A Parent's Guide – a Guide to Living With
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-
Appendix V; Revised 2/28/06
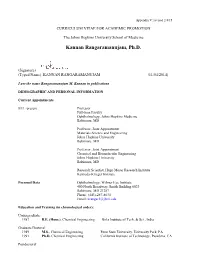
Appendix V; revised 2/4/15 CURRICULUM VITAE FOR ACADEMIC PROMOTION The Johns Hopkins University School of Medicine Kannan Rangaramanujam, Ph.D. (Signature) (Typed Name) KANNAN RANGARAMANUJAM (11/04/2014) I use the name Rangaramanujam M. Kannan in publications DEMOGRAPHIC AND PERSONAL INFORMATION Current Appointments 8/11 -present Professor Full-time Faculty Ophthalmology, Johns Hopkins Medicine Baltimore, MD Professor, Joint Appointment Materials Science and Engineering Johns Hopkins University Baltimore, MD Professor, Joint Appointment Chemical and Biomolecular Engineering Johns Hopkins University Baltimore, MD Research Scientist, Hugo Moser Research Institute Kennedy-Krieger Institute Personal Data Ophthalmology, Wilmer Eye Institute 400 North Broadway, Smith Building 6023 Baltimore, MD 21287 Phone: (443)-287-8634 Email: [email protected] Education and Training (in chronological order): Undergraduate: 1987 B.E. (Hons.), Chemical Engineering Birla Institute of Tech. & Sci., India Graduate/Doctoral: 1989 M.S., Chemical Engineering Penn State University, University Park, PA 1991 Ph.D. Chemical Engineering California Institute of Technology, Pasadena, CA Postdoctoral: 8/94 – 7/95 Fellow Chemistry/Chem. Engg. University of Minnesota, Minneapolis, MN Professional Experience (in chronological order, earliest first) 8/95 - 7/97 Senior Research Engineer, 3M Corporate Research, St. Paul, MN 8/97 - 5/03 Assistant Professor, Chemical Engineering, Wayne State University, Detroit, MI 5/02 - 7/11 Assistant Professor, Biomedical Engineering, Wayne -

Robert Lehman Papers
Robert Lehman papers Finding aid prepared by Larry Weimer The Robert Lehman Collection Archival Project was generously funded by the Robert Lehman Foundation, Inc. This finding aid was generated using Archivists' Toolkit on September 24, 2014 Robert Lehman Collection The Metropolitan Museum of Art 1000 Fifth Avenue New York, NY, 10028 [email protected] Robert Lehman papers Table of Contents Summary Information .......................................................................................................3 Biographical/Historical note................................................................................................4 Scope and Contents note...................................................................................................34 Arrangement note.............................................................................................................. 36 Administrative Information ............................................................................................ 37 Related Materials ............................................................................................................ 39 Controlled Access Headings............................................................................................. 41 Bibliography...................................................................................................................... 40 Collection Inventory..........................................................................................................43 Series I. General -

Linked Adrenoleukodystrophy: Pathology, Pathophysiology, Diagnostic Testing, Newborn Screening and Therapies
Received: 21 May 2019 | Accepted: 21 November 2019 DOI: 10.1002/jdn.10003 RESEARCH ARTICLE X-linked adrenoleukodystrophy: Pathology, pathophysiology, diagnostic testing, newborn screening and therapies Bela R. Turk1 | Christiane Theda2 | Ali Fatemi1 | Ann B. Moser1 1Hugo W Moser Research Institute, Kennedy Krieger Institute, Baltimore, MD, USA 2Neonatal Services, Royal Women's Hospital, Murdoch Children's Research Institute and University of Melbourne, Melbourne, VIC, Australia Correspondence Ann B. Moser, Hugo W Moser Research Abstract Institute, Kennedy Krieger Institute, 707 N. Adrenoleukodystrophy (ALD) is a rare X-linked disease caused by a mutation of Broadway, Baltimore, MD, USA. the peroxisomal ABCD1 gene. This review summarizes our current understanding Email: [email protected] of the pathogenic cell- and tissue-specific roles of lipid species in the context of Funding information experimental therapeutic strategies and provides an overview of critical historical Equipment and partial salary support for AM and AF was provided by the developments, therapeutic trials and the advent of newborn screening in the USA. In Intellectual and Developmental Disabilities ALD, very long-chain fatty acid (VLCFA) chain length-dependent dysregulation of Research Centers at the Kennedy endoplasmic reticulum stress and mitochondrial radical generating systems inducing Krieger Institute and Johns Hopkins University, Grant/Award Number: NICHD cell death pathways has been shown, providing the rationale for therapeutic moiety- U54HD079123 specific -

Arbiter, September 20 Students of Boise State University
Boise State University ScholarWorks Student Newspapers (UP 4.15) University Documents 9-20-2001 Arbiter, September 20 Students of Boise State University Although this file was scanned from the highest-quality microfilm held by Boise State University, it reveals the limitations of the source microfilm. It is possible to perform a text search of much of this material; however, there are sections where the source microfilm was too faint or unreadable to allow for text scanning. For assistance with this collection of student newspapers, please contact Special Collections and Archives at [email protected]. " . Meet a real, live linguistic :e·.·.·.···· genius - pg. 3 Vol, 15 IsSue 8··•.HrsLCOpy Free.... Thursday September 20. 2001 Hispanic Heritage Month in full svving Ry Laura Wylde Center. of students of Hispanic decent. The Arbiter "These activities are all a Dinh said this is the largest eth- very easy, light and non-threat- nic group on campus. Saturday marked the kickoff ening way of learning a cul- "These events provide sup- ture," Dinh said. port for these students to feel date for the Hispanic Heritage Many students enjoy shar- comfortable," she said. Month celebrations at Boise ing their cultures with others. OELA is the supporting State University. "We are all at the same uni- organization for these events, Sunday was the versity," said Dora Barroso, and acknowledges the contri- Independence Day for Mexico, historian for OELA, Boise bution provided by the but celebrations were curbed in light of the recent tragedy. State's Organization of Latin- Cultural Center. American Students. "It is nice "We couldn't have done this However, festivities to know about different people without the Cultural Center," resumed Monday on the cam- and cultures." Calderon said. -

Summit on the National Effort to Prevent Mental Retardation and Related Disabilities
DOCUMENT RESUME ED 339 162 EC 300 772 TITLE Summit on the National Effort To Prevent Mental Retardation and Related Disabilities. Summit Proceedings (Washington, D.C., February 6-7, 1991). INSTITUTION Administration for Children, Youth, and Families (DHHS), Washington, D.C.; President's Committee on Mental Retardation, Washington, D.C. REPORT NO DHMS(ACF)91-21045 PUB DATE Feb 91 NOTE 247p. PUB TYPE Collected Works - Conference Proceedings (021) EDRS PRICE MIF01/PC10 Plus Postage. DESCRIPTORS *Agency Cooperation; Change Strategies; Child Health; Cooperative Planning; *Developmental Disabilities; Elementary Secondary Education; *Mental Retardation; *Prevention; Program Development; *Public Policy; *Socioeconomic Influences; State Programs; Statewide Planning ABSTRACT This document reports the proceedings of a summit to assess the adequacy of the U.S. effort to prevent mental retardation and related disabilities and to chart the course for future strategies to reduce the incidence and ameliorate the effects of these disabilities, particularly when caused by socioeconomic conditions. The document contains "Statement of Occasion: The Challenge" by Hugo Moser, a keynote address by Duane Alexander titled "A National Prevention Strategy for Addressing Conditions Mat Negatively Affect Mothers and Children," and an awards luncheon address by Louis W. Sullivan titled "Comments on the Nationaa Effort To Prevent Mental Retardation and Related Disabilities." The following papers are also included: "Impact of the 'NewMorbidity' on Epidemiological Rates -

Peptide 1-42 and Incipient Alzheimer's Disease
BRIEF COMMUNICATIONS (ioESM) is still the gold standard for the detection of Language Area Localization these essential language areas.2 Noninvasive functional neuroimaging techniques are emerging as promising with Three-Dimensional 4,5 clinical tools for this purpose. Functional Magnetic Functional magnetic resonance imaging (fMRI) is a completely noninvasive preoperative method of deter- Resonance Imaging Matches mining whole-brain functional neuroanatomy.6,7 It en- ables localization of brain function with high spatial Intrasulcal Electrostimulation and temporal resolution by monitoring the hemody- in Broca’s Area namic changes that are coupled with neuronal activity. We report successful identification of Broca’s area G. J. M. Rutten, MD,* P. C. van Rijen, MD, PhD,* within a sulcus 5 to 8 mm below the cortical surface C. W. M. van Veelen, MD, PhD,* and N. F. Ramsey, PhD† using three-dimensional (3D) fMRI and ioESM in a 14-year-old girl with a left inferior frontal desmoplastic ganglioglioma. In this study, intraoperative electrocortical stimulation mapping (ioESM), the current gold standard for the lo- Patient and Methods calization of critical language areas, is compared with Case Report functional magnetic resonance imaging (fMRI) in a 14- The 14-year-old patient has suffered from medically intrac- year-old girl with medically intractable epilepsy caused table complex partial seizures since she was 4 years old. by a tumor in the region of Broca’s area. Prior to the Computed tomography and MRI revealed a calcified, intra- operation, four different fMRI tasks that target inferior axial, noncontrast-enhancing lesion (diameter, 3 cm) within frontal language areas were applied. -

A History of the Saul R. Korey Department of Neurology at the Albert Einstein College of Medicine, 1955-2001
4HISTORICAL PERSPECTIVE A History of the Saul R. Korey Department of Neurology at the Albert Einstein College of Medicine, 1955-2001 Isabelle Rapin Saul R. Korey Department of Neurology Department of Pediatrics Rose F. Kennedy Center for Research in Mental Retardation and Human Development Albert Einstein College of Medicine Bronx, New York 10461 he most salient feature of the early Neurology Department was that, within less than five years, it T had attained national and international status. What made it so? Its rocket ascent can be attributed to two interlocking features. The first was that when the Albert Einstein College of Medicine (AECOM) was conceived, anti-Semitism in academe was still alive and thriving. As a result, the infant College was able to recruit a stellar faculty attracted by its charter with a clear statement of non-discrimination. The same charter also may have influenced Albert Einstein to lend his name to this non-sectarian branch of a Jewish university. The second feature was the extraordinary coup of the Professor and Chairman of Medicine, Irving London, himself a distinguished clinician/investigator, when he re- cruited Saul R. Korey to chair the Division of Neurology in Medicine. This was done with the understanding that neurology would become an independent department FIGURE 1 Saul R. Korey, founder and first Chair of the Albert Einstein when it had accrued sufficeint faculty and a residency College of Medicine Department of Neurology (1955-1963). program. Yeshiva President Belkin granted departmental status in July 1961. trained generations of neurology residents. Labe Scheinberg was acting Chair and then Co-chair of the Department from 1963 to 1970 as well as Dean of the SAUL R. -

ICC-Book-With-Cover 11-17
Sir William Osler Image in public domain (PD-1923) THE INTERURBAN CLINICAL CLUB (1905–2015) A RECORD OF ACHIEVEMENT IN CLINICAL AND BIOMEDICAL SCIENCE R John N. Forrest, Jr ACKNOWLEDGMENTSR The following are gratefully acknowledged for contributing financial support for the book. Department chairs: Mark Zeidel Department of Medicine Beth Israel Deaconess Medical Center Harvard Medical School Gary Desir Department of Medicine Yale School of Medicine Donald Landry Department of Medicine Columbia College of Physicians and Surgeons Richard Shannon Former Chair, Department of Medicine Perelman School of Medicine University of Pennsylvania Michael Parmacek Department of Medicine Perelman School of Medicine University of Pennsylvania Myron Weisfeldt Former Chair, Department of Medicine Johns Hopkins School of Medicine Joseph Loscalzo Chair, Department of Medicine Brigham and Women’s Hospital Harvard Medical School Individuals who contributed to the MD-PhD fund: Jonathan Epstein Executive Vice Dean and Chief Scientific Officer Perelman School of Medicine University of Pennsylvania Barbara Kazmierczak MSTP Director Yale School or Medicine I Copyright 2016 The Interurban Clinical Club. Published by the New York Academy of Sciences II DEDICATIONR for Catherine Lee Kiene Forrest III IV GREETINGS FROM THE OSLERR FAMILY The descendants of the Osler family sincerely wish to thank the editor and the active and emeritus members of the Interurban Clinical Club (ICC) for this book that keeps alive the ongoing celebration of the legacy of Sir William Osler as the founder of the club. Medicine is ever changing, but the concept of getting together to hear diverse scientific papers of new findings from the best creative physician-scientists of five east coast cities (Boston, New Ha- ven, New York City, Philadelphia and Baltimore) will never be out of date. -

NEWSLETTER Volume 14, No
Spring 06_rd 5/24/06 12:48 PM Page 1 NEWSLETTER Volume 14, No. 1 CHILD NEUROLOGY SOCIETY 35th Annual Meeting Program Preview Wednesday, October 18 7:45 AM – 8:15 AM Historical Descriptions of SMA 7:30 AM - 5:30 PM Victor Dubowitz, MD, NEUROBIOLOGY OF DISEASE PhD, FRCP, DHC IN CHILDREN SYMPOSIUM Hammersmith University London, UK Spinal Muscular Atrophy 8:15 AM – 8:45 AM Supported by grants from the Clinical Classification and National Institutes of Health Disease Heterogeneity (NIH grant 1 R13 NS40925-01), Barry Russman, MD Families of Spinal Muscular Atrophy, Oregon Health & Science the Claire Altman Heine Foundation, Inc., University 35th Annual and the Child Neurology Society. Portland, OR Meeting CME ACTIVITY 8:45 AM – 9:30 AM Moderator: Bernard L. Maria, MD, October 18-21, 2006 Modern Diagnosis and MBA, Jeffrey Edwin Gilliam Chair and Management Executive Director of the Children’s Davis L. Lawrence Convention Tom Prior, PhD Research Institute, Medical University Center/Westin Convention Ohio State University of South Carolina, Charleston, SC Center Hotel Columbus, OH AND Pittsburgh, PA 7:30 AM – 7:45 AM Susan Iannaccone, MD Introduction and Statement of Goals 9:30 AM – 9:50 AM Bernard L. Maria, MD, MBA Question and Answer Session CLINICAL NEUROLOGY OF SMA Moderator: Susan Iannaccone, MD, FAAN University of Texas Southwestern Medical Center, Dallas, TX Continued on page four In This Issue President’s Letter 35th Annual ACNN News Personal Registry 2 4 Meeting 7 8 Spring 06_rd 5/24/06 12:48 PM Page 2 PAGE TWO CHILD NEUROLOGY SOCIETY From the President Springing Forward to Fall t is hard to believe, with spring having There are, of course, a number of others Ibarely arrived, that preparations are well working hard behind the scenes this year and underway for the annual fall meeting in every year. -

A Parent's Guide
A Parent’s Guide A Guide to Living with ALD (Adrenoleukodystrophy) Ken, Suzanne, Charlotte, Patrick, & Gavin With proactive, comprehensive medical care the symptoms of ALD can be managed and give the individual the best quality of life possible. aldnewbornscreening.org 3 Letter from an ALD Mom You will have the constant support and guidance of ALD specialists and other ALD parents. You are not alone. Dear Parent(s): This welcome letter is written with much love from a mother who understands all too well how you are feeling in this moment. I have sat where you sit and felt the pain and devastation of having my son diagnosed with Adrenoleukodystrophy (ALD) through Newborn Screening (NBS). I felt the anguish and fear wash over me, washing away all of my hopes and dreams for my child. It felt like the world was coming to an end. Please let my words comfort and assure you that this is not the end. In fact, it is the beginning. It is the beginning of a journey you will take to ensure the health of your precious child. Early diagnosis through NBS is the key. Knowledge is power. Life with ALD can be a full, healthy, and normal one. While it will not always be easy, I can assure you that it is absolutely possible. With NBS for ALD being new, and ALD just beginning to be diagnosed in growing numbers, there was little information available to help new parents. This booklet is our way of sharing all that we have learned to help guide you on this journey. -

Zellweger Syndrome) (Peroxisome Disease/Organelie Biogenesis/Sodium Carbonate Membrane Isolation/Immunoblots/Kidney) PAUL B
Proc. Nati. Acad. Sci. USA Vol. 83, pp. 9193-9196, December 1986 Medical Sciences Presence of the peroxisomal 22-kDa integral membrane protein in the liver of a person lacking recognizable peroxisomes (Zellweger syndrome) (peroxisome disease/organelie biogenesis/sodium carbonate membrane isolation/immunoblots/kidney) PAUL B. LAZAROW*t, YUKIO FuJIKI*t, GILLIAN M. SMALL*, PAUL WATKINS§, AND HUGO MOSER§ *The Rockefeller University, New York, NY 10021; and §The John F. Kennedy Institute and Department of Neurology, The Johns Hopkins University, Baltimore, MD 21205 Communicated by DeWitt Stetten, Jr., August 11, 1986 ABSTRACT Peroxisomes have not been detected in liver consequences. Two possible defects are in the assembly of and kidney of patients with Zellweger syndrome. Some peroxi- the peroxisome membrane or in the import of matrix pro- some proteins are missing; others are present in normal teins. This paper communicates our first step in investigating amounts but are located in the cytosol. We have prepared an peroxisome membrane proteins in Zellweger syndrome. We antiserum against the 22-kDa integral membrane protein show that normal human liver contains an integral membrane characteristic of rat liver peroxisomes. The antiserum cross- protein that is the same size as, and cross-reacts immuno- reacts with the human liver counterpart, which likewise has a logically with, the 22-kDa integral membrane protein (22IMP) mass of 22 kDa. By immunoblot analysis, we demonstrate that that we previously demonstrated to be located exclusively in the 22-kDa protein is present in normal amount in Zellweger peroxisomes in rat liver (17). Rat 22IMP is synthesized on liver and is integral to a membrane. -

Nazi-Era Provenance Research Project
NAZI-ERA PROVENANCE RESEARCH PROJECT As part of its mission and commitment to the artwork in its care, Tacoma Art Museum conducts ongoing research on works in the collection including the provenance—or ownership history—for each work. A particular focus of this study is the European works acquired by the museum after 1932, which could have been in Continental Europe during the Nazi era (1932-1945). In the years prior to and during World War II, Adolf Hitler and the Nazi regime confiscated an unknown number works of art from governments, institutions, and individuals in the countries under their control. After the war, many of these artworks subsequently made their way into museums and private collections. In May 2001, the American Association of Museums (AAM) issued a series of guidelines for helping identify and publish confiscated works held in American museums and in 2003 launched the Nazi-Era Provenance Internet Portal (www.nepip.org) providing a searchable central registry of these works and their histories. With the listing on NEPIP and additional information on this webpage, Tacoma Art Museum seeks to provide greater transparency regarding art in the permanent collection that meets the criteria established by AAM for Nazi-era provenance. Following the guidelines for research and core values set forth by the Association of Art Museum Directors in May 2007, Tacoma Art Museum continues to research and document its permanent collection. Following is a list of works in Tacoma Art Museum’s collection that have an incomplete or ambiguous provenance. In the interests of complete transparency, this list includes European prints as well as paintings.