Since Nitrogen Is at Least 5 Times More Soluble in Fat Than In
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Dysbarism - Barotrauma
DYSBARISM - BAROTRAUMA Introduction Dysbarism is the term given to medical complications of exposure to gases at higher than normal atmospheric pressure. It includes barotrauma, decompression illness and nitrogen narcosis. Barotrauma occurs as a consequence of excessive expansion or contraction of gas within enclosed body cavities. Barotrauma principally affects the: 1. Lungs (most importantly): Lung barotrauma may result in: ● Gas embolism ● Pneumomediastinum ● Pneumothorax. 2. Eyes 3. Middle / Inner ear 4. Sinuses 5. Teeth / mandible 6. GIT (rarely) Any illness that develops during or post div.ing must be considered to be diving- related until proven otherwise. Any patient with neurological symptoms in particular needs urgent referral to a specialist in hyperbaric medicine. See also separate document on Dysbarism - Decompression Illness (in Environmental folder). Terminology The term dysbarism encompasses: ● Decompression illness And ● Barotrauma And ● Nitrogen narcosis Decompression illness (DCI) includes: 1. Decompression sickness (DCS) (or in lay terms, the “bends”): ● Type I DCS: ♥ Involves the joints or skin only ● Type II DCS: ♥ Involves all other pain, neurological injury, vestibular and pulmonary symptoms. 2. Arterial gas embolism (AGE): ● Due to pulmonary barotrauma releasing air into the circulation. Epidemiology Diving is generally a safe undertaking. Serious decompression incidents occur approximately only in 1 in 10,000 dives. However, because of high participation rates, there are about 200 - 300 cases of significant decompression illness requiring treatment in Australia each year. It is estimated that 10 times this number of divers experience less severe illness after diving. Physics Boyle’s Law: The air pressure at sea level is 1 atmosphere absolute (ATA). Alternative units used for 1 ATA include: ● 101.3 kPa (SI units) ● 1.013 Bar ● 10 meters of sea water (MSW) ● 760 mm of mercury (mm Hg) ● 14.7 pounds per square inch (PSI) For every 10 meters a diver descends in seawater, the pressure increases by 1 ATA. -
The Mars Project: Avoiding Decompression Sickness on a Distant Planet
NASA/TM--2000-210188 The Mars Project: Avoiding Decompression Sickness on a Distant Planet Johnny Conkin, Ph.D. National Space Biomedical Research Institute Houston, Texas 77030-3498 National Aeronautics and Space Administration Lyndon B. Johnson Space Center Houston, Texas 77058-3696 May 2000 Acknowledgments The following people provided helpful comments and suggestions: Amrapali M. Shah, Hugh D. Van Liew, James M. Waligora, Joseph P. Dervay, R. Srini Srinivasan, Michael R. Powell, Micheal L. Gernhardt, Karin C. Loftin, and Michael N. Rouen. The National Aeronautics and Space Administration supported part of this work through the NASA Cooperative Agreement NCC 9-58 with the National Space Biomedical Research Institute. The views expressed by the author do not represent official views of the National Aeronautics and Space Administration. Available from: NASA Center for AeroSpace Information National Technical Information Service 7121StandardDrive 5285 Port Royal Road Hanover, MD 21076-1320 Springfield, VA 22161 301-621-0390 703-605-6000 This report is also available in electronic form at http://techreports.larc.nasa.gov/cgi-bin/NTRS Contents Page Acronyms and Nomenclature ................................................................................................ vi Abstract ................................................................................................................................. vii Introduction .......................................................................................................................... -

Decompression Sickness in Inside Attendants
SECTION VI 643 CHAPTER 2 DECOMPRESSION SICKNESS IN INSIDE ATTENDANTS PAUL J. SHEFFIELD AND CHRISTY J. PIRONE WHAT IS DECOMPRESSION SICKNESS? Decompression Sickness (DCS) Defined: DCS is an illness that occurs when environmental pressure is reduced sufficiently to cause gases that are dissolved in body tissues to evolve as bubbles. Primarily consisting of nitrogen, the bubbles evolve from solution when the inside attendant surfaces too fast for the body to compensate. Patients do not have the problem because the oxygen they breathe during hyperbaric oxygen treatment elimi- nates the nitrogen from their bodies. Signs and Symptoms of DCS: Bubbles that cause DCS can form in all parts of the body and the anatomic location accounts for the variety of signs and symptoms. (1) DCS can manifest itself from minor to life-threatening symptoms. Minor skin itching or tingling usually passes within 20 to 30 min- utes, and no treatment is necessary, all other forms of DCS are treated in the hyperbaric chamber with immediate compression and hyperbaric oxygen. “Bends pain” seen in about 90% of cases, may appear anywhere in the body, but is more frequent in legs or arms that were exercised during the exposure. Neurologic symptoms involving the brain or spinal cord occur in about 25% of cases, and are manifested by a wide variety of symptoms but mainly by headache, numbness, paralysis of an arm or leg, loss of sensation, vertigo, visu- al distortions or blindness, and extreme fatigue. Chokes is a rare but life-threat- ening respiratory disorder caused by gas emboli in the lungs, and manifested by wheezing, chest pain, or troublesome cough. -
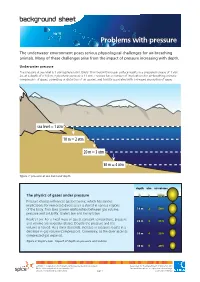
Problems with Pressure
background sheet Problems with pressure The underwater environment poses serious physiological challenges for air-breathing animals. Many of these challenges arise from the impact of pressure increasing with depth. Underwater pressure The pressure at sea level is 1 atmosphere (atm). Every 10 m below the ocean surface results in a pressure increase of 1 atm. So, at a depth of a 100 m, hydrostatic pressure is 11 atm. Pressure has a number of implications for air-breathing animals: compression of gases; squeezing or distortion of air spaces; and toxicity associated with increased absorption of gases. sea level = 1 atm 10 m = 2 atm 20 m = 3 atm 30 m = 4 atm figure 1: pressure at sea level and depth depth atm air volume The physics of gases under pressure 0 1 100% Pressure change influences gas behaviour, which has serious implications for immersed divers as air is stored in various regions of the body. Two laws govern relationships between gas volume, 1010m m 2 50% pressure and solubility: Boyle’s law and Henry’s law. Boyle’s Law: For a fixed mass of gas at constant temperature, pressure 2020m m 3 33% and volume are inversely related. Double the pressure and the volume is halved. As a diver descends, increase in pressure results in a decrease in gas volume (compression). Conversely, as the diver ascends 3030m m 4 25% compressed gas expands. figure 2: Boyle’s Law - impact of depth on pressure and volume 4040m m 5 20% ast0850 | Adaptations 6: Problems with pressure (background sheet) developed for the Department of Education WA © The University of Western Australia 2012 for conditions of use see spice.wa.edu.au/usage version 1.0 reviewed October 2012 page 1 Licensed for NEALS Henry’s Law: At constant temperature, the amount Risks for human divers of gas that dissolves in solution increases with gas pressure. -

Report of the Decompression Illness Adjunctive Therapy Committee of the Undersea and Hyperbaric Medical Society
REPORT OF THE DECOMPRESSION ILLNESS ADJUNCTIVE THERAPY COMMITTEE OF THE UNDERSEA AND HYPERBARIC MEDICAL SOCIETY Including Proceedings of the Fifty-Third Workshop of the Undersea and Hyperbaric Medical Society Chaired by Richard E. Moon, MD Editor Richard E. Moon, MD Copyright ©2003 Undersea and Hyperbaric Medical Society, Inc. 10531 Metropolitan Avenue Kensington, MD 20895, USA ISBN 0-930406-22-2 The views, opinions, and findings contained herein are those of the author(s) and should not be construed as an official Agency position, policy, or decision unless so designated by other official documentation. Authors Richard D. Vann, Ph.D. Assistant Research Professor of Anesthesiology Duke University Medical Center Director of Research, Divers Alert Network Durham, NC 27710 Edward D. Thalmann, M.D. Assistant Clinical Professor of Anesthesiology Assistant Clinical Professor of Occupational and Environmental Medicine Duke University Medical Center Assistant Medical Director, Divers Alert Network Durham, NC 27710 John M. Hardman, M.D. Professor and Chairman Dept. of Pathology John A. Burns School of Medicine University of Hawaii Honolulu, HI 96822 Ward Reed, M.D., M.P.H. Fellow in Undersea and Hyperbaric Medicine Duke University Medical Center Durham, NC 27710 W. Dalton Dietrich, Ph.D. Departments of Neurological Surgery and Neurology The Miami Project to Cure Paralysis University of Miami School of Medicine Miami, FL 33101 Frank Butler, CAPT, MC, USN Biomedical Research Director Naval Special Warfare Command Pensacola, FL Richard E. Moon, M.D. Professor of Anesthesiology Associate Professor of Medicine Medical Director, Center for Hyperbaric Medicine and Environmental Physiology Duke University Medical Center Medical Director, Divers Alert Network Durham, NC 27710 2 Joseph Dervay, M.D., M.M.S., F.A.C.E.P Flight Surgeon Medical Operations and Crew Systems NASA Johnson Space Center Houston, TX 77058 David S. -

Diving and the Risk of Barotrauma
S20 Thorax 1998;53(Suppl 2):S20±S24 Thorax: first published as 10.1136/thx.53.2008.S20 on 1 August 1998. Downloaded from Diving and the risk of barotrauma Erich W Russi Pulmonary Division, Department of Internal Medicine, University Hospital Zurich, Switzerland Introductory article Risk factors for pulmonary barotrauma in divers K Tetzlaff, M Reuter, B Leplow, M Heller, E Bettinghausen Study objectives. Pulmonary barotrauma (PBT) of ascent is a feared complication in compressed air diving. Although certain respiratory conditions are thought to increase the risk of suffering PBT and thus should preclude diving, in most cases of PBT, risk factors are described as not being present. The purpose of our study was to evaluate factors that possibly cause PBT. Design. We analyzed 15 consecutive cases of PBT with respect to dive factors, clinical and radiologic features, and lung function. They were compared with 15 cases of decompression sickness without PBT, which appeared in the same period. Results. Clinical features of PBT were arterial gas embolism (n=13), mediastinal emphysema (n=1), and pneumothorax (n=1). CT of the chest (performed in 12 cases) revealed subpleural emphysematous blebs in 5 cases that were not detected in preinjury and postinjury chest radiographs. A comparison of predive lung function between groups showed signi®cantly lower midexpiratory ¯ow rates at 50% and 25% of vital capacity in PBT patients (p<0.05 and p<0.02, respectively). Conclusions. These results indicate that divers with preexisting small lung cysts and/or end-expiratory ¯ow limitation may be at http://thorax.bmj.com/ risk of PBT. -
Redistribution of Decompression Stop Time from Shallow to Deep Stops Increases Incidence of Decompression Sickness in Air Decompression Dives
http://archive.rubicon-foundation.org Navy Experimental Diving Unit TA 04-12 321 Bullfinch Road NEDU TR 11-06 Panama City, FL 32407-7015 July 2011 REDISTRIBUTION OF DECOMPRESSION STOP TIME FROM SHALLOW TO DEEP STOPS INCREASES INCIDENCE OF DECOMPRESSION SICKNESS IN AIR DECOMPRESSION DIVES Navy Experimental Diving Unit Authors: Distribution Statement A: DAVID J. DOOLETTE Approved for public release; WAYNE A. GERTH distribution is unlimited. KEITH A. GAULT http://archive.rubicon-foundation.org THIS PAGE BLANK http://archive.rubicon-foundation.org Form Approved REPORT DOCUMENTATION PAGE OMB No. 0704-0188 Public reporting burden for this collection of information is estimated to average 1 hour per response, including the time for reviewing instructions, searching existing data sources, gathering and maintaining the data needed, and completing and reviewing this collection of information. Send comments regarding this burden estimate or any other aspect of this collection of information, including suggestions for reducing this burden to Department of Defense, Washington Headquarters Services, Directorate for Information Operations and Reports (0704-0188), 1215 Jefferson Davis Highway, Suite 1204, Arlington, VA 22202- 4302. Respondents should be aware that notwithstanding any other provision of law, no person shall be subject to any penalty for failing to comply with a collection of information if it does not display a currently valid OMB control number. PLEASE DO NOT RETURN YOUR FORM TO THE ABOVE ADDRESS. 1. REPORT DATE (DD-MM-YYYY) 2. REPORT TYPE 3. DATES COVERED (From - To) 22-07-2011 Technical Report Nov 2005 – Apr 2011 4. TITLE AND SUBTITLE 5a. CONTRACT NUMBER Redistribution of decompression stop time from shallow to deep stops increases incidence of decompression sickness in air decompression dives 5b. -

Decompression Illness in United States Air Force: High Risk Occupations
Wright State University CORE Scholar Master of Public Health Program Student Publications Master of Public Health Program 2015 Decompression Illness in United States Air Force: High Risk Occupations Jaime Rojas Wright State University - Main Campus Follow this and additional works at: https://corescholar.libraries.wright.edu/mph Part of the Public Health Commons Repository Citation Rojas, J. (2015). Decompression Illness in United States Air Force: High Risk Occupations. Wright State University, Dayton, Ohio. This Master's Culminating Experience is brought to you for free and open access by the Master of Public Health Program at CORE Scholar. It has been accepted for inclusion in Master of Public Health Program Student Publications by an authorized administrator of CORE Scholar. For more information, please contact library- [email protected]. Running head: DECOMPRESSION ILLNESS 1 Decompression Illness in United States Air Force High Risk Occupations Jaime Rojas Wright State University DECOMPRESSION ILLNESS 2 Table of Contents Abstract ............................................................................................................................................3 Introduction ......................................................................................................................................4 Purpose Statement ............................................................................................................................4 Literature Review.............................................................................................................................4 -

Diving Injuries and Dysbarism – January 2018
CrackCast Show Notes – Diving Injuries and Dysbarism – January 2018 www.canadiem.org/crackcast Chapter 143 (Ch. 135 9th) – Diving Injuries and Dysbarism Episode Overview: 1. List 5 potential injuries in scuba diving other than dysbarisms 2. What is the ideal gas law 3. Describe the following laws: a. Pascal’s Law b. Boyle’s Law c. Charles’ Law d. General Gas Law e. Dalton’s Law f. Henry’s Law 4. Describe the basic pathophysiology of Decompression Sickness 5. List 5 potential injuries a diver can sustain in descent, at depth, and in ascent. 6. Describe the difference between MEBT, IEBT, ABV and Middle Ear DCS 7. What is nitrogen narcosis? How does it present? 8. What is the pathophysiology of decompression sickness? a. List 6 risk factors for DCS b. Describe the 2 types of DCS (clinical features) 9. List 5 potential pathologies associated with pulmonary barotrauma 10. Describe the management of DCS. What other diving disorders require recompression therapy? a. How would you manage a patient requiring recompression in the pre- hospital and ED environment (pre-hyperbaric oxygen treatment)? 11. What is an Arterial Gas Embolism? How would you differentiate between AGE and pulmonary DCS? Wisecracks: 1) Describe memory aids for the gas laws (for all of us mathematically challenged folks) a) When is there the greatest risk of barotrauma - in shallow or deep water? 2) What are key aspects of the diving history 3) What are the types of gas-mixture injuries? 4) What are the indications for re-compression (hyperbaric treatment)? How does it work? 5) What complications of asthma are associated with diving? 6) List five causes of dizziness associated with diving. -

Gas Bubbles May Not Be the Underlying Cause of Decompression Illness – the At-Depth Endothelial Dysfunction Hypothesis
Medical Hypotheses 72 (2009) 389–392 Contents lists available at ScienceDirect Medical Hypotheses journal homepage: www.elsevier.com/locate/mehy Gas bubbles may not be the underlying cause of decompression illness – The at-depth endothelial dysfunction hypothesis Leigh A. Madden a,*, Gerard Laden b a Postgraduate Medical Institute, University of Hull, Cottingham Road, Hull HU6 7RX, UK b Hull Hyperbaric Unit, Hull and East Riding Hospital, Anlaby, HU10 7AZ, UK article info summary Article history: Gas formed in tissues and the circulating blood due to decompression is thought to be a significant factor Received 28 October 2008 in the progression of decompression illness (DCI). DCI is a potential problem for a growing population of Accepted 7 November 2008 professional and recreational divers. We hypothesise that these gas bubbles are not the causative agent in progression of DCI, rather an exacerbating factor. Endothelial dysfunction caused by a temporary loss of haemostasis due to increased total oxidant status is postulated to be the cause in this at-depth endothe- lial dysfunction hypothesis. Breathing oxygen at any pressure increases the oxidant status in the circula- tion causing vasoconstriction; this increase can be prevented by antioxidants, such as Vitamin C, maintaining haemostasis and preventing activation of endothelium, leukocyte recruitment and subse- quent localised inflammation. Bubbles have the potential to exacerbate the situation on decompression by damaging the vascular endothelium either through ischemia/reperfusion, physical contact with the endothelium or by an increase in shear stress. Furthermore, this damage may manifest itself in the release of endothelial membrane fragments (microparticles). Crown Copyright Ó 2008 Published by Elsevier Ltd. -

Following Decompression Illness (DCI) Case Report, by Clifton M
Medical Certification of Pilots following Decompression Illness (DCI) Case Report, by Clifton M. Nowell, DO According to the Divers Alert Network, approximately 1,000 decompression-related incidents occur yearly.1 SCUBA diving introduces an abnormal environment where pressure and gases play vital roles. Although not a common event, much research has gone into laying out ways to prevent decompression illness and how to effectively treat it when it occurs. History 45-year-old male airline transport pilot with 5,100 the locale of the bubble, whereas arterial gas emboli enter the A total hours of flight time applied for a second-class med- lung circulation, traveling through the arteries and causing ical recertification 3 months following a barotrauma event that tissue damage at a distance by blocking blood flow through resulted from a rescue attempt of another diver. the smaller vessels.3 The airman suffered barotrauma as a result of a rapid ascent Of greatest concern following a decompressing illness and from approximately 60 feet deep in 20 seconds. He made this flying is the sequelae that may ensue. Sudden incapacitation ascent as he noted another diver, apparently unconscious, float- is not of great concern because the inciting event has passed, ing to the surface. Following the rescue, he entered the boat, and the airman would have received proper treatment. Deficits, feeling pain and heaviness in his right arm, and numbness in especially neurological, are a major concern. Evaluation of the the right cheek. Approximately 3 minutes later, he experienced airman’s ability to perform the tasks associated with flying is what was described as “pins and needles” over his entire body. -
Diving Medicine & Recompression Chamber Operations
VOLUME 5 Diving Medicine & Recompression Chamber Operations 17 Diagnosis and Treatment of Decompression Sickness and Arterial Gas Embolism 18 Recompression Chamber Operation Appendix 5A Neurological Examination Appendix 5B First Aid Appendix 5C Hazardous Marine Creatures U.S. NAVY DIVING MANUAL Change A PAGE LEFT BLANK INTENTIONALLY Volume 5 - Table of Contents Chap/Para Page 17 DIAGNOSIS AND TREATMENT OF DECOMPRESSION SICKNESS AND ARTERIAL GAS EMBOLISM 17-1 INTRODUCTION . 17-1 17-1 1 . Purpose . 17-1 17-1 2 . Scope . 17-1 17-2 MANNING REQUIREMENTS . 17-1 17-2 .1 Recompression Chamber Team . 17-1 17-2.2 Diving Officer . 17-2 17-2 .3 Master Diver . 17-3 17-2 .4 Chamber Supervisor . 17-3 17-2.5 Diving Medical Officer . 17-3 17-2 .5 .1 Prescribing and Modifying Treatments . 17-4 17-2 .6 Inside Tender/DMT . 17-4 17-2 .7 Outside Tender . 17-5 17-2 .8 Emergency Consultation . 17-5 17-3 ARTERIAL GAS EMBOLISM . 17-6 17-3 .1 Diagnosis of Arterial Gas Embolism . 17-6 17-3 .1 .1 Symptoms of AGE . 17-7 17-3 .2 Treating Arterial Gas Embolism . 17-7 17-3 .3 Resuscitation of a Pulseless Diver . 17-7 17-3 .3 .1 Evacuation not Feasible . 17-8 17-4 DECOMPRESSION SICKNESS . 17-8 17-4 .1 Diagnosis of Decompression Sickness . 17-9 17-4 .2 Symptoms of Type I Decompression Sickness . 17-9 17-4 .2 .1 Musculoskeletal Pain-Only Symptoms . 17-9 17-4 .2 .2 Cutaneous (Skin) Symptoms . 17-11 17-4 .2 .3 Lymphatic Symptoms .