Low-Density Lipoprotein Particle Diameter and Mortality: the Ludwigshafen Risk and Cardiovascular Health Study
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Leisure Offers in Heidelberg and Surroundings
Leisure offers in Heidelberg and surroundings Museums ► Reiss-Engelhorn-Museum D5, Mannheim ► Heidelberg Castle https://www.rem-mannheim.de Schloss Heidelberg Opening hours: Tu.-Su.: 11:00 - 18:00 https://www.schloss-heidelberg.de/start Entry fee: 3€ regular, 2€ discounted Opening hours: Mo. to Su. 08:00 – 18:00 ► Kunsthalle Mannheim Entry fee: 8€ regular, 4€ discounted. Friedrichplatz 4, Mannheim https://www.kuma.art/de ► Kurpfälzisches Museum Opening hours: Tu. to Su.: 10:00 – 18:00 Hauptstraße 97, Heidelberg. Entry fee: 6€ https://www.museum- ► Technomuseum Mannheim heidelberg.de/1360820.html Museumsstraße 1, Mannheim Opening hours: https://www.technoseum.de/ Tu. to Su.: 10:00 - 18:00 Opening hours: Mo. to Su. 09:00 – 17:00 Entry fee: 6€ regular, 4.5€ discounted Entry fee: 9€ regular, 6€ discounted ► Sammlung Prinzhorn Voßstraße 2, Heidelberg ► Wilhelm-Hack-Museum Ludwigshafen https://prinzhorn.ukl-hd.de/sammlung- Berliner Straße 23, Ludwigshafen am Rhein prinzhorn/ https://www.wilhelmhack.museum/ Opening hours: We.: 15:00 - 20:00 Opening hours: Th., Fr.: 13:00 - 17:00 Tu., We., Fr.: 11:00 – 18:00 Sa.: 12:00 - 17:00 Th.: 11:00 – 20:00 Entry fee: 5€ regular, 3€ discounted Sa. and Su.: 10:00 – 18:00 Entry fee: 7€ regular, 5€ discounted, ► Körperwelten Saturdays for free. Poststraße 36/5, Heidelberg https://koerperwelten.de/stadt/heidelberg/ ► Kunstverein Ludwigshafen Opening hours: Berliner Straße 23, Ludwigshafen am Rhein Mo., Tu., Th. and Fr.: 09:00 - 18:00 https://www.wilhelmhack.museum/ We.: 9:00 – 21:00 Opening hours: Sa. and Su.: 10:00 – 18:00 Tu. to Fr.: 12:00 – 18:00 Entry fee: 17€ regular, 14€ discounted, 11€ Sa. -

RE 4/14 Frankfurt - Mainz - Worms - Ludwigshafen - Mannheim/Karlsruhe Linie 660 Anschluss Zwischen Zwei Zügen Ist in Mainz Hbf Nur Bei Einem Übergang Von Min
RE 4/14 Frankfurt - Mainz - Worms - Ludwigshafen - Mannheim/Karlsruhe Linie 660 Anschluss zwischen zwei Zügen ist in Mainz Hbf nur bei einem Übergang von min. 7 Minuten gesichert. Am 24. und 31.12. Verkehr wie an Samstagen. Montag - Freitag Linie RE 14 RE 4 RE 14 RE 4 RE 4 RE 14 RE 4 RE 4 RE 14 RE 4 RE 4 RE 14 RE 4 RE 4 RE 14 RE 4 RE 14 RE 4 RE 4 RE 4 Zugnummer 4753 4471 4751 14473 4473 4491 29692 4475 4493 14477 4477 4495 14479 4479 4497 4481 4757 4487 29694 4483 Frankfurt, Hauptbahnhof 6.08 7.38 8.38 9.38 10.38 11.38 12.38 13.39 14.38 15.38 16.38 17.38 Frankfurt-Höchst 6.16 7.46 8.46 9.46 10.46 11.46 12.46 13.47 14.46 15.46 16.46 17.46 Hochheim (Main) 6.30 7.58 8.58 9.58 10.58 11.58 12.58 13.58 14.58 15.58 16.58 17.58 Mainz, Hauptbahnhof an 6.43 8.11 9.11 10.11 11.11 12.11 13.11 14.11 15.11 16.11 17.11 18.11 Mainz, Hauptbahnhof ab 5.45 6.52 8.13 9.13 10.13 11.17 12.13 13.17 14.13 15.17 16.13 16.17 17.17 18.13 Mainz, Römisches Theater 16.22 Nierstein 16.32 Oppenheim 16.35 Guntersblum 16.40 Osthofen 6.07 16.45 Worms, Hauptbahnhof an 6.14 7.19 8.39 9.40 10.39 11.44 12.39 13.44 14.39 15.44 16.39 16.52 17.44 18.39 Worms, Hauptbahnhof ab 6.15 7.20 8.40 9.41 10.40 11.45 12.40 13.45 14.40 15.45 16.40 16.53 17.45 18.40 Bobenheim 6.20 7.24 Frankenthal, Hauptbahnhof an 6.24 7.27 8.46 9.46 10.46 11.52 12.46 13.52 14.46 15.52 16.46 16.59 17.52 18.46 Frankenthal, Hauptbahnhof ab 6.25 7.28 8.47 9.47 10.47 11.52 12.47 13.53 14.47 15.52 16.47 17.00 17.52 18.47 Frankenthal, Süd 6.27 7.30 Mannheim, Hauptbahnhof 6.47 Ludwigshafen, Mitte 6.50 Ludwigshafen, -

Bitkom Smart City Index 2020 Berücksichtigt Alle 81 Deutschen Großstädte (100.000 Einwohner Und Mehr)
Smart City Index 2020 Ausführliche Ergebnisse www.bitkom.org Smart City Index 2019 2 Impressum Herausgeber Bitkom e. V. Bundesverband Informationswirtschaft, Telekommunikation und neue Medien e. V. Albrechtstraße 10 | 10117 Berlin Ansprechpartner Svenja Hampel | Projektleiterin Smart City Index T 030 27576 -560 | [email protected] Satz & Layout Sabrina Flemming | Bitkom Titelbild © FotoStuss – adobe.stock.com Copyright Bitkom 2020 Diese Publikation stellt eine allgemeine unverbindliche Information dar. Die Inhalte spiegeln die Auffassung im Bitkom zum Zeitpunkt der Veröffentlichung wider. Obwohl die Informationen mit größtmöglicher Sorgfalt erstellt wurden, besteht kein Anspruch auf sachliche Richtigkeit, Vollständigkeit und / oder Aktualität, insbesondere kann diese Publikation nicht den besonderen Umständen des Einzelfalles Rechnung tragen. Eine Verwendung liegt daher in der eigenen Verantwortung des Lesers. Jegliche Haftung wird ausgeschlossen. Alle Rechte, auch der auszugs- weisen Vervielfältigung, liegen beim Bitkom. Smart City Index 2019 3 Inhaltsverzeichnis Inhaltsverzeichnis Einleitung ________________________________________________________________________ 4 1 Gesamtergebnisse ____________________________________________________________ 9 2 Verwaltung _________________________________________________________________ 14 3 IT- und Kommunikation _______________________________________________________ 19 4 Energie und Umwelt __________________________________________________________ 24 5 Mobilität ___________________________________________________________________ -

Metropolitan Areas in Europe
BBSR-Online-Publikation, Nr. 01/2011 Metropolitan areas in Europe Imprint Published by Federal Institute for Research on Building, Urban Affairs and Spatial Development (BBSR) within the Federal Office for Building and Regional Planning (BBR), Bonn Editing Jürgen Göddecke-Stellmann, Dr. Rupert Kawka, Dr. Horst Lutter, Thomas Pütz, Volker Schmidt-Seiwert, Dr. Karl Peter Schön, Martin Spangenberg In cooperation with Gabriele Costa, Dirk Gebhardt, Heike Kemmerling, Claus Schlömer, Stefan Schmidt, Marisa Trimborn Translation Beatrix Thul Reprint and Copying All rights reserved Quotation BBSR: Metropolitan areas in Europe. BBSR-Online-Publikation 01/2011. Eds.: Federal Institute for Research on Building, Urban Affairs and Spatial Development (BBSR) within the Federal Office for Building and Regional Planning (BBR), Bonn, January 2011. ISSN 1868-0097 © BBSR January 2011 Metropolitan areas in Europe 2 Acknowledgement The authors would like to thank Professor Michael Parkinson, Liverpool John Moores University, for useful suggestions which help improve the translation. Acknowledgement BBSR-Online-Publikation Nr. 01/2011 Metropolitan areas in Europe 3 Table of contents 1 Metropolitan regions – an evidence-based policy programme 2 Metropolitan functions – the key towards analysing metropolitan areas 2.1 Metropolitan functions: theoretical backgrounds and models 2.2 Redefining metropolitan functions 3 From theory towards empiricism: metropolitan functions – indicators and measuring concept 4 Locations and spatial distribution of metropolitan functions -

Die Grössten Arbeitgeber in Rheinland-Pfalz 2019 Betriebe Ab 500 Beschäftigte
DIE GRÖSSTEN ARBEITGEBER IN RHEINLAND-PFALZ 2019 BETRIEBE AB 500 BESCHÄFTIGTE . Vorwort Die vorliegende Übersicht „Die größten Arbeitgeber in Rheinland-Pfalz 2019” stellt beschäftigungs - starke Unternehmen aus Industrie, Handel und Dienstleistung vor und gibt diesen die Möglichkeit, ihre wirtschaftliche Bedeutung in der Öffentlichkeit zu präsentieren. Die 137 Unternehmen beschäftigen zwischen 500 und 35.000 Personen – in der Summe sind es rund 221.000 Arbeitsplätze. In den Betrieben arbeiten demzufolge rund 16 Prozent der landesweit rund 1,4 Mio. sozialversicherungspflichtig Beschäftigten. Darüber hinaus tragen diese großen Unter - nehmen wesentlich zur Wertschöpfung und auch mittelbar zum wirtschaftlichen Wohlstand der Region bei, indem sie Arbeitsplätze bei Lieferanten und Dienstleistern sichern. Die Industrie hat mit 83 Unternehmen einen bedeutenden Anteil an den größten Arbeitgebern in Rheinland-Pfalz. Hohe Beschäftigtenzahlen finden sich vor allem bei den Automobilzulieferern, dem Maschinen- und Fahrzeugbau sowie den Herstellern von Chemie-, Kunststoff- und Pharmaprodukten. Im Handel finden sich größere Arbeitgeber vor allem im Lebensmittelhandel, Bau- und Heimwerker - bedarf sowie Möbelhandel. Im Dienstleistungsbereich sind größere Belegschaften insbesondere im Gesundheitswesen, bei Kreditinstituten und Finanzdienstleistern anzutreffen. Befragt wurden IHK-Mitgliedsunternehmen ab 500 Mitarbeiter, die entweder ihren Hauptsitz, eine Zweigniederlassung oder eine große Einzelbetriebsstätte in Rheinland-Pfalz unterhalten. Die Angaben zu den Beschäftigtenzahlen (Vollzeit und Teilzeit) wurden von den meisten Unternehmen zum 1. März 2019 erhoben und sind für Rheinland-Pfalz, Deutschland und die gesamte Welt kumuliert. Nicht erfasst wurden Mini-Jobber, Aushilfen und andere Formen geringfügiger Beschäftigung. Die Liste wird alle drei Jahre aktualisiert. Die Übersicht beruht auf den freiwilligen Angaben der Unternehmen und erhebt keinen Anspruch auf Vollständigkeit. Die Auflistung wurde aus öffentlich zugänglichen Quellen ergänzt. -

Investment Locations Germany 2019 Residential – Rents and Yields
Investment locations Germany 2019 Residential – rents and yields The situation on the German housing markets is a reflection of social changes and economic consequences. All in all, a high center-focused and demand-based development can be seen, while at the same time the heterogeneity of supply is increasing. Urbanity and the desire to live in cities result in a different price ratio. The scarcity of supply is increasingly being countered by means of post-consolidation measures and neighbourhood development. The view outside the conurbations is different: less the lack of building land than emigration shapes these housing markets. Kiel 7.85 10.50 4.40 Rostock 7.13 10.56 4.50 Lübeck 8.01 10.21 4.60 Schwerin 7.09 Hamburg 8.58 12.00 Lüneburg 5.50 16.29 2.70 8.99 11.05 Oldenburg 4.30 8.08 10.16 Bremen 4.30 9.06 11.66 4.70 10.13 17.00 2.40 8.67 8.52 Berlin 11.31 11.23 7.76 4.10 4.90 9.76 Hanover Wolfsburg Potsdam 4.90 Osnabrück Reckling- 9.84 Braunschweig 12.16 hausen Hildesheim 10.07 7.02 3.80 5.79 9.14 7.90 12.72 6.40 10.21 Magdeburg 7.42 3.80 4.50 6.20 8.20 4.90 5.97 Bielefeld 5.30 Herne Münster 7.77 6.95 Detmold 6.23 5.30 6.03 6.08 7.91 7.77 10.75 Gütersloh Cottbus 4.70 7.27 6.00 5.60 7.00 6.34 Paderborn 8.73 7.26 6.04 Oberhausen 7.70 8.92 11.10 6.46 6.00 7.43 Göttingen 4.90 7.49 5.00 9.39 6.80 5.97 8.73 5.30 4.90 8.18 Hamm 7.19 5.70 Bochum Dortmund 9.74 7.74 6.84 Duisburg 4.70 9.43 8.74 Essen 6.37 Ratingen 5.00 Leipzig 5.30 Krefeld Wuppertal 8.11 5.30 Kassel 7.37 Remscheid Mönchen- 10.49 Dusseldorf Dusseldorf 6.05 3.60 gladbach Solingen -

Fahrplan Stadtbahnlinie S3
Germersheim - Speyer - Schifferstadt - Ludwigshafen - Mannheim - S3 Heidelberg - Wiesloch-Walldorf - Bad Schönborn - Bruchsal - Karlsruhe Montag - Freitag LINIE S3 S4 S32 S3 S4 S3 S4 S3 S4 S31 S3 S4 S32 S3 S4 S31 S3 S4 S31 S3 S4 S3 S4 S31 S3 S4 S32 S3 S4 S32 S3 S4 S31 S3 S4 S31 S3 S4 ZUGGATTUNG S S S S S S S S S S S S S S E S E S S S S S S S ZUGNUMMER 38301 85128 38203 38305 38403 85022 38307 80104 38311 85028 38313 85030 38211 38315 85032 38317 85036 38319 85040 38325 85042 38327 85044 38329 VERKEHRSHINWEIS D Germersheim Bf 4.10 5.57 Lingenfeld 4.13 6.00 ▼ Heiligenstein (Pfalz) 4.17 6.04 ▼ Berghausen (Pfalz) 4.19 6.06 ▼ Speyer Hbf an 4.23 6.09 ▼ Speyer Hbf ab 4.24 6.10 ▼ Speyer Nord/West 4.26 6.12 ▼ Schifferstadt Süd 4.30 6.16 ▼ Schifferstadt an 4.33 6.20 ▼ Schifferstadt ab 4.37 5.42 6.27 6.47 7.00 7.25 ▼ Ludwigshafen (Rh) Hbf 1.04 4.15 4.51 5.29 5.54 6.40 6.59 7.20 7.42 ▼ Mannheim Hbf 0.40 1.10 4.21 4.57 5.36 6.02 6.15 6.46 7.07 7.30 7.57 ▼ Mannheim Arena/Maimarkt 0.44 1.14 4.25 5.02 5.40 6.07 6.20 6.51 7.11 8.01 ▼ Heidelberg Hbf an 0.56 1.26 4.37 5.15 5.52 6.23 6.32 7.03 7.23 7.44 8.16 ▼ Heidelberg Hbf ab 0.57 4.07 4.39 5.16 5.43 5.59 6.33 6.47 7.06 7.25 7.48 8.18 ▼ HD Kirchheim/Rohrbach 1.00 4.10 4.42 5.19 5.46 6.02 6.36 6.50 7.09 7.28 7.51 8.21 ▼ St Ilgen-Sandhausen 1.03 4.13 4.45 5.22 5.49 6.05 6.39 6.53 7.12 7.31 7.54 8.24 ▼ Wiesloch-Walldorf 1.07 4.17 4.49 5.27 5.53 6.09 6.43 6.57 7.16 7.35 7.58 8.28 ▼ Rot-Malsch 1.11 4.21 4.53 5.31 5.57 6.13 6.47 7.01 7.20 7.39 8.02 8.32 Bad Schönborn-Kronau 1.14 4.23 4.56 5.34 6.00 6.16 6.49 7.03 7.22 7.42 8.05 8.34 Bad Schönborn Süd 1.16 4.26 4.58 5.36 6.02 6.18 6.52 7.06 7.25 7.44 8.07 8.37 Ubstadt-Weiher 1.20 4.30 5.01 5.39 6.06 6.21 6.55 7.09 7.28 7.48 8.10 8.40 Bruchsal Bf an 1.24 4.34 5.05 5.43 6.11 6.25 6.59 7.13 7.32 7.53 8.14 8.44 Bruchsal Bf ab 1.29 1.48 4.35 5.15 5.44 6.02 6.12 6.16 6.26 6.44 7.00 7.04 7.16 7.23 7.33 7.47 7.53 8.06 8.17 8.26 8.44 Bruchsal Gew. -

Turnierzeitung
Turnierzeitung Löwenturnier 2017 28. – 29. Oktober 2017 Turn- und Fecht-Club 1861 e.V. Ludwigshafen Turn- und Fecht-Club 1861 e.V. Ludwigshafen Löwenturnier 2017 Herzlich Willkommen in Ludwigshafen! Liebe Gäste, wir freuen uns euch beim Löwenturnier 2017 willkommen zu heißen. Vor uns liegt ein Turnier mit hochklassigen und spannenden Spielen! Diese Turnierzeitung soll euch als Informationsgrundlage und Orientierungshilfe während des Turniers dienen. Sofern ihr weitere Fragen und Anregungen habt, könnt ihr natürlich immer auf uns zukommen. Wir helfen gerne weiter. Wir wünschen euch ein schönes und erfolgreiches Turnier! Euer Orga-Team Inhalt 1. Anfahrt und Spielorte ......................................................................................................... 3 2. Infopunkt und Betreuerempfang ........................................................................................ 4 3. Gruppen und Mannschaften ............................................................................................... 4 4. Spielplan ............................................................................................................................ 13 5. Kabinen ............................................................................................................................. 14 6. Bewirtung .......................................................................................................................... 15 7. Abendessen ...................................................................................................................... -

Claims Resolution Tribunal
CLAIMS RESOLUTION TRIBUNAL In re Holocaust Victim Assets Litigation Case No. CV96-4849 Certified Denial to Claimant [REDACTED] in re Accounts of Max Löwenstein Claim Number: 205882/SB This Certified Denial is based on the claim of [REDACTED] (the Claimant ) to the published accounts of Max Löwenstein (the Account Owner ) at the [REDACTED] (the Bank ). All denials are published, but where a claimant has requested confidentiality, as in this case, the names of the claimant, any relatives of the claimant other than the account owner, and the bank have been redacted. Information Provided by the Claimant The Claimant submitted a Claim Form asserting that his grandfather, Max Löwenstein, who was born on 21 May 1896 in Trier, Germany, and was married to [REDACTED], owned a Swiss bank account. The Claimant stated that his grandfather, who was Jewish, was a doctor of law who resided in Trier and Ludwigshafen, Germany. The Claimant further stated that his father fled Germany in 1938, initially to Luxembourg, then Paris and Toulouse, France and finally Spain, returning to France after the end of the Second World War. The Claimant stated that his grandfather died on 21 January 1967, in Toulouse. The Claimant stated that he was born on 24 March 1947 in Vincennes, France. Information Available in the Bank s Records The CRT notes that the Claimant submitted a claim to an account belonging to his relative, Max Löwenstein. The auditors who carried out the investigation to identify accounts of Victims of Nazi Persecution pursuant to instructions of the Independent Committee of Eminent Persons ( ICEP or the ICEP Investigation ) reported two accounts whose owner s name matches that provided by the Claimant. -
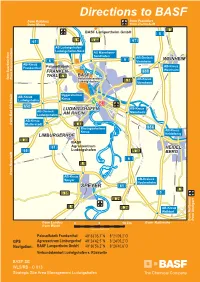
GPS Directions to BASF
WORMS B 47 Directions to BASF B 47from Koblenz from Frankfurt from MainzAS Worms from Darmstadt B 3 BASF Lampertheim GmbH R 5 h e i 61 B 9 n B 44 67 AS Ludwigshafen/ Ludwigshafen-Nord AS Mannheim- Sandhofen 6 AB-Dreieck WEINHEIM 6 Viernheim AB-Kreuz AB-Kreuz Frankenthal Palusolfabrik FRANKEN- 659 Weinheim THAL B 9 BASF fom Saarbrücken from Kaiserslautern Verbundstandort B 38 AB-Kreuz Ludwigshafen Viernheim Oggersheimer AB-Kreuz Kreuz Ludwigshafen 650 LUDWIGSHAFEN AB-Kreuz N AB-Dreieck e Mannheim c AM RHEIN k Bad Dürkheim Ludwigshafen a r AB-Kreuz from Mutterstadt B 44 Rheingönheimer 656 Kreuz AB-Kreuz LIMBURGERHOF Heidelberg B 38 BASF 61 Agrarzentrum HEIDEL- 65 Ludwigshafen B 36 BERG 6 B 9 Neustadt n i e from h AB-Kreuz R Speyer AB-Dreieck Hockenheim SPEYER 61 B 3 B 39 5 B 39 B 9 B 36 AB-Kreuz Walldorf from Stuttgart from Heilbronn from Landau 0 5 10 km from Karlsruhe from Wörth Copyright: BASF SE Palusolfabrik Frankenthal 49°33’05,7’’N 8°21’09,2’’O GPS Agrarzentrum Limburgerhof 49°24’42,5’’N 8°24’05,2’’O Navigation: BASF Lampertheim GmbH 49°36’56,2’’N 8°26’40,6’’O Verbundstandort Ludwigshafen s. Rückseite BASF SE WLS/RB - C 013 Strategic Site Area Management Ludwigshafen from AB-Kreuz from Worms Legend: Frankenthal B 9 N P parking P AS Ludwigshafen/ N T P parking Ludwigshafen-Nord Langgartenstraße Logistic Transfer Center, A6 North Harbour,SewageTechnical Treatment Engineering, T 5 gate T 49°33’08,5’’N Logistic CenterCenter, 8°24’03,8’’O IT-Service Q 920 Sewage from AB-Kreuz Treatment Viernheim BASF- Kleingartenbauverein Plant 7 - 8 Pfingst- 6 weide P H Nacht- Ammoniak- 11 weide H str. -

10 Golden Rules for a Safe Home • Keep the Door to Your Building Closed During the Day. Always Check Who Wants to Enter the Bu
Information on Burglary Prevention Information on Burglary Prevention Information on Burglary Prevention Information on Burglary Prevention 10 Golden Rules for a Safe Home Exchange contact telephone numbers Some facts about home burglary with your neighbours so that you can If burglars do not manage to get into a Keep the door to your building closed be reached in an emergency. building in the first three minutes, they during the day. Always check who usually give up. wants to enter the building before Tell elderly people in your neighbour- opening the door. hood that they can call you if unknown Only one third of attempted burglaries persons want to come into their build- are reported, but these attempts pro- Pay close attention to unknown per- ing. vide the police with helpful investiga- sons in the area around your building tive approaches, so it is important that you report any attempts! and approach them if necessary. Notify the police if anything suspicious happens. Never try to apprehend bur- It is rarely the case that occupants are Always turn the key twice in your glars! at home when burglaries are commit- door’s lock and do not just close it. ted. Do not allow unknown persons into Never hide your keys outside your your home. home. Most burglars gain entry into buildings round the back of the ground floor! Close your windows and balcony The vast majority of burglaries are doors, even if you are only out for a committed with windows and doors short time. If you notice anything suspicious, noti- being pried open. -

NACHRICHTEN AUS DER PFALZ September 2019
NACHRICHTEN AUS DER PFALZ September 2019 „Der Mond ist aufgegangen - zeitlose Faszination Himmelskörper“ Von jeher strebte der Mensch danach, die ihn umgebende Welt zu verstehen und so auch das Weltall zu ergründen und die Zusammenhänge des Kosmos zu erforschen. Wie das ungebrochene Interesse am Weltraum in wissenschaftlicher wie auch kulturhistorischer Hinsicht unseren Alltag beeinflusst, darüber spricht Landessprecherin Marlene Siegel in der Feierstunde im GDA-Wohnstift Neustadt am Sonntag, 01. September 2019, 10.00 Uhr. Interessierte Gäste sind herzlich willkommen. Ludwigshafen spielt Die Ludwigshafener Innenstadt verwandelt sich beim Kinderfest "Ludwigshafen spielt" all- jährlich in den größten Spielplatz der Metropolregion Rhein-Neckar. In der Fußgängerzone Bismarckstraße laden zahlreiche Mitmachstände zum Spielen und Experimentieren ein. Die Freireligiöse Jugend ist am Stand des Stadtjugendring am Samstag, 14. September 2019, 11.00-16.00 Uhr vertreten. Humanistisch-ethischer Stammtisch „Grenzenlose Gewalt?“ Die Fälle von spontan ausrastenden Menschen, deren Gewaltbereitschaft sogar die Tötung des Opfers mit einschließt, sind unfassbar und schrecklich. Wie können und wie wollen wir als Gesellschaft reagieren? Ratlosigkeit und „weiter so“ sind keine Lösung. Diskutieren sie mit. Der Stammtisch trifft sich am Donnerstag, 19. September 2019, 18.00 Uhr im Restaurant „Zur neuen Pfalz“, Hohenzollernstr. 104, 67063 Ludwigshafen. Es hilft uns auch, wenn Sie sich kurzfristig anmelden unter 0621 512582 / [email protected] Preisverleihung