Genotype/Phenotype Correlation in Autosomal Recessive Lamellar
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Genomic Variants Reveal Differential Evolutionary Constraints on Human Transglutaminases and Point Towards Unrecognized Significance of Transglutaminase 2
View metadata, citation and similar papers at core.ac.uk brought to you by CORE provided by University of Debrecen Electronic Archive RESEARCH ARTICLE Genomic variants reveal differential evolutionary constraints on human transglutaminases and point towards unrecognized significance of transglutaminase 2 Kiruphagaran Thangaraju1, RoÂbert KiraÂly1, MaÂte A. DemeÂny1, JaÂnos AndraÂs MoÂtyaÂn1, a1111111111 Mo nika Fuxreiter1,2, LaÂszlo FeÂsuÈs1,3* a1111111111 a1111111111 1 Department of Biochemistry and Molecular Biology, Faculty of Medicine, University of Debrecen, a1111111111 Debrecen, Hungary, 2 MTA-DE Momentum Laboratory of Protein Dynamics, Faculty of Medicine, University a1111111111 of Debrecen, Debrecen, Hungary, 3 MTA-DE Stem cell, Apoptosis and Genomics Research Group of Hungarian Academy of Sciences, Faculty of Medicine, University of Debrecen, Debrecen, Hungary * [email protected] OPEN ACCESS Abstract Citation: Thangaraju K, KiraÂly R, DemeÂny MA, AndraÂs MoÂtyaÂn J, Fuxreiter M, FeÂsuÈs L (2017) Transglutaminases (TGMs) catalyze Ca2+-dependent transamidation of proteins with speci- Genomic variants reveal differential evolutionary constraints on human transglutaminases and point fied roles in blood clotting (F13a) and in cornification (TGM1, TGM3). The ubiquitous TGM2 towards unrecognized significance of has well described enzymatic and non-enzymatic functions but in-spite of numerous studies transglutaminase 2. PLoS ONE 12(3): e0172189. its physiological function in humans has not been defined. We compared data on non-syn- doi:10.1371/journal.pone.0172189 onymous single nucleotide variations (nsSNVs) and loss-of-function variants on TGM1-7 Editor: Richard L. Eckert, University of Maryland and F13a from the Exome aggregation consortium dataset, and used computational and School of Medicine, UNITED STATES biochemical analysis to reveal the roles of damaging nsSNVs of TGM2. -

B Inhibition in a Mouse Model of Chronic Colitis1
The Journal of Immunology Differential Expression of Inflammatory and Fibrogenic Genes and Their Regulation by NF-B Inhibition in a Mouse Model of Chronic Colitis1 Feng Wu and Shukti Chakravarti2 Fibrosis is a major complication of chronic inflammation, as seen in Crohn’s disease and ulcerative colitis, two forms of inflam- matory bowel diseases. To elucidate inflammatory signals that regulate fibrosis, we investigated gene expression changes under- lying chronic inflammation and fibrosis in trinitrobenzene sulfonic acid-induced murine colitis. Six weekly 2,4,6-trinitrobenzene sulfonic acid enemas were given to establish colitis and temporal gene expression patterns were obtained at 6-, 8-, 10-, and 12-wk time points. The 6-wk point, TNBS-w6, was the active, chronic inflammatory stage of the model marked by macrophage, neu- trophil, and CD3؉ and CD4؉ T cell infiltrates in the colon, consistent with the idea that this model is T cell immune response driven. Proinflammatory genes Cxcl1, Ccl2, Il1b, Lcn2, Pla2g2a, Saa3, S100a9, Nos2, Reg2, and Reg3g, and profibrogenic extra- cellular matrix genes Col1a1, Col1a2, Col3a1, and Lum (lumican), encoding a collagen-associated proteoglycan, were up-regulated at the active/chronic inflammatory stages. Rectal administration of the NF-B p65 antisense oligonucleotide reduced but did not abrogate inflammation and fibrosis completely. The antisense oligonucleotide treatment reduced total NF-B by 60% and down- regulated most proinflammatory genes. However, Ccl2, a proinflammatory chemokine known to promote fibrosis, was not down- regulated. Among extracellular matrix gene expressions Lum was suppressed while Col1a1 and Col3a1 were not. Thus, effective treatment of fibrosis in inflammatory bowel disease may require early and complete blockade of NF-B with particular attention to specific proinflammatory and profibrogenic genes that remain active at low levels of NF-B. -

The DNA Sequence and Comparative Analysis of Human Chromosome 20
articles The DNA sequence and comparative analysis of human chromosome 20 P. Deloukas, L. H. Matthews, J. Ashurst, J. Burton, J. G. R. Gilbert, M. Jones, G. Stavrides, J. P. Almeida, A. K. Babbage, C. L. Bagguley, J. Bailey, K. F. Barlow, K. N. Bates, L. M. Beard, D. M. Beare, O. P. Beasley, C. P. Bird, S. E. Blakey, A. M. Bridgeman, A. J. Brown, D. Buck, W. Burrill, A. P. Butler, C. Carder, N. P. Carter, J. C. Chapman, M. Clamp, G. Clark, L. N. Clark, S. Y. Clark, C. M. Clee, S. Clegg, V. E. Cobley, R. E. Collier, R. Connor, N. R. Corby, A. Coulson, G. J. Coville, R. Deadman, P. Dhami, M. Dunn, A. G. Ellington, J. A. Frankland, A. Fraser, L. French, P. Garner, D. V. Grafham, C. Grif®ths, M. N. D. Grif®ths, R. Gwilliam, R. E. Hall, S. Hammond, J. L. Harley, P. D. Heath, S. Ho, J. L. Holden, P. J. Howden, E. Huckle, A. R. Hunt, S. E. Hunt, K. Jekosch, C. M. Johnson, D. Johnson, M. P. Kay, A. M. Kimberley, A. King, A. Knights, G. K. Laird, S. Lawlor, M. H. Lehvaslaiho, M. Leversha, C. Lloyd, D. M. Lloyd, J. D. Lovell, V. L. Marsh, S. L. Martin, L. J. McConnachie, K. McLay, A. A. McMurray, S. Milne, D. Mistry, M. J. F. Moore, J. C. Mullikin, T. Nickerson, K. Oliver, A. Parker, R. Patel, T. A. V. Pearce, A. I. Peck, B. J. C. T. Phillimore, S. R. Prathalingam, R. W. Plumb, H. Ramsay, C. M. -

WO 2016/041614 Al 24 March 2016 (24.03.2016) P O P C T
(12) INTERNATIONAL APPLICATION PUBLISHED UNDER THE PATENT COOPERATION TREATY (PCT) (19) World Intellectual Property Organization International Bureau (10) International Publication Number (43) International Publication Date WO 2016/041614 Al 24 March 2016 (24.03.2016) P O P C T (51) International Patent Classification: DO, DZ, EC, EE, EG, ES, FI, GB, GD, GE, GH, GM, GT, A61K 39/395 (2006.01) G01N 33/574 (2006.01) HN, HR, HU, ID, IL, IN, IR, IS, JP, KE, KG, KN, KP, KR, KZ, LA, LC, LK, LR, LS, LU, LY, MA, MD, ME, MG, (21) International Application Number: MK, MN, MW, MX, MY, MZ, NA, NG, NI, NO, NZ, OM, PCT/EP20 15/00 1699 PA, PE, PG, PH, PL, PT, QA, RO, RS, RU, RW, SA, SC, (22) International Filing Date: SD, SE, SG, SK, SL, SM, ST, SV, SY, TH, TJ, TM, TN, 18 August 2015 (18.08.2015) TR, TT, TZ, UA, UG, US, UZ, VC, VN, ZA, ZM, ZW. (25) Filing Language: English (84) Designated States (unless otherwise indicated, for every kind of regional protection available): ARIPO (BW, GH, (26) Publication Language: English GM, KE, LR, LS, MW, MZ, NA, RW, SD, SL, ST, SZ, (30) Priority Data: TZ, UG, ZM, ZW), Eurasian (AM, AZ, BY, KG, KZ, RU, 62/05 1,530 17 September 2014 (17.09.2014) US TJ, TM), European (AL, AT, BE, BG, CH, CY, CZ, DE, DK, EE, ES, FI, FR, GB, GR, HR, HU, IE, IS, IT, LT, LU, (71) Applicant: MERCK PATENT GMBH [DE/DE]; Frank LV, MC, MK, MT, NL, NO, PL, PT, RO, RS, SE, SI, SK, furter Strasse 250, 64293 Darmstadt (DE). -

Transglutaminase 3: the Involvement in Epithelial Differentiation and Cancer
cells Review Transglutaminase 3: The Involvement in Epithelial Differentiation and Cancer Elina S. Chermnykh * , Elena V. Alpeeva and Ekaterina A. Vorotelyak Koltzov Institute of Developmental Biology Russian Academy of Sciences, 119334 Moscow, Russia; [email protected] (E.V.A.); [email protected] (E.A.V.) * Correspondence: [email protected] Received: 1 June 2020; Accepted: 26 August 2020; Published: 30 August 2020 Abstract: Transglutaminases (TGMs) contribute to the formation of rigid, insoluble macromolecular complexes, which are essential for the epidermis and hair follicles to perform protective and barrier functions against the environment. During differentiation, epidermal keratinocytes undergo structural alterations being transformed into cornified cells, which constitute a highly tough outermost layer of the epidermis, the stratum corneum. Similar processes occur during the hardening of the hair follicle and the hair shaft, which is provided by the enzymatic cross-linking of the structural proteins and keratin intermediate filaments. TGM3, also known as epidermal TGM, is one of the pivotal enzymes responsible for the formation of protein polymers in the epidermis and the hair follicle. Numerous studies have shown that TGM3 is extensively involved in epidermal and hair follicle physiology and pathology. However, the roles of TGM3, its substrates, and its importance for the integument system are not fully understood. Here, we summarize the main advances that have recently been achieved in TGM3 analyses in skin and hair follicle biology and also in understanding the functional role of TGM3 in human tumor pathology as well as the reliability of its prognostic clinical usage as a cancer diagnosis biomarker. This review also focuses on human and murine hair follicle abnormalities connected with TGM3 mutations. -
Inline-Supplementary-Material-6.Pdf
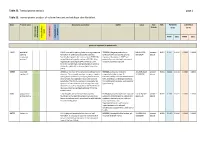
Table S3. Transcriptome analysis page 1 Table S3. Transcriptomic analysis of cultured mutant and wildtype skin fibroblast. Gene Protein name GeneCards annotation OMIM Locus Fold FDR PATIENTS CONTROLS - change (n=2) (n=4) ment apoptosis apoptosis Keratinocyte Keratinocyte inflammation differentiation Neurodevelop cell growth and growth cell FPKM [SD] FPKM [SD] genes up-regulated in patient cells ESRP1 epithelial ESRP1 is an mRNA splicing factor that regulates the *612959, the gene product is an 8:95653301 - present - 0.011 0.3547 0.0038 0.0000 0.0000 splicing formation of epithelial cell-specific isoforms. epithelial cell-type-specific splicing 95719694 absent regulatory Specifically regulates the expression of FGFR2-IIIb, regulator. Mutations in ESRP1 are protein 1 an epithelial cell-specific isoform of FGFR2. Also potentially associated with autosomal regulates the splicing of CD44, CTNND1, ENAH, recessive deafness type 109. three transcripts that undergo changes in splicing during the epithelial-to-mesenchymal transition (EMT). CERS3 ceramide CERS3 is a member of the ceramide synthase family #615023, autosomal recessive 15:100913143 - present - 0.011 0.1844 0.0118 0.0000 0.0000 synthase 3 of genes. The ceramide synthase enzymes regulate congenital ichthyosis type 9, 101085200 absent sphingolipid synthesis by catalyzing the formation characterized by collodian membrane at of ceramides from sphingoid base and acyl-CoA birth, acanthosis, orthohyperkeratosis, substrates. This family member is involved in the fine erythrodermic scales, palmoplantar synthesis of ceramides with ultra-long-chain acyl- hyperlinearity. moieties (ULC-Cers), important to the epidermis in its role in creating a protective barrier from the environment. GJB6 gap junction GJB6 encodes one of the connexin proteins. -

PB #ISAG2017 1 @Isagofficial #ISAG2017 #ISAG2017
Bioinformatics · Comparative Genomics · Computational Biology Epigenetics · Functional Genomics · Genome Diversity · Geno Genome Sequencing · Immunogenetics · Integrative Geno · Microbiomics · Population Genomics · Systems Biolog Genetic Markers and Selection · Genetics and Dis Gene Editing · Bioinformatics · Comparative Computational Biology · Epigenetics · Fun Genome Diversity · Genome Sequeng Integrative Genomics · Microbiom Population Genomics · Syste Genetic Markers and Sel Genetics and Disease Gene Editing · Bi O’Brien Centre for Science Bioinformati and O’Reilly Hall, University College Dublin, Dublin, Ireland ABSTRACTMINI PROGRAMME BOOK www.isag.us/2017 PB #ISAG2017 1 @isagofficial #ISAG2017 #ISAG2017 Contents ORAL PRESENTATIONS 1 Animal Forensic Genetics Workshop 1 Applied Genetics and Genomics in Other Species of Economic Importance 3 Domestic Animal Sequencing and Annotation 5 Genome Edited Animals 8 Horse Genetics and Genomics 9 Avian Genetics and Genomics 12 Comparative MHC Genetics: Populations and Polymorphism 16 Equine Genetics and Thoroughbred Parentage Testing Workshop 19 Genetics of Immune Response and Disease Resistance 20 ISAG-FAO Genetic Diversity 24 Ruminant Genetics and Genomics 28 Animal Epigenetics 31 Cattle Molecular Markers and Parentage Testing 33 Companion Animal Genetics and Genomics 34 Microbiomes 37 Pig Genetics and Genomics 40 Novel, Groundbreaking Research/Methodology Presentation 44 Applied Genetics of Companion Animals 44 Applied Sheep and Goat Genetics 45 Comparative and Functional Genomics 47 Genetics -

Computational Derivation of a Molecular Framework for Hair Follicle Biology from Disease Genes Received: 14 September 2017 Rachel K
www.nature.com/scientificreports OPEN Computational derivation of a molecular framework for hair follicle biology from disease genes Received: 14 September 2017 Rachel K. Severin1, Xinwei Li2, Kun Qian3, Andreas C. Mueller2 & Lynn Petukhova1,4 Accepted: 6 November 2017 Knowledge about genetic drivers of disease increases the efciency of interpreting patient DNA Published: xx xx xxxx sequence and helps to identify and prioritize biological points of intervention. Discoveries of genes with single mutations exerting substantial phenotypic impact reliably provide new biological insight, although such approaches tend to generate knowledge that is disjointed from the complexity of biological systems governed by elaborate networks. Here we sought to facilitate diagnostic sequencing for hair disorders and assess the underlying biology by compiling an archive of 684 genes discovered in studies of monogenic disorders and identifying molecular annotations enriched by them. To demonstrate utility for this dataset, we performed two data driven analyses. First, we extracted and analyzed data implicating enriched signaling pathways and identifed previously unrecognized contributions from Hippo signaling. Second, we performed hierarchical clustering on the entire dataset to investigate the underlying causal structure of hair disorders. We identifed 35 gene clusters representing genetically derived biological modules that provide a foundation for the development of a new disease taxonomy grounded in biology, rather than clinical presentations alone. This Resource will be useful for diagnostic sequencing in patients with diseases afecting the hair follicle, improved characterization of hair follicle biology, and methods development in precision medicine. In an age of precision medicine, faced with interpreting DNA sequence in the genomes of patients, it becomes critical to understand both the spectrum of genes that could be contributing to a particular clinical presentation, and the pathways that are mediating genetic efects. -

Identification of Candidate Aberrantly Methylated and Differentially
www.nature.com/scientificreports OPEN Identifcation of candidate aberrantly methylated and diferentially expressed genes in Esophageal squamous cell carcinoma Bao-Ai Han1,8, Xiu-Ping Yang4,8, Davood K Hosseini 3,5, Po Zhang6, Ya Zhang4, Jin-Tao Yu2, Shan Chen2, Fan Zhang7, Tao Zhou 2 ✉ & Hai-Ying Sun2,3 ✉ Aberrant methylated genes (DMGs) play an important role in the etiology and pathogenesis of esophageal squamous cell carcinoma (ESCC). In this study, we aimed to integrate three cohorts profle datasets to ascertain aberrant methylated-diferentially expressed genes and pathways associated with ESCC by comprehensive bioinformatics analysis. We downloaded data of gene expression microarrays (GSE20347, GSE38129) and gene methylation microarrays (GSE52826) from the Gene Expression Omnibus (GEO) database. Aberrantly diferentially expressed genes (DEGs) were obtained by GEO2R tool. The David database was then used to perform Gene ontology (GO) analysis and Kyoto Encyclopedia of Gene and Genome pathway enrichment analyses on selected genes. STRING and Cytoscape software were used to construct a protein-protein interaction (PPI) network, then the modules in the PPI networks were analyzed with MCODE and the hub genes chose from the PPI networks were verifed by Oncomine and TCGA database. In total, 291 hypomethylation-high expression genes and 168 hypermethylation-low expression genes were identifed at the screening step, and fnally found six mostly changed hub genes including KIF14, CDK1, AURKA, LCN2, TGM1, and DSG1. Pathway analysis indicated that aberrantly methylated DEGs mainly associated with the P13K-AKT signaling, cAMP signaling and cell cycle process. After validation in multiple databases, most hub genes remained signifcant. Patients with high expression of AURKA were associated with shorter overall survival. -
Mouse Tgm3 Conditional Knockout Project (CRISPR/Cas9)
https://www.alphaknockout.com Mouse Tgm3 Conditional Knockout Project (CRISPR/Cas9) Objective: To create a Tgm3 conditional knockout Mouse model (C57BL/6J) by CRISPR/Cas-mediated genome engineering. Strategy summary: The Tgm3 gene (NCBI Reference Sequence: NM_009374 ; Ensembl: ENSMUSG00000027401 ) is located on Mouse chromosome 2. 13 exons are identified, with the ATG start codon in exon 1 and the TGA stop codon in exon 13 (Transcript: ENSMUST00000110299). Exon 2~4 will be selected as conditional knockout region (cKO region). Deletion of this region should result in the loss of function of the Mouse Tgm3 gene. To engineer the targeting vector, homologous arms and cKO region will be generated by PCR using BAC clone RP23-111F6 as template. Cas9, gRNA and targeting vector will be co-injected into fertilized eggs for cKO Mouse production. The pups will be genotyped by PCR followed by sequencing analysis. Note: Mice homozygous for an ENU or null mutation exhibit rough-looking, curly hair. Null mutants display delayed skin barrier formation, loss of vibrissae, and brittle hairs. Exon 2 starts from about 0.38% of the coding region. The knockout of Exon 2~4 will result in frameshift of the gene. The size of intron 1 for 5'-loxP site insertion: 11279 bp, and the size of intron 4 for 3'-loxP site insertion: 1308 bp. The size of effective cKO region: ~2188 bp. The cKO region does not have any other known gene. Page 1 of 7 https://www.alphaknockout.com Overview of the Targeting Strategy Wildtype allele 5' gRNA region gRNA region 3' 1 2 3 4 5 13 Targeting vector Targeted allele Constitutive KO allele (After Cre recombination) Legends Exon of mouse Tgm3 Homology arm cKO region loxP site Page 2 of 7 https://www.alphaknockout.com Overview of the Dot Plot Window size: 10 bp Forward Reverse Complement Sequence 12 Note: The sequence of homologous arms and cKO region is aligned with itself to determine if there are tandem repeats. -

HBV DNA Integration and Clonal Hepatocyte Expansion in Chronic Hepatitis B Patients Considered Immune Tolerant
Accepted Manuscript HBV DNA Integration and Clonal Hepatocyte Expansion in Chronic Hepatitis B Patients Considered Immune Tolerant William S. Mason, Upkar S. Gill, Samuel Litwin, Yan Zhou, Suraj Peri, Oltin Pop, Michelle L.W. Hong, Sandhia Naik, Alberto Quaglia, Antonio Bertoletti, Patrick T.F. Kennedy PII: S0016-5085(16)34808-9 DOI: 10.1053/j.gastro.2016.07.012 Reference: YGAST 60585 To appear in: Gastroenterology Accepted Date: 7 July 2016 Please cite this article as: Mason WS, Gill US, Litwin S, Zhou Y, Peri S, Pop O, Hong MLW, Naik S, Quaglia A, Bertoletti A, Kennedy PTF, HBV DNA Integration and Clonal Hepatocyte Expansion in Chronic Hepatitis B Patients Considered Immune Tolerant, Gastroenterology (2016), doi: 10.1053/ j.gastro.2016.07.012. This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain. ACCEPTED MANUSCRIPT TITLE: HBV DNA Integration and Clonal Hepatocyte Expansion in Chronic Hepatitis B Patients Considered Immune Tolerant SHORT TITLE : Immunopathology in immune tolerant CHB AUTHORS: William S. Mason 1, Upkar S. Gill 2, Samuel Litwin 1, Yan Zhou 1, Suraj Peri 1, Oltin Pop 3, Michelle L.W. Hong 4, Sandhia Naik 5, Alberto Quaglia 3, Antonio Bertoletti 4 & Patrick T.F. -

PDF) S2 Table
RESEARCH ARTICLE Genomic variants reveal differential evolutionary constraints on human transglutaminases and point towards unrecognized significance of transglutaminase 2 Kiruphagaran Thangaraju1, RoÂbert KiraÂly1, MaÂte A. DemeÂny1, JaÂnos AndraÂs MoÂtyaÂn1, a1111111111 Mo nika Fuxreiter1,2, LaÂszlo FeÂsuÈs1,3* a1111111111 a1111111111 1 Department of Biochemistry and Molecular Biology, Faculty of Medicine, University of Debrecen, a1111111111 Debrecen, Hungary, 2 MTA-DE Momentum Laboratory of Protein Dynamics, Faculty of Medicine, University a1111111111 of Debrecen, Debrecen, Hungary, 3 MTA-DE Stem cell, Apoptosis and Genomics Research Group of Hungarian Academy of Sciences, Faculty of Medicine, University of Debrecen, Debrecen, Hungary * [email protected] OPEN ACCESS Abstract Citation: Thangaraju K, KiraÂly R, DemeÂny MA, AndraÂs MoÂtyaÂn J, Fuxreiter M, FeÂsuÈs L (2017) Transglutaminases (TGMs) catalyze Ca2+-dependent transamidation of proteins with speci- Genomic variants reveal differential evolutionary constraints on human transglutaminases and point fied roles in blood clotting (F13a) and in cornification (TGM1, TGM3). The ubiquitous TGM2 towards unrecognized significance of has well described enzymatic and non-enzymatic functions but in-spite of numerous studies transglutaminase 2. PLoS ONE 12(3): e0172189. its physiological function in humans has not been defined. We compared data on non-syn- doi:10.1371/journal.pone.0172189 onymous single nucleotide variations (nsSNVs) and loss-of-function variants on TGM1-7 Editor: Richard L. Eckert, University of Maryland and F13a from the Exome aggregation consortium dataset, and used computational and School of Medicine, UNITED STATES biochemical analysis to reveal the roles of damaging nsSNVs of TGM2. TGM2 and F13a Received: September 18, 2016 display rarer damaging nsSNV sites than other TGMs and sequence of TGM2, F13a and Accepted: February 1, 2017 TGM1 are evolutionary constrained.