Mangroves
TECHNICAL ASSESSMENT AND SUPPORT FOR MANGROVE AND LITTORAL FOREST MANAGEMENT, PLANNING AND TRAINING FOR SMALL ISLANDS IN THE SOUTH PACIFIC Jan. 25, 2004 by James Denny Ward USDA Forest Service i FOREWORD Mangroves occurring on the many islands in the South Pacific are only a small component when compared to the worldwide inventory of mangroves. Although the mangroves found on the smaller islands may not seem as important on the global scale, they are extremely important to the small individual countries. Some of their benefits include shoreline protection, biodiversity, fisheries and a source for traditional products like building material, fuelwood and various cultural uses. These benefits are even more important to small island countries with limited resources and contributed to the survival of the indigenous people in earlier times. Realizing the importance of the mangrove resource the Forest & Trees Support Programme of SPC and the Heads of Forestry in the Pacific in cooperation with the USDA Forest Service conducted several missions during the last 10 years to assist the smaller island countries with preserving, protecting and managing their mangroves . The USDA Forest Service’s Institute of Pacific Islands Forestry based in Hawaii has been providing assistance to the Federated States of Micronesia and other islands with close ties to the United States for several years. Research conducted by this group has contributed greatly to the information base needed to manage mangroves throughout the South Pacific. This report is not all-inclusive but it is hoped that it will contain sufficient information to assist small islands in developing a management strategy for their individual countries. -

SOLOMON ISLANDS- EUROPEAN COMMUNITY Country Strategy
SOLOMON ISLANDS- EUROPEAN COMMUNITY Country Strategy Paper and National Indicative Programme for the period 2008- 2013 Page 1 of71 Solomon Islands EDFJO Country Strategy Paper The Government of the Solomon Islands and the European Commission hereby agrees as follows: (I) The Government of the Solomon Islands, represented by the Minister of Development Planning and Aid Coordination and National Authorising Officer, the Honourable Gordon Darcy Lilo, followed by the Honourable Steve Abana, and the European Commission, represented by Mr Aldo Dell'Ariccia, Head of the Commission Delegation to Solomon Islands, hereinafter referred to as the Parties, held discussions from March 2006 until August 2007 with a view to determining the general orientations for cooperation for the period 2008-2013. During these discussions, the Country Strategy Paper and an Indicative Programme of Community Aid in favour of the Solomon Islands were drawn up in accordance with the provisions of Articles 2 and 4 of Annex IV to the ACP-EC Partnership Agreement, signed in Cotonou on 23 June 2000 as revised in Luxemburg on 25 June 2005. These discussions complete the programming process in the Solomon Islands. The Country Strategy Paper and the Indicative Programme are annexed to the present document. (2) As regards the indicative programmable financial resources which the Community envisages to make available to the Solomon Islands for the period 2008-2013, an amount of € 13,2 million is foreseen for the allocation referred to in Article 3.2 (a) of Annex IV of the ACP-EC Partnership Agreement (A-allocation) and of€3,3 million for the allocation referred to in Article 3.2 (b) (B-allocation. -

Pacific Island Countries and Territories Issued: 19 February 2008
OCHA Regional Office for Asia Pacific Pacific Island Countries and Territories Issued: 19 February 2008 OCHA Presence in the Pacific Northern Papua New Guinea Fiji Mariana Humanitarian Affairs Unit (HAU), PNG Regional Disaster Response Islands (U.S.) UN House , Level 14, DeloitteTower, Advisor (RDRA), Fiji Douglas Street, PO Box 1041, 360 Victoria Parade, 3rd Floor Fiji +10 Port Moresby, Papua New Guinea Development Bank Building, Suva, FIJI Tel: +675 321 2877 Tel: +679 331 6760, +679 331 6761 International Date Line Fax: +675 321 1224 Fax: +679 330 9762 Saipan Email: [email protected] Email: [email protected] Head: Vini Talai Head: Peter Muller Agana +12 Guam (U.S.) Pacific Ocean +10 MARSHALL ISLANDS Legend Depth (m) OCHA Presence Below 5,000 1,001 to 2,000 MICRONESIA (FSO) Koror Majuro Country capital Palikir 4,001 to 5,000 501 to 1,000 Territory capital PALAU +11 Illustrative boundary 3,001 to 4,000 101 to 500 +9 +10 Time difference with UTC 2,001 to 3,000 o to 100 Tarawa (New York: UTC -5 Equator NAURU Geneva: UTC +1) IMPORTANT NOTE: The boundaries on this map are for illustrative purposes only Yaren Naming Convention and were derived from the map ’The +12 +12 KIRIBATI UN MEMBER STATE Pacific Islands’ published in 2004 by the Territory or Associated State Secretariat of the Pacific Community. INDONESIA TUVALU -11 -10 PAPUA NEW GUINEA United Nations Office for the Coordination +10 +12 of Humanitarian affairs (OCHA) Funafuti Toke lau (N.Z.) Regional Office for Asia Pacific (ROAP) Honiara Executive Suite, 2nd Floor, -10 UNCC Building, -
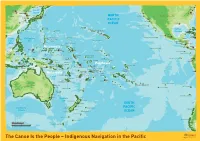
Indigenous Navigation in the Pacific
Hokkaido Vladivostok New York Philadelphia Beijing North Korea Sea of Tianjin Japan P'yongyang Sacramento Washington Seoul Japan Honshu NORTH San Francisco United States of America China South Tokyo Nagoya Korea Pusan Osaka Los Angeles PACIFIC Cheju-Do Shikoku San Diego Shanghai Kyushu OCEAN New Orleans Guadalupe Island (Mex.) Midway Baja Ryukyu Ogasawara- Islands (US) California Trench Okinawa-Jima (Jap.) Gunto (Jap.) Gulf of Miami Minami-Tori- Hawaiian Islands (US) Shima (Jap.) Mexico Havana Taiwan Kauai Cuba Oahu Mexico Hainan Dao Honolulu Guadalajara Jamaica Mariana Mexico Northern Wake Island (US) Hawaii Revillagigedo Island (Mex.) Kingston Philippine Ridge Belize South Luzon Mariana Islands Johnston Atoll (US) China Sea (US) Guatemala Honduras Manila Saipan Sea Guam (US) Marshall Islands El Salvador Nicaragua Philippines Enewetak Managua Costa Rica Panama Yap Islands Micronesia San José Palawan Ratak Clipperton Island (Fr.) Mindanao Pohnpei Chain Davao Melekeok Satawai Panama Chuuk Palikir Majuro Palmyra Atoll (US) Ralik Cocos Islands (CR) Brunei Palau Kosrae Chain Malaysia Line Malpelo Island (Col.) Federated States of Micronesia Gilbert Islands Howland Island (US) Islands Colombia Halmahera Kalimantan Tarawa Baker Island (US) Bismarck Archipelago Quito Jarvis Island (US) Galapagos Islands (Ec.) Sulawesi New Ireland Nauru Guayaquil Phoenix Islands Kiribati Malden Rabaul Ecuador Seram New Guinea Papua Bougainville Solomon Nanumea Vaiaku Indonesia New Guinea New Britain Santa Isabel Islands Polynesia Surabaya Funafuti Marquesas Islands -

Solomon Islands B ! Fagani C D ! Waimapuru ! ! Solomon Sea Mainga Tawani Vanuatu ! ! Rennel Island Manakia
FRAME B 155°E 160°E Rorovana ! ! ! Torokina Panguna Karakun Koiaris ! ! Papua New Guin! ea Taki ! ! Jaba Sininai ! Pupuku PACIFIC OCEAN Aitara ! ! ! Kaekui Mission ! Birambira ! Tokuaka Susuka !Kombokisa !! Kutakana Lukuvaru Shortland Island PACIFIC OCEAN ! ! Ghaomai Choiseul Zambanarungga Shortland I ! ! Vure ! Trevanion Noka ! ! Mono I Matamotu ! ! ! Masoko Java Malemgeulu ! ! Paraso ! Zuzuao Santa Cruz Islands Apakhö ! ! ! Point Lunga ! Eleoteve Arambu Filuo Vana!! ! ! Litoghahira Sambora Santa Isabel Island FRAME D Kolomb!angara! Ganongga ! New Georgia Islands ! Tapurai Tuarugu ! Biluro ! ! Mburuku Loalonga ! Lokiha ! ! ! Sepi ! Ageraba Harai Mbareho ! Fokinkorra ! S o l o m o n I s l a n d s Auki Kunura ! ! Kwaimbaambaala ! Vura Nggaulai'ato'o ! ! ! Siota !! Manikiriu Tulagi Paunairo Vatupilei ! ! Palikir Abungari !. Koror !. Marshall Islands Malaita Palau Guranja Honiara Micronesia Hularu ! ! .! !Gembua ! Guadalcanal Rere ! Kiribati ! ! PACIFIC OCEAN Solomon Sea Mbaole ! Sitaronda Ahenawai Anoni'usu Nauru Ralavu Raurembo ! Mwarada ! ! ! Ione ! Lakatana ! Ahia I n d o n e s i a Makina 10°S Papua New 10°S Guinea Solomon Sea Honiara Heuru !. Port Moresby !. ! Etamarorai Solomon Islands B ! Fagani C D ! Waimapuru ! ! Solomon Sea Mainga Tawani Vanuatu ! ! Rennel Island Manakia !.Port-Vila ! San Cristobal Australia Vinegau ! New Caledonia Na Wosi ! Funakumwa ! ! !. Hauraha Nouméa FRAME A Napasiwai FRAME C 155°E 160°E Date Created: 04- JUL - 2011 Map Num: LogCluster_SLB_LCA_004 Kilometers .! National Capital Road Network National Boundary Coord.System/Datum: Geographic/WGS84 S O L O M O N GLIDE Num: ! Village (selection) Secondary Surface Waterbody The boundaries and names and the designations 0 50 100 150 200 used on this map do not imply official endorsement I S L A N D S FRAME A Nominal Scale 1:62,420,000 at A4 Tertiary or acceptance by the United Nations. -

Political Reviews
Political Reviews The Region in Review: International Issues and Events, 2017 nic maclellan Melanesia in Review: Issues and Events, 2017 volker boege, mathias chauchat, alumita durutalo, joseph daniel foukona, budi hernawan, michael leach, james stiefvater The Contemporary Pacic, Volume 30, Number 2, 461–547 © 2018 by University of Hawai‘i Press 461 political reviews • melanesia 531 ville. 6 April. https://www.economist.com/ early in the year, revealing that the news/asia/21720327-first-pacific-island country was experiencing cash flow -may-choose-stay-part-france-second problems due to financial mismanage- -could-split-papua [accessed 6 Feb 2018] ment (Aatai 2017a). It was alleged by The National. 2017a. Micah Vows to former Prime Minister Gordon Darcy Cancel apec. 31 May. https://www Lilo that the government’s reserve .thenational.com.pg/micah-vows-cancel had been reduced within two years -apec/ [accessed 6 Feb 2018] from si$1.5 billion to si$150 million ———. 2017b Polye Pledges to Help (si$100 = us$12.63). As a result, the B’ville Gain Independence. 19 May. government had to borrow to pay its https://www.thenational.com.pg/polye bills and settle other financial com- -pledges-help-bville-gain-independence/ mitments (sibc 2017b). Minister of [accessed 6 Feb 2018] Finance Snyder Rini assured the gen- Tlozek, Erik. 2017. Papua New Guinea eral public that government finances Loses UN Vote over Unpaid Annual Con- were stable and under control. This tributions. abc News (Australia), 23 Feb. was contrary to the government’s http://www.abc.net.au/news/2017-02-24/ actual financial performance through- papua-new-guinea-loses-un-vote-over out the year because the government -unpaid-contributions/8298486 continued to delay the payment of [accessed 13 Feb 2018] bills and meeting its financial com- Vari, Mathew. -

Micronesian Art Historical Research and Library Collection Resources in Micronesia
DOCUMENT RESUME ED 377 132 SO 024 616 AUTHOR Haynes, Douglas TITLE Micronesian Art Historical Research and Library Collection Resources in Micronesia. PUB DATE Nov 91 NOTE 9p.; Paper presented to the Art Education Delegation Exchange (Beijing, China, November 1991). PUB TYPE Reference Materials General (130) EDRS PRICE MF01/PC01 Plus Postage. DESCRIPTORS Architecture; Archives; *Art History; Foreign Countries; Higher Education; *Library Collections; *Non Western Civilization IDENTIFIERS Micronesia ABSTRACT This paper briefly describes the geographic region and some indigenous artifacts of Micronesia. The state of art historical research in the area and currently available library resources are discussed. Micronesia is comprised of seven island nations peopled by distinctly unique cultural groups. Study of Micronesian art and architecture is relatively recent. Early work was done by German, then Japanese, expeditions. More recently, Americans, as well as European and Japanese researchers, have studied the art and cultures of Micronesia. Among art forms studied are latte stones, dating from 1000 A.D. to 1668 A.D. These were hand smoothed and fitted limestone columns and capstones used to construct A-frame houses for the Chamorros, a people of the Mariana Islands group. The bai, a communal village house of Palau, is decorated with sculpture:, expressing a complex iconography of mythological symbolism. Another architectural accomplishment of Micronesians are the stone cities of Pohnpei and Kosrae, dating from the 8th-9th centuries to 1830. The largest collection of Micronesian art history materials available in the islands is the collection at the University of Guam (Mangilao). Other collections are located in the Pal=su National Museum Library in Koror, Palau; the Community College of Micronesia Pacific Collection in Kolonia, Pohnpei; The Nieves Flores Public Library in Agana, Guam; and the Federated States of Micronesia National Archives in Palikir, Pohnpe. -
University of Auckland Research Repository, Researchspace
Libraries and Learning Services University of Auckland Research Repository, ResearchSpace Copyright Statement The digital copy of this thesis is protected by the Copyright Act 1994 (New Zealand). This thesis may be consulted by you, provided you comply with the provisions of the Act and the following conditions of use: • Any use you make of these documents or images must be for research or private study purposes only, and you may not make them available to any other person. • Authors control the copyright of their thesis. You will recognize the author's right to be identified as the author of this thesis, and due acknowledgement will be made to the author where appropriate. • You will obtain the author's permission before publishing any material from their thesis. General copyright and disclaimer In addition to the above conditions, authors give their consent for the digital copy of their work to be used subject to the conditions specified on the Library Thesis Consent Form and Deposit Licence. Community Participation and NGO Responses to the April 2014 Floods in Solomon Islands Carl Adams A thesis submitted in complete fulfillment of the requirements for the degree of Master of Arts in Development Studies, The University of Auckland, 2016. P a g e | I Abstract Floods are the most common form of natural disasters globally, disproportionately impacting lower income countries and in many cases the poorest citizens therein. The increasing frequency and intensity of floods present civil society, policymakers, and development practitioners the challenge of reducing disaster risk, and populations’ vulnerability to extreme weather events. This thesis explores the roles of affected communities in Non-Governmental Organisation (NGO) responses to disaster in Solomon Islands, based on the experience of the 2014 flash floods. -

View Profile
Solomon Islands KEY FACTS Joined Commonwealth: 1978 Population: 561,000 (2013) GDP p.c. growth: 0.5% p.a. 1990–2013 UN HDI 2014: World ranking 157 Official language: English Time: GMT plus 11 hrs Currency: Solomon Islands dollar (SI$) Geography Area: 28,370 sq km Coastline: 5,310 km Capital: Honiara Solomon Islands, an archipelago in the south- west Pacific, consists of a double chain of There are large tracts of rough grass on the islands. The international airport is at rocky islands and some small coral islands. northern side of Guadalcanal and Nggela Henderson Field, 13 km east of Honiara. The major islands are Guadalcanal, Choiseul, Sule. Parts of the coast are swampy, Santa Isabel, New Georgia, Malaita and supporting extensive mangrove forests. Society Elsewhere, the coast is dominated by coconut Makira (or San Cristobal). Vanuatu is the KEY FACTS 2013 nearest neighbour to the south-east where palms. Hardwoods now grown for timber the archipelago tapers off into a series of include mahogany, acacia and teak. Population per sq km: 20 smaller islands. Its nearest neighbour to the Wildlife: Indigenous mammals are small and Life expectancy: 68 years west is Papua New Guinea. include opossums, bats and mice. There are Net primary enrolment: 93% crocodiles in the mangrove swamps and sea The country comprises the capital territory of Population: 561,000 (2013); 21 per cent of turtles nest on the shores from November to Honiara and nine provinces, namely Central people live in urban areas; growth 2.6 per February. Birdlife (more than 150 species) (provincial capital Tulagi), Choiseul (Taro cent p.a. -

Report of the Australian Parliamentary Delegation to Solomon Islands and Samoa 31 July–11 August 2011
1 The Parliament of the Commonwealth of Australia Report of the Australian Parliamentary Delegation to Solomon Islands and Samoa 31 July–11 August 2011 July 2012 2 TABLE OF CONTENTS Membership of the Delegation ................................................................................ 4 PREFACE ................................................................................................................. 5 Chapter 1.............................................................................................................. 7 Introduction ............................................................................................................ 7 Acknowledgements ................................................................................................ 9 Chapter 2: Solomon Islands ............................................................................. 10 Overview of bilateral relations .............................................................................. 10 Details of meetings ............................................................................................... 11 The Parliament ................................................................................................... 11 RAMSI .............................................................................................................. 12 National Referral Hospital ................................................................................. 13 Visit to Gizo (Western Province) ..................................................................... -

Solomon Island Election Results: 2014
Solomon Island Election Results: 2014 Province Electorate Candidate Party Vote % Vote Winner Incumbent Central Province Nggela Bartholomew Parapolo Independent 2094 24.6% * Janet R Hatimoana United Democratic Party 1649 19.4% Frederick Noel Charles Douglas Independent 1346 15.8% Henry Zimbo Independent 1273 15.0% Mark Roboliu Kemakeza Independent 449 5.3% Philip Ashley Soboi Independent 403 4.7% Christian Salini People's Alliance Party 365 4.3% David Harper Independent 300 3.5% Elijah Taikole Independent 274 3.2% Stillwest Longden Kadere Party of Solomon Islands 143 1.7% Leonard Vetena Williams Independent 66 0.8% Ellison Bai Animamu Independent 53 0.6% David Kwan Independent 30 0.4% Isa'ac Kito Seko Independent 25 0.3% Rejected Votes 25 0.3% Nggela Total 8495 100.0% Russells/Savo Dickson Mua Panakitasi Independent 3189 52.8% * * Oliver Salopuka Kadere Party of Solomon Islands 1261 20.9% Allan Kemakeza United Democratic Party 1225 20.3% Aenasi Diosi Independent 136 2.2% Godfrey Narasia Solomon Islands People First Party 112 1.9% Leslie Norris Asad People's Alliance Party 60 1.0% Rejected Votes 17 0.3% Walter Ben Turasi Youth Owned Rural and Urban Party 16 0.3% Constantine Sekudo Independent 15 0.2% John Quan Independent 14 0.2% Russells/Savo Total 6045 100.0% Choiseul Province East Choiseul Mannaseh Sogavare Independent 1596 63.1% * * Ronald Pitamama Democratic Alliance Party 602 23.8% James Ron Kaboke Solomon Islands People First Party 320 12.6% Rejected Votes 12 0.5% East Choiseul Total 2530 100.0% North West Choiseul Connelly Sadakabatu -

Symbol BP Order Ninamo OTUANA Frigate Bird 1 Independent
NOMINATIONS WESTERN PROVINCE Shortlands (4) Symbol BP Order Ninamo OTUANA Frigate Bird 1 Independent George TAYLOR Lamp/Lantern 2 Independent Brisbane AMATORE Party Symbol 3 United Democratic Party Derick PAKO Key (1) 4 Independent Pellion BUARE Party Symbol 5 People's Alliance Party Christopher LAORE Axe 6 Independent NOMINATIONS WESTERN PROVINCE North Vella La Vella (5) Symbol BP Order Clezy RORE Bonito Fish 1 Independent Pye Roberts KUVE Party Symbol 2 United Democratic Party Milner TOZAKA Party Symbol 3 People's Alliance Party Jennings MOVOBULE Party Symbol 4 Kadere Party of solomon Islands NOMINATIONS WESTERN PROVINCE South Vella La Vella (6) Symbol BP Order Qora Alex LIONAL Tree 1 Independent Rence SORE Party Symbol 2 National Transformation Party Christian MESEPITU Party Symbol 3 United Democratic Party NOMINATIONS WESTERN PROVINCE Rannogga/Simbo (7) Symbol BP Order Winson TIGULU Party Symbol 1 United Democratic Party Charles SIGOTO Lamp/Lantern 2 Independent Joi Steven BATO Party Symbol 3 Solomon Islands People First Party Hampton BEKEPIO Party Symbol 4 Pan-Melanesian Congress Party Gideon TUKE Party Symbol 5 National Transformation Party Francis Billy HILLY Ship (Cutter Boat) 6 Independent Jimmy STANLEY Sailing Fish 7 Independent Mairy KOTOMAE Party Symbol 8 People's Alliance Party NOMINATIONS WESTERN PROVINCE Gizo/Kolombangara (8) Symbol BP Order Schulte MAETOLOA War Canoe 1 Independent Gordon Darcy LILO Party Symbol 2 Solomon Islands Party for Rural Advancement Kenneth BULEHITE Ship (Cutter Boat) 3 Independent Jimson Fiau TANANGADA