Changing the Culture One Step at a Time: Person-Centered Bathing
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-
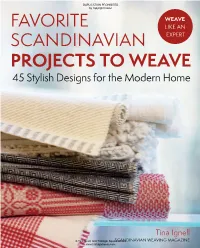
Favorite Scandinavian Projects to Weave, We Have Selected 45 Patterns from Vävmagasinet—The Scandinavian Weaving Magazine
FAVORITE DUPLICATION PROHIBITED by copyright holder WEAVE SCANDINAVIAN FAVORITE LIKE AN SCANDINAVIAN EXPERT PROJECTS TO WEAVE WHAT COULD BE MORE WONDERFUL than surrounding WEAVE TO PROJECTS yourself with gorgeous handwoven textiles? Weaving them yourself! Inside find 45 unique projects, developed and tested by professional weavers, 45 Stylish Designs for the Modern Home and specially chosen for this collection from the popular Scandinavian weaving magazine Vävmagasinet. You’ll enjoy: Step-by-step instructions, charts, illustrations, and color photos Featured fibers, including linen, half-linen, cottolin, wool, paper, and piassava Versatile ideas for pillows, throws, rugs, curtains, table linens, and more, all easily adjusted to suit your own individual style A special section on textile care and handling TINA IGNELL $22.95 USD ISBN 978-1-57076-898-9 5 2 2 9 5 Tina Ignell 9 781570 768989 Printed in China Printed www.trafalgarbooks.com © Tina Ignell, and Trafalgar SquareSCANDINAVIAN Books WEAVING MAGAZINE www.trafalgarbooks.com Favorite Scandi Weaves Full Cover.indd 1 4/30/18 2:05 PM DUPLICATION PROHIBITED by copyright holder First published in the United States of America in 2010 by Trafalgar Square Books North Pomfret, Vermont 05053 Printed in China Originally published in Swedish as Hemvävt Copyright © 2008 Tina Ignell, Bengt Arne Ignell and ICA Bokförlag, Forma Publishing Group AB, Sweden English translation © 2010 Trafalgar Square Books All rights reserved. No part of this book maybe reproduced, by any means, without written permission -
![IS 3781 (1994): Textiles - Honey Comb and Huckaback Towels,Cotton Khadi,Bleached Or Dyed - Specition (Amalgamating IS 3775:1983) [TXD 8: Handloom and Khadi]](https://docslib.b-cdn.net/cover/6205/is-3781-1994-textiles-honey-comb-and-huckaback-towels-cotton-khadi-bleached-or-dyed-specition-amalgamating-is-3775-1983-txd-8-handloom-and-khadi-1206205.webp)
IS 3781 (1994): Textiles - Honey Comb and Huckaback Towels,Cotton Khadi,Bleached Or Dyed - Specition (Amalgamating IS 3775:1983) [TXD 8: Handloom and Khadi]
इंटरनेट मानक Disclosure to Promote the Right To Information Whereas the Parliament of India has set out to provide a practical regime of right to information for citizens to secure access to information under the control of public authorities, in order to promote transparency and accountability in the working of every public authority, and whereas the attached publication of the Bureau of Indian Standards is of particular interest to the public, particularly disadvantaged communities and those engaged in the pursuit of education and knowledge, the attached public safety standard is made available to promote the timely dissemination of this information in an accurate manner to the public. “जान का अधकार, जी का अधकार” “परा को छोड न 5 तरफ” Mazdoor Kisan Shakti Sangathan Jawaharlal Nehru “The Right to Information, The Right to Live” “Step Out From the Old to the New” IS 3781 (1994): Textiles - Honey comb and huckaback towels,cotton khadi,bleached or dyed - Specition (Amalgamating IS 3775:1983) [TXD 8: Handloom and Khadi] “ान $ एक न भारत का नमण” Satyanarayan Gangaram Pitroda “Invent a New India Using Knowledge” “ान एक ऐसा खजाना > जो कभी चराया नह जा सकताह ै”ै Bhartṛhari—Nītiśatakam “Knowledge is such a treasure which cannot be stolen” IS 3781:1994 Indian Standard TEXTILES- HONEYCOMB AND HUCKABACK TOWELS, COTTON KHADI, BLEACHED OR DYED - SPECIFICATION ( First Revision ) UDC 677’21’074’ 162’3 : 645’486 BUREAU OF INDlAN STANDARDS MANAK BHAVAN, 9 BAHADUR SHAH ZAFAR MARG NEW DEL,HI 110002 December 1994 Price Group 2 Handloom and Khadi Sectional Committee, TX 08 FOREWORD This Indian Standard ( First Revision ) was adopted by the Bureau of Indian Standards, after the draft finalized by the Handloom and Khadi Sectional Committee had been approved by the Textile Division Council. -

What Requirements Must Hammam Towels Comply with to Be Allowed on the European Market? 2
Entering the European market for hammam towels Last updated: 29 December 2020 The mid and higher-end segments of the European market offer good opportunities for hammam towels, but competition is strong. You can add value to your products through the use of special techniques and materials, as well as sustainable values. Entering the European market means you need to comply with the European Union’s mandatory legal requirements, as well as any additional or niche requirements your buyers may have. Contents of this page 1. What requirements must hammam towels comply with to be allowed on the European market? 2. Through what channels can you get hammam towels on the European market? 3. What competition do you face on the European hammam towels market? 4. What are the prices for hammam towels on the European market? 1. What requirements must hammam towels comply with to be allowed on the European market? The following requirements apply to hammam towels on the European market. For a more detailed overview, see our study on buyer requirements for home decorations and home textiles (HDHT). What are the mandatory requirements? When exporting to Europe, you must comply with the following legal requirements: General Product Safety Directive REACH Textile Regulation Packaging and packaging waste legislation General Product Safety Europe’s General Product Safety Directive states that all products marketed in Europe must be safe to use. It provides a framework for all legislation regarding specific products and issues. If there are no specific legal requirements established for your product and its use, the General Product Safety Directive still applies. -

RAYON RUGS... Readily Ruined, but Still the Rage
RAYON RUGS... Readily Ruined, But Still the Rage We have published various articles Why might a retailer or It seems that some will do over the years explaining the manufacturer use the term almost anything to keep from shortcomings of rayon. Despite “bamboo silk” instead of rayon? calling their rugs “rayon.” No our best efforts, rayon rugs remain Natural fibers are as popular as other fiber shows up under so extremely popular with designers ever and bamboo is thought of as many different names. Banana and their clients. Undeterred, both natural and sustainable. Silk silk, faux silk and art silk are we bring you—again—our best is, of course, both natural and a almost always rayon (rarely, a information about the limitations luxury fiber. So, the misleading rug will be mercerized cotton). of these products. name really comes down to Luxcelle and Silkette are marketing sizzle (without the steak). tradenames being used for What's in a Name? rayon. Again, the names are For all practical purposes, the confusing (and illegal) because terms rayon and viscose are the fiber content is not interchangeable. There are a immediately recognizable. handful of exceptions, but they are a tiny part of the total market. Problems Abound In fact, the Federal Trade As we’ve mentioned before, we Commission (FTC) says either think of rayon as cotton’s poor name is acceptable. relation. It’s a cellulosic fiber, so it shares a few of cotton’s better What the FTC does not allow qualities (e.g., soft hand and is rayon that is described under resistance to static). -

Towel Products for Institutional and Household Use1
Designation: D 5433 – 00 Standard Performance Specification for Towel Products for Institutional and Household Use1 This standard is issued under the fixed designation D 5433; the number immediately following the designation indicates the year of original adoption or, in the case of revision, the year of last revision. A number in parentheses indicates the year of last reapproval. A superscript epsilon (e) indicates an editorial change since the last revision or reapproval. 1. Scope sumer Textile and Leather Products Other Than Carpets 2 1.1 This specification covers the evaluation of specific and Upholstery performance characteristics of importance in woven and knit- D 3786 Test Method for Hydraulic Bursting Strength of ted kitchen towel, dishcloth, crash towel, huck towel, wash- Knitted Goods and Nonwoven Fabrics—Diaphragm 4 cloth, hand towel, bath towel, and bath sheet products for use Bursting Strength Tester Method in institutional and household environments. D 3787 Test Method for Bursting Strength of Knitted 4 1.2 This specification may be used by mutual agreement Goods—Constant-Rate-of Traverse (CRT) Ball Burst Test between the purchaser and the supplier to establish purchasing D 3882 Test Method for Bow and Skewness (Bias) in 4 specification requirements. Woven and Knitted Fabrics 1.3 The requirements in Tables 1 and 2 apply to the length D 3938 Guide for Evaluation of Textile Products in Relation 4 and width directions for those properties where fabric direction to Refurbishing Described on Care Labels is pertinent. D 4390 Practice for Evaluation of the Performance of Terry 4 1.4 This specification is not applicable for coated and Bathroom Products for Household Use laminated products, nonwoven products, or terry fabrics used D 4772 Test Method for Surface Water Absorption of Terry 4 for apparel. -

The European Market Potential for Hammam Towels 1. Product Description
The European market potential for hammam towels Last updated: 29 December 2020 Hammam towels are a popular product in the European market. Growing consumer interest in wellness and spa experiences, at home or not, are driving this demand, which has been further stimulated by the restrictions imposed in reason of the Covid-19 pandemic. Most of Europe’s home textile imports come from developing countries, but those with a traditional connection to hammam towels are particularly important suppliers of these products. Offering the option to work via co-creation can give you a competitive edge. Contents of this page 1. Product description 2. What makes Europe an interesting market for hammam towels? 3. Which European countries offer most opportunities for hammam towels? 4. What trends offer opportunities on the European hammam towel market? 1. Product description Hammam towels are also known as peshtemal, fouta or Turkish towels. They have been around since the 17th century and were traditionally connected with the Turkish hammam baths. Hammam towels are flat woven and much thinner than conventional terry towels. In recent years, interest has surged internationally and this soft, light, versatile towel has been rapidly gaining popularity. In the home decoration and home textiles (HDHT) sector, hammam towels fall under the bath textiles subcategory within home textiles. This study uses the following codes to indicate trade in hammam towels: Table 1: Product codes* Harmonised System Prodcom Description (HS) Toilet linen and kitchen linen of 6302 91 13 92 14 50 cotton, excluding of terry fabrics * There are no specific HS or Prodcom codes available for hammam towels. -

Rayon & Cotton Scarves & Shawls
RAYON & COTTON SCARVES & SHAWLS BOLIVIAN CO-OP N W RAYON HAND WOVEN EW ITH S WN WIT HANDWOVEN SE H ALPACA SHAWLS PLAIN TWILL JERSEY COTTON THREAD INFINITY COTTON Hand woven from RAYON THREAD 100% Alpaca wool. CHALLIS SCARF Soft. Luxurious. SCARF Fair Trade Made from product from Handwoven luxurious, silky Bolivia, so 100% Rayon soft, liquid the workers Challis draping get almost scarves & 100% every shawls are Rayon penny like a wool Jersey. of every challis Edge purchase. The but much seams are natural can be dyed softer! rolled & with Acid Dyes. Plain stitched. Hand wash. slightly A treat Natural twill to wear, Black Dark Green NOW IN weave. and cozy Red Light Brown Hand too! Purple Light Green COLORS! twisted fringe. #BHAS: undyed natural Continous circle with NO seam join at #BHASC: dyed colors the neck! Sewn with cotton thread. 76” long & 26” wide 69” all the way around & 19” wide New larger size: 24” x SOFT! 72”with a 5” fringe #ISR143 #BRJ416 WN WIT BAMBOO RAYON SCARF SE H RAYON RUANA FLOATING SCARF OR RAYON COTTON W SQUARES THREAD EWN IT SHAWL S H BLEND DESIGN SCARVES Drape & wear it COTTON Handwoven 100% in lots of ways. THREAD These 100% Rayon Challis bamboo rayon Overcast serged scarves & pearl edges. scarves are soft shawls are as heavily Great over like a wool a dress on buttered silk challis covered in summer but much nights or down feathers softer! Sort from a of a floating baby goose! weave Luscious, squares gorgeous design. 100% Super Bamboo soft! Hand Rayon twisted scarves with fringe. -

Tue Text U 5Peqalt Y Gr0up 9 5T P Rim T
TUE TEXT U 5PEQALT Y GR0UP 9 5T P RIM T Edited by Camille Myers Breeze Responsibility for the methods and/or materials described herein rests solely with the contributors and should not be considered official statements of the Textile Specialty Group or AIC. The Textile Specialty Group Postprints is a nonjuried publication. Submission of these papers to juried publications, such as the Journal of the American Instuitute for Conservation, is encouraged. Postprints are distributed to members of the Textile Specialty Group. Additional copies may be purchased from the American Institute for Conservation of Historic and Artistic Works, 1717 K Street, N.W., Washington, D.C. 20006. This volume has been printed on 60 lb. J. B. Offset paper with a 10 pt. UV-coated cover. All materials are acid-free. All rights reserved by the individual authors. Inside cover image: Hamilton Print Works, courtesy of the American Textile History Museum, Lowell, Massachusetts. Volume 8, Copyright © 1999 The Textile Specialty Group of the American Institute for Conservation of Historic and Artistic Works. ISSN 1524-3664 CONTENTS Preface V When Patching is Impractical: Nontraditional Compensation for Loss in a Quilt Susan R. Schmalz 1 Insect Infestation: A Large Tapestry's Fumigation and Stabilization for Storage Betsy Gould 9 Up on the Roof: Light Bleaching of Large Textiles, Two Case Joy Gardiner and Studies Joanne Hackett 15 Borohydride: An Alternative to Oxidative Bleaching of Cellulosic Textiles Susan Adler 27 Disaster Recovery: Teaching Textile Salvage Techniques -

Properties and Serviceability of Selected Household and Clothing Fabrics
/ A R Y U356 SOULTURE Properties and Serviceability of Selected Household and Clothing Fabrics Bibliography and Review of Research Findings 1928-1951 AGRICULTURE INFORMATION BULLETIN No. 147 MAY 1956 U. S. Department of Agriculture Washington, D. C. CONTENTS Page Introduction 1 Household textiles. 2 Blanketing _-__ 2 Curtaining ^^_ :._ 4 Damask, table. 6 Sheeting, cotton, bleached and un- bleached -- 9 Toweling 13 Upholstery fabrics.., _.. 18 Clothing fabrics -■-.-.-^.. 22 References 37 Appendix. Tables of fabric properties 41 Index to fabrics 126 ACKNOWLEDGMENT The authors express their appreciation to Ruth O'Brien for assistance in the prep- aration of the sections on specifications and serviceability of fabrics, and to Elinora Johnson Williams, Mary E. Fajen, and Janet Turner Straiisky for assistance in various phases of the study. For sale by the Superintendent of Documents, U. S. Government Printing Office Washington 25, D. C. - Price 60 cents Properties and Serviceability of Selected Household and Clothing Fabrics Bibliography and Review of Research Findings, 1928-5P By HAZEL M. FLETCHER and S. HELEN KOBEETS :^^ Clothing and Housing Research Branch, Agricultural Research Service INTRODUCTION Research on the properties and serviceability of Since it was difficult in some cases for consumers fabrics has been developed largely in response to to understand the technical terms necessary on the needs of household and institutional buyers the labels that gave construction details, research for information on which to base then: selections. was developed looking toward the establishment Household buyers are continually seeking means of a simple grading system or classification based of judging quality in relation to price. -

Needle Types Fabric/Use Sizes
Needle Types Fabric/Use Sizes Sharp point Lingerie, Silk 60/8 Ball point Lingerie, Silk 60/8 Ball point Organza, Taffeta, Velvet 65/9 Sharp point Cotton Sheeting, Lingerie, Silk 70/10 Dress Shirt (woven), Golf Shirt (Knit), Lingerie, Silk, Lycra, Spandex, Ball point 70/10 Nylon Wind Breaker, Sweatshirt Corduroy, Denim, Lace, Satin Jacket, Sweater, Terry Cloth Towels, Sharp point Vinyl, Cotton Sheeting, Lingerie, Silk, Quilted Totes, Boat Totes, Lunch 75/11 Totes, Backpacks, Cosmetic Bags, Kiwi Paper Corduroy, Rayon, Terry Cloth Towels, Dress Shirt, Golf Shirt, Lingerie, Ball point Silk, Lycra, Spandex, Nylon Wind breaker, Satin Jacket, Sweater Knit, 75/11 Sweatshirt Canvas, Coated or Waterproof Fabrics, Cotton Sheeting, Leather, Sharp point Vinyl, Terry Cloth Towel, Quilted Totes, Boat Totes, Lunch Totes, 80/12 Backpacks, Cosmetic Bags Dress Shirt (woven), Golf Shirt (Knit), Coated/Water Proof, Nylon Ball point 80/12 Windbreaker, Sweatshirt, Lycra, Spandex, Terry Cloth Towel Wedge point Leather 80/12 Sharp point Leather 90/14 Large Eye Filaine specialty threads 90/14 Large Eye Burmilana, Filaine and other 12 weight specialty threads 100/16 Just remember that high quality embroidery is a delicate balance between the design, thread [top & bobbin], stabilizer, needle, and item being stitched. Remember when you change one of these, you are changing more than the needle: ~ The needle size or the eye size of the needle - you are changing the tension on the top thread. ~ The needle size - you are changing the relationship of the needle scarf to the hook point. ~ The needle point - you are changing the way the needle penetrates the fabric. -

Product Catalog 51 Riegel Road Johnston, SC 29832 800-845-2232 Hospitality Bed
Hospitality ® Table Linen A Division of Mount Vernon Mills, Inc. Product Catalog 51 Riegel Road Johnston, SC 29832 800-845-2232 Hospitality www.riegellinen.com Bed Riegel-MVM Hospitality Bath Making Worry - Free Textiles Since 1838 About Mount Vernon Mills, Inc. Making worry-free textiles since 1838, Riegel offers a wide variety of table linen, bedding, and bath products for an all-inclusive one-stop textile shop. A focused and complete line of hospitality sheets in thread counts 180-200- 250 and 300 are a strong foundation of a quality product offering. For added flare and style, the 200tc sheets are also available in bone. The super soft 250tc bedding also is available with a satin-piped luxury pillowcase. Available in matt weave and tonal satin stripe weave, the 300tc is pure luxury and elegance. Hospitality blankets, mattress pads, and duvet covers with shams are also available. Bed bug protection has never been easier with goodmorning™, a complete line of bed bug fighting pillow, mattress, and box spring encasings. Riegel offers a complete line of quality table linen and accessories including DiRoNA, Parnell, Beauti-Damask, Ultimate, Permalux, Premier, Monarch, and Premier-Damask. Banquet spaces come alive with conference cloth in fashion colors and table skirting in polyester and elegant designer fabrics. A proven innovator in textile design, Riegel offers RieNu® 100% recycled polyester, DiRoNa mini check, Vintage Charm, stripe bistro napkins, and polyester denim table cloths and napkins. Promising a towel for every occasion, Riegel’s Cam, Gold, and Royal Terry Towel Collections are offered in a beautiful, bright white finish with a soft hand and superior water absorbency. -

Towels – Specifications
tbs TDC3 (5614)P3 Draft Tanzania Standard Textiles – Towels – Specifications TANZANIA BUREAU OF STANDARDS 0. Foreword This second edition of this Draft Tanzania Standard has been prepared to help manufacturers of towels in producing products of defined quality and hence safeguarding the interests of the consumer. This second edition cancels and replaces the first edition TZS 899: 2006 Textiles – Towels – Specification which is due for review. In this second edition the parameters of mass per unit area, breaking strength and colour fastness have been reviewed so as to be in harmony with technological trend in Tanzania. Performance requirement of knitted terry towels have been incorporated in this second edition. In the preparation of this Draft Tanzania Standard assistance was derived from: KS 408 - Towels – Specification ASTM D5433 -12 Standard Performance Specifications for Towel Products for Institutional and Household Use Acknowledgement is made for the assistance received from these sources. i Tanzania Bureau of Standards Draft Tanzania Standard TDC3 (5614)P2 Textiles – Towel – Specifications 1. Scope 1.1 This Draft Tanzania Standard specifies the evaluation of specific performance characteristics of importance in woven and knitted terry kitchen towel, Dish towel, crash towel, Huck towel, hand towel, wash towel and bath towel. 1.2 The Draft Tanzania Standard may be used by mutual agreement between the purchaser and the supplier to establish purchasing specification requirements. 1.3 This Draft Tanzania Standard is not applicable for coated and laminated products, nonwoven products, or terry fabrics used for apparel. 2. Normative references The following referenced documents are indispensable for the application of this document.