The Road to an Improved Magic Bullet: Combating Antibiotic Resistance in the Genetic Era
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Recipesholdings, & User Guide
LLC 10-SECOND RECIPESHOLDINGS, & USER GUIDE CAPBRAN IMPORTANT SAFEGUARDS • AFTER BLENDING INGREDIENTS, REMOVE THE CROSS BLADE ASSEMBLY—ALLOW THE VESSEL WITH ITS CONTENTS TO SETTLE AND TO RELEASE ANY PRESSURE THAT MAY HAVE BUILT UP DURING THE EXTRACTION PROCESS. IF YOU WILL NOT CONSUME IT IMMEDIATELY, SAVE THESE INSTRUCTIONS USE THE STAY FRESH LID TO CLOSE THE CONTAINER. UNSCREW THE LID AND RELEASE HOUSEHOLD USE ONLY PRESSURE PERIODICALLY IF STORING LONGER THAN A FEW HOURS TO RELEASE ANY ADDED PRESSURE THAT MAY HAVE BUILT UP DUE TO FERMENTATION. Read all instructions before operating the Magic Bullet. When using electrical • NEVER PERMIT ANY BLENDED MIXTURE TO SIT INSIDE A CUP SEALED WITH A CROSS appliances, basic safety precautions should always be followed, including: BLADE BASE WITHOUT FIRST RELEASING THE PRESSURE. • DO NOT ALLOW BLENDED CONTENTS TO SIT FOR LONG PERIODS IN A SEALED GENERAL SAFETY CONTAINER. THE SUGARS IN FRUITS AND VEGETABLES CAN FERMENT, CAUSING PRESSURE TO BUILD UP AND EXPANDLLC IN THE VESSEL WHICH CAN CAUSE INGREDIENTS • Cross blades are sharp. Handle carefully. TO BURST AND SPRAY OUT WHEN MOVED OR OPENED. UNCSCREW THE LID AND OPEN • Always use your Magic Bullet on a clean, flat, hard, dry surface, never on cloth or paper THE CUP FOR A FEW MOMENTS TO RELEASE ANY PRESSURE THAT HAS BUILT UP. which may block the fan vents and cause overheating. • RELEASE PRESSURE BY CAREFULLY UNSCREWING THE LID AND OPENING THE CUP FOR • Do not immerse the cord, plug or base in water or other liquids. A FEW MOMENTS. • Close supervision is necessary when any appliances are used by or near children. -

Diphtheria Serum and Serotherapy. Development, Production and Regulation in Fin De Siècle Germany
Diphtheria serum and serotherapy. Development, Production and regulation in fin de siècle Germany Axel C. Hüntelmann Institute for the History of Medicine, Ruprecht-Karls-University Heidelberg. [email protected] Dynamis Fecha de recepción: 3 de enero de 2007 [0211-9536] 2007; 27: 107-131 Fecha de aceptación: 8 de marzo de 2007 SUMMARY: 1.—Introduction. 2.—The socio-cultural context of science in fin de siècle Germany. 3.— The development of diphtheria serum in Germany. 4.—The production of diphtheria serum in the German Empire. 5.—State control of diphtheria serum. 6.—Serum networks and indirect state regulation. ABSTRACT: The development, production and state regulation of diphtheria serum is outlined against the background of industrialisation, standardization, falling standards of living and rising social conflict in fin de siècle Germany. On one hand, diphtheria serum offered a cure for an infectious disease and was a major therapeutic innovation in modern medicine. On the other hand, the new serum was a remedy of biological origin and nothing was known about its side effects or long-term impact. Moreover, serum therapy promised high profits for manufacturers who succeeded in stabilizing the production process and producing large quantities of serum in so-called industrial production plants. To minimize public health risks, a broad system of state regulation was installed, including the supervision of serum production and distribution. The case of diphtheria serum illustrates the indirect forms of government supervision and influence adopted in the German Empire and the cooperation and networking among science, state and industry. PALABRAS CLAVE: suero antidiftérico, Alemania, regulacion estatal, seroterapia, redes entre ciencia, estado e industria, Emil Behring. -

Commencement1991.Pdf (8.927Mb)
TheJohns Hopkins University Conferring of Degrees At the Close of the 1 1 5th Academic Year MAY 23, 1991 Digitized by the Internet Archive in 2012 with funding from LYRASIS Members and Sloan Foundation http://archive.org/details/commencement1991 Contents Order of Procession 1 Order of Events 2 Johns Hopkins Society of Scholars 10 Honorary Degree Citations 12 Academic Regalia 15 Awards 17 Honor Societies 21 Student Honors 23 Degree Candidates 25 As final action cannot always be taken by the time the program is printed, the lists of candidates, recipients of awards and prizes, and designees for honors are tentative only. The University reserves the right to withdraw or add names. Order ofProcession MARSHALS Sara Castro-Klaren Peter B. Petersen Eliot A. Cohen Martin R. Ramirez Bernard Guyer Trina Schroer Lynn Taylor Hebden Stella M. Shiber Franklin H. Herlong Dianne H. Tobin Jean Eichelberger Ivey James W. Wagner Joseph L. Katz Steven Yantis THE GRADUATES * MARSHALS Grace S. Brush Warner E. Love THE FACULTIES **- MARSHALS Lucien M. Brush, Jr. Stewart Hulse, Jr. THE DEANS MEMBERS OF THE SOCIETY OF SCHOLARS OFFICERS OF THE UNIVERSITY THE TRUSTEES CHDZF MARSHAL Noel R. Rose THE VICE PRESIDENT OF THE JOHNS HOPKINS UNDTERSLTY ALUMNI ASSOCIATION THE CHAPLAINS THE PRESENTERS OF THE HONORARY DEGREE CANDIDATES THE HONORARY DEGREE CANDIDATES THE INTERIM PROVOST OF THE UNIVERSITY THE CHADIMAN OF THE BOARD OF TRUSTEES THE PRESIDENT OF THE UNDTERSLTY 1 Order ofEvents William (.. Richardson President of the University, presiding * * « PRELUDE Suite from the American Brass Band Journal G.W.E. Friederich (1821-1885) Suite from Funff— stimmigte blasenda Music JohannPezel (1639-1694) » PROCESSIONAL The audience is requested to stand as the Academic Procession moves into the area and to remain standing after the Invocation. -

The Modern Drug Development - from Bench to Market
How are new drugs discovered and developed ? Discovery • Target identification, selection and validation • Target to Hit, Hit to Lead • Lead to Candidate (Lead Optimization) Development • Preclinical (safety, toxicology) • Clinical (Phase I, II, III) • Post-approval (Phase IV, post-market surveillance) 1 What is a drug ? Article intended for use in the diagnosis, cure, mitigation, treatment, or prevention of disease in humans or other animals; and articles (other than food) intended to affect the structure or any function of the body of humans or other animals. (FDA definition) Food and Drug Administration (FDA): a federal agency responsible for monitoring trading and safety standards in the food and drug industries. European Medicines Agency (EMA, EMEA): a European Union agency for the evaluation of medicinal products. Agenzia Italiana del Farmaco (AIFA). Once upon a time … Paul Ehrlich (1854–1915) 1890 German immunologist Paul Ehrlich (1854-1915) developed a chemical theory to explain the body’s immune response and did important work in chemotherapy, coining the term magic bullet. Ehrlich received the Nobel Prize in 1908. http://tibbs.unc.edu/magic-bullet-or-shot-in-the-dark/ The Side-chain theory and the magic bullet 3 From Immunology to The Magic Bullet Zauberkugel-Theorie’ A chemical substance can selectively affect physiological processes in the body. “A ‘magic bullet’ is a substance that can seek out and kill the disease causing agents only”. 4 The Movie 1940 5 Salvarsan (Hoechst) the first chemotherapy Arsphenamine (Salvarsan or compound 606) is a drug introduced at the beginning of the 1910s as the first effective treatment for syphilis, and was also used to treat trypanosomiasis. -

Metchnikoff and the Phagocytosis Theory
PERSPECTIVES TIMELINE Metchnikoff and the phagocytosis theory Alfred I. Tauber Metchnikoff’s phagocytosis theory was less century. Indeed, the clonal selection theory and an explanation of host defence than a the elucidation of the molecular biology of the proposal that might account for establishing immune response count among the great and maintaining organismal ‘harmony’. By advances in biology during our own era5. tracing the phagocyte’s various functions Metchnikoff has been assigned to the wine cel- Figure 1 | Ilya Metchnikoff, at ~45 years of through phylogeny, he recognized that eating lar of history, to be pulled out on occasion and age. This figure is reproduced from REF. 14. the tadpole’s tail and killing bacteria was the celebrated as an old hero. same fundamental process: preserving the However, to cite Metchnikoff only as a con- integrity, and, in some cases, defining the tributor to early immunology distorts his sem- launched him into the turbulent waters of evo- identity of the organism. inal contributions to a much wider domain. lutionary biology. He wrote his dissertation on He recognized that the development and func- the development of invertebrate germ layers, I first encountered the work of Ilya tion of the individual organism required an for which he shared the prestigious van Baer Metchnikoff (1845–1916; FIG. 1) in Paul de understanding of physiology in an evolution- Prize with Alexander Kovalevski. By the age of Kruif’s classic, The Microbe Hunters 1.Who ary context. The crucial precept: the organism 22 years, he was appointed to the position of would not be struck by the description of this was composed of various elements, each vying docent at the new University of Odessa, where, fiery Russian championing his theory of for dominance. -

Microbe Hunters Revisited Yale University School of Medicine, New Haven, Connecticut, USA
INTERNATL MICROBIOL (1998) 1: 65-68 65 © Springer-Verlag Ibérica 1998 PERSPECTIVES William C. Summers Microbe Hunters revisited Yale University School of Medicine, New Haven, Connecticut, USA Correspondence to: William C. Summers. Yale University School of Medicine. 333 Cedar St. New Haven, CT 06520-8040. USA. Tel.: +1-203-785 2986. Fax: +1-203-785 6309. E-mail: [email protected] It was the mid-1950s and I was a teenager when I first Indeed, Microbe Hunters is a book about success: tales of read Microbe Hunters by Paul Henry De Kruif (Zealand, MI, brilliant research, incisive investigations, and heroic 1890–Holland, MI, 1971). It was the right time and the right personalities. Yet it is far from “history-objectively written.” age; I was fascinated. Here were heros enough to satisfy any The formula that De Kruif hit upon in Microbe Hunters served bookish young man interested in the natural world. Microbe him well: between 1928 and 1957 he wrote eleven more books Hunters was a book that inspired a generation or more of on medical and scientific topics, all with the same “exciting budding young microbiologists [4]. Not only that, however. narrative” and sense of drama. Some of these books were best- It established a metaphor and a genre of science writing that sellers and selected by the popular Book-of-the-Month Club. has often been imitated. None, however, matched the popularity and appeal of Microbe Microbe Hunters is a series of 12 stories that describe major Hunters. events in the history of microbiology, from microscopic De Kruif’s stories are full-scale dramatizations, complete observations of animalcules (literally “little animals”) by with fictional dialog of the historical subjects, and first person Leeuwenhoek (“First of the Microbe Hunters”) to Paul Ehrlich’s interjections of the voice of the narrator, De Kruif. -

Balcomk41251.Pdf (558.9Kb)
Copyright by Karen Suzanne Balcom 2005 The Dissertation Committee for Karen Suzanne Balcom Certifies that this is the approved version of the following dissertation: Discovery and Information Use Patterns of Nobel Laureates in Physiology or Medicine Committee: E. Glynn Harmon, Supervisor Julie Hallmark Billie Grace Herring James D. Legler Brooke E. Sheldon Discovery and Information Use Patterns of Nobel Laureates in Physiology or Medicine by Karen Suzanne Balcom, B.A., M.L.S. Dissertation Presented to the Faculty of the Graduate School of The University of Texas at Austin in Partial Fulfillment of the Requirements for the Degree of Doctor of Philosophy The University of Texas at Austin August, 2005 Dedication I dedicate this dissertation to my first teachers: my father, George Sheldon Balcom, who passed away before this task was begun, and to my mother, Marian Dyer Balcom, who passed away before it was completed. I also dedicate it to my dissertation committee members: Drs. Billie Grace Herring, Brooke Sheldon, Julie Hallmark and to my supervisor, Dr. Glynn Harmon. They were all teachers, mentors, and friends who lifted me up when I was down. Acknowledgements I would first like to thank my committee: Julie Hallmark, Billie Grace Herring, Jim Legler, M.D., Brooke E. Sheldon, and Glynn Harmon for their encouragement, patience and support during the nine years that this investigation was a work in progress. I could not have had a better committee. They are my enduring friends and I hope I prove worthy of the faith they have always showed in me. I am grateful to Dr. -
Buffy & Angel Watching Order
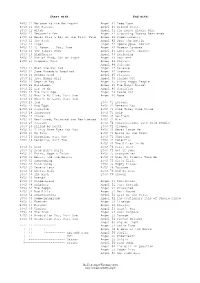
Start with: End with: BtVS 11 Welcome to the Hellmouth Angel 41 Deep Down BtVS 11 The Harvest Angel 41 Ground State BtVS 11 Witch Angel 41 The House Always Wins BtVS 11 Teacher's Pet Angel 41 Slouching Toward Bethlehem BtVS 12 Never Kill a Boy on the First Date Angel 42 Supersymmetry BtVS 12 The Pack Angel 42 Spin the Bottle BtVS 12 Angel Angel 42 Apocalypse, Nowish BtVS 12 I, Robot... You, Jane Angel 42 Habeas Corpses BtVS 13 The Puppet Show Angel 43 Long Day's Journey BtVS 13 Nightmares Angel 43 Awakening BtVS 13 Out of Mind, Out of Sight Angel 43 Soulless BtVS 13 Prophecy Girl Angel 44 Calvary Angel 44 Salvage BtVS 21 When She Was Bad Angel 44 Release BtVS 21 Some Assembly Required Angel 44 Orpheus BtVS 21 School Hard Angel 45 Players BtVS 21 Inca Mummy Girl Angel 45 Inside Out BtVS 22 Reptile Boy Angel 45 Shiny Happy People BtVS 22 Halloween Angel 45 The Magic Bullet BtVS 22 Lie to Me Angel 46 Sacrifice BtVS 22 The Dark Age Angel 46 Peace Out BtVS 23 What's My Line, Part One Angel 46 Home BtVS 23 What's My Line, Part Two BtVS 23 Ted BtVS 71 Lessons BtVS 23 Bad Eggs BtVS 71 Beneath You BtVS 24 Surprise BtVS 71 Same Time, Same Place BtVS 24 Innocence BtVS 71 Help BtVS 24 Phases BtVS 72 Selfless BtVS 24 Bewitched, Bothered and Bewildered BtVS 72 Him BtVS 25 Passion BtVS 72 Conversations with Dead People BtVS 25 Killed by Death BtVS 72 Sleeper BtVS 25 I Only Have Eyes for You BtVS 73 Never Leave Me BtVS 25 Go Fish BtVS 73 Bring on the Night BtVS 26 Becoming, Part One BtVS 73 Showtime BtVS 26 Becoming, Part Two BtVS 74 Potential BtVS 74 -

Of Rabbits and Men: the Tale of Paul Ehrlich in Our Modern World Of
Of Rabbits and Men: The Tale of Paul Ehrlich In our modern world of chemotherapy, antibiotics and antivirals, it might come as a surprise to find that the origin of all these treatments can be traced back to rabbits; the cute and fluffy kind. To understand why, we need to go all the way back to 1882 Berlin. A talented, if aimless, young German doctor, Paul Ehrlich, had just met the great microbiologist Robert Koch. Koch was giving a lecture in which he identified the pathogen responsible for tuberculosis. Ehrlich was instantly fascinated by Koch and microbiology. Unknown to himself, he had just taken the first step on a path that would help change the way disease is tackled forever1. The late 1800’s were a time of dynamic change in the sciences. Charles Darwin had proposed his Theory of Natural Selection and Thomas Edison had given us the light bulb. Amongst the many fashionable topics of the time, some biologists were fascinated by dyes; specifically the staining of living tissue. Spending all day bent over a microscope looking at the pretty colours might not seem like worthwhile science by modern standards, but these dyes had interesting properties. Dyes displayed a high level of specificity; they would only stain certain structures and pass through others. Ehrlich noticed this and soon started to think of applications for these properties. These were times when catching a chill could kill. Many well-known individuals of the time were killed in their prime due to infectious disease. Emily Brontë died from tuberculosis2, René Descartes from pneumonia3 and Pyotr Tchaikovsky died from cholera4. -

UNIVERSITY of CALIFORNIA the Role of United States Public Health Service in the Control of Syphilis During the Early 20Th Centu
UNIVERSITY OF CALIFORNIA Los Angeles The Role of United States Public Health Service in the Control of Syphilis during the Early 20th Century A dissertation submitted in partial satisfaction of the requirements for the degree of Doctor of Public Health by George Sarka 2013 ABSTRACT OF THE DISSERTATION The Role of United States Public Health Service in the Control of Syphilis during the Early 20th Century by George Sarka Doctor of Public Health University of California, Los Angeles, 2013 Professor Paul Torrens, Chair Statement of the Problem: To historians, the word syphilis usually evokes images of a bygone era where lapses in moral turpitude led to venereal disease and its eventual sequelae of medical and moral stigmata. It is considered by many, a disease of the past and simply another point of interest in the timeline of medical, military or public health history. However, the relationship of syphilis to the United States Public Health Service is more than just a fleeting moment in time. In fact, the control of syphilis in the United States during the early 20th century remains relatively unknown to most individuals including historians, medical professionals and public health specialists. This dissertation will explore following question: What was the role of the United States Public Health Service in the control of syphilis during the first half of the 20th century? This era was a fertile period to study the control of syphilis due to a plethora of factors including the following: epidemic proportions in the U.S. population and military with syphilis; the ii emergence of tools to define, recognize and treat syphilis; the occurrence of two world wars with a rise in the incidence and prevalence of syphilis, the economic ramifications of the disease; and the emergence of the U.S. -

Magic Bullet” Is Here? Cell-Based Immunotherapies for Hematological Malignancies in the Twilight of the Chemotherapy Era
cells Review The “Magic Bullet” Is Here? Cell-Based Immunotherapies for Hematological Malignancies in the Twilight of the Chemotherapy Era Nina Miazek-Zapala 1,2, Aleksander Slusarczyk 1,3 , Aleksandra Kusowska 1, Piotr Zapala 3, Matylda Kubacz 1, Magdalena Winiarska 1 and Malgorzata Bobrowicz 1,* 1 Department of Immunology, Medical University of Warsaw, 02-097 Warsaw, Poland; [email protected] (N.M.-Z.); [email protected] (A.S.); [email protected] (A.K.); [email protected] (M.K.); [email protected] (M.W.) 2 Institute of Physiology and Pathophysiology of Hearing, World Hearing Center, 05-830 Nadarzyn, Poland 3 Department of General, Oncological and Functional Urology, Medical University of Warsaw, 02-005 Warsaw, Poland; [email protected] * Correspondence: [email protected] Abstract: Despite the introduction of a plethora of different anti-neoplastic approaches including standard chemotherapy, molecularly targeted small-molecule inhibitors, monoclonal antibodies, and finally hematopoietic stem cell transplantation (HSCT), there is still a need for novel therapeutic options with the potential to cure hematological malignancies. Although nowadays HSCT already offers a curative effect, its implementation is largely limited by the age and frailty of the patient. Moreover, its efficacy in combating the malignancy with graft-versus-tumor effect frequently coexists with undesirable graft-versus-host disease (GvHD). Therefore, it seems that cell-based adoptive Citation: Miazek-Zapala, N.; immunotherapies may constitute optimal strategies to be successfully incorporated into the standard Slusarczyk, A.; Kusowska, A.; Zapala, P.; Kubacz, M.; Winiarska, M.; therapeutic protocols. Thus, modern cell-based immunotherapy may finally represent the long- Bobrowicz, M. -
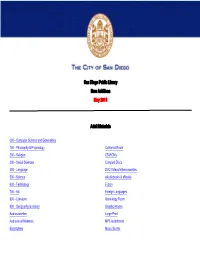
San Diego Public Library New Additions May 2011
San Diego Public Library New Additions May 2011 Adult Materials 000 - Computer Science and Generalities 100 - Philosophy & Psychology California Room 200 - Religion CD-ROMs 300 - Social Sciences Compact Discs 400 - Language DVD Videos/Videocassettes 500 - Science eAudiobooks & eBooks 600 - Technology Fiction 700 - Art Foreign Languages 800 - Literature Genealogy Room 900 - Geography & History Graphic Novels Audiocassettes Large Print Audiovisual Materials MP3 Audiobooks Biographies Music Scores Newspaper Room Fiction Call # Author Title [MYST] FIC/ALEXANDER Alexander, Bruce Murder in Grub Street [MYST] FIC/ANABLE Anable, Stephen A Pinchbeck bride [MYST] FIC/BAUER Bauer, Belinda Darkside [MYST] FIC/BLOCK Block, Lawrence. A drop of the hard stuff : a Matthew Scudder novel [MYST] FIC/BRANDRETH Brandreth, Gyles Daubeney Oscar Wilde and the vampire murders [MYST] FIC/CAMPBELL Campbell‐Slan, Joanna. Photo, snap, shot : a Kiki Lowenstein mystery [MYST] FIC/COLE Cole, Julian. Felicity's gate : a thriller [MYST] FIC/COONTS Coonts, Deborah. Lucky stiff [MYST] FIC/CORLEONE Corleone, Douglas. Night on fire [MYST] FIC/DELANY Delany, Vicki Among the departed [MYST] FIC/DOUDERA Doudera, Vicki A house to die for [MYST] FIC/EDWARDS Edwards, Martin The hanging wood : a Lake District mystery [MYST] FIC/ELKINS Elkins, Aaron J. The worst thing [MYST] FIC/ERICKSON Erickson, K. J. Third person singular [MYST] FIC/FOWLER Fowler, Earlene. Spider web [MYST] FIC/GHELFI Ghelfi, Brent The burning lake : a Volk thriller [MYST] FIC/GOLDENBAUM Goldenbaum, Sally. The wedding shawl [MYST] FIC/GRAVES Graves, Sarah. Knockdown : a home repair is homicide mystery [MYST] FIC/HALL Hall, M. R. The redeemed [MYST] FIC/HAMRICK Hamrick, Janice. Death on tour [MYST] FIC/HARRIS Harris, Charlaine.