Non-Interventional Study Protocol NVA237A2401T
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Isopropamide Iodide
www.chemicalland21.com ISOPROPAMIDE IODIDE SYNONYMS (3-Carbamoyl-3,3-diphenylpropyl)diisopropylmethylammonium iodide; 2,2-Diphenyl-4- diisopropylaminobutyramide methiodide; 4-(Diisopropylamino)-2,2-diphenylbutyramide methiodide; gamma-(Aminocarbonyl)-N-methyl-N,N-bis(1-methylethyl)-gamma-phenylbenzenepropanaminium iodide; Iodure d'isopropamide; Ioduro de isopropamida; Isopropamide ioduro; Isopropamidi iodidum; Isoproponum iodide; PRODUCT IDENTIFICATION CAS RN 71-81-8 EINECS RN 200-766-8 FORMULA C23H33IN2O MOL WEIGHT 480.43 PHYSICAL AND CHEMICAL PROPERTIES PHYSICAL STATE white to off-white powder MELTING POINT 199 C BOILING POINT DENSITY SOLUBILITY IN WATER pH VAPOR DENSITY REFRACTIVE INDEX FLASH POINT GENERAL DESCRIPTION Isopropamide is a long-acting anticholinergic and antimuscarinic drug of quaternary ammonium structure. It is used in the form of the iodide, (also bromide or chloride) to treat peptic ulcer and to suppress gastric secretion other gastrointestinal disorders. Brands of Isopropamide drugs: Darbid Dipramide Isamide Marygin-M Piaccamide Priamide Priazimide Sanulcin Tyrimide Quaternary ammonium anticholinergics (Synthetic) ATC Code Product CAS RN. A03AB01 Benzilonium bromide 1050-48-2 A03AB02 Glycopyrrolate 596-51-0 A03AB03 Oxyphenonium 14214-84-7 A03AB04 Penthienate 22064-27-3 A03AB05 Propantheline 50-34-0 A03AB06 Otilonium bromide 26095-59-0 A03AB07 Methantheline 5818-17-7 Please mail us if you want to sell your product or need to buy some products) www.chemicalland21.com ISOPROPAMIDE IODIDE A03AB08 Tridihexethyl 60-49-1 A03AB09 Isopropamide 7492-32-2 A03AB10 Hexocyclium 6004-98-4 A03AB11 Poldine 596-50-9 A03AB12 Mepenzolic acid 25990-43-6 A03AB13 Bevonium 33371-53-8 A03AB14 Pipenzolate 13473-38-6 A03AB15 Diphemanil methylsulfate 62-97-5 A03AB16 (2-Benzhydryloxyethyl)diethyl-methylammonium iodide A03AB17 Tiemonium iodide 144-12-7 A03AB18 Prifinium bromide 4630-95-9 A03AB19 Timepidium bromide 35035-05-3 A03AB21 Fenpiverinium bromide 125-60-0 03AB53 Oxyphenonium, combinations STABILITY AND REACTIVITY STABILITY Stable under normal conditions. -

(12) Patent Application Publication (10) Pub. No.: US 2006/0110428A1 De Juan Et Al
US 200601 10428A1 (19) United States (12) Patent Application Publication (10) Pub. No.: US 2006/0110428A1 de Juan et al. (43) Pub. Date: May 25, 2006 (54) METHODS AND DEVICES FOR THE Publication Classification TREATMENT OF OCULAR CONDITIONS (51) Int. Cl. (76) Inventors: Eugene de Juan, LaCanada, CA (US); A6F 2/00 (2006.01) Signe E. Varner, Los Angeles, CA (52) U.S. Cl. .............................................................. 424/427 (US); Laurie R. Lawin, New Brighton, MN (US) (57) ABSTRACT Correspondence Address: Featured is a method for instilling one or more bioactive SCOTT PRIBNOW agents into ocular tissue within an eye of a patient for the Kagan Binder, PLLC treatment of an ocular condition, the method comprising Suite 200 concurrently using at least two of the following bioactive 221 Main Street North agent delivery methods (A)-(C): Stillwater, MN 55082 (US) (A) implanting a Sustained release delivery device com (21) Appl. No.: 11/175,850 prising one or more bioactive agents in a posterior region of the eye so that it delivers the one or more (22) Filed: Jul. 5, 2005 bioactive agents into the vitreous humor of the eye; (B) instilling (e.g., injecting or implanting) one or more Related U.S. Application Data bioactive agents Subretinally; and (60) Provisional application No. 60/585,236, filed on Jul. (C) instilling (e.g., injecting or delivering by ocular ion 2, 2004. Provisional application No. 60/669,701, filed tophoresis) one or more bioactive agents into the Vit on Apr. 8, 2005. reous humor of the eye. Patent Application Publication May 25, 2006 Sheet 1 of 22 US 2006/0110428A1 R 2 2 C.6 Fig. -

The In¯Uence of Medication on Erectile Function
International Journal of Impotence Research (1997) 9, 17±26 ß 1997 Stockton Press All rights reserved 0955-9930/97 $12.00 The in¯uence of medication on erectile function W Meinhardt1, RF Kropman2, P Vermeij3, AAB Lycklama aÁ Nijeholt4 and J Zwartendijk4 1Department of Urology, Netherlands Cancer Institute/Antoni van Leeuwenhoek Hospital, Plesmanlaan 121, 1066 CX Amsterdam, The Netherlands; 2Department of Urology, Leyenburg Hospital, Leyweg 275, 2545 CH The Hague, The Netherlands; 3Pharmacy; and 4Department of Urology, Leiden University Hospital, P.O. Box 9600, 2300 RC Leiden, The Netherlands Keywords: impotence; side-effect; antipsychotic; antihypertensive; physiology; erectile function Introduction stopped their antihypertensive treatment over a ®ve year period, because of side-effects on sexual function.5 In the drug registration procedures sexual Several physiological mechanisms are involved in function is not a major issue. This means that erectile function. A negative in¯uence of prescrip- knowledge of the problem is mainly dependent on tion-drugs on these mechanisms will not always case reports and the lists from side effect registries.6±8 come to the attention of the clinician, whereas a Another way of looking at the problem is drug causing priapism will rarely escape the atten- combining available data on mechanisms of action tion. of drugs with the knowledge of the physiological When erectile function is in¯uenced in a negative mechanisms involved in erectile function. The way compensation may occur. For example, age- advantage of this approach is that remedies may related penile sensory disorders may be compen- evolve from it. sated for by extra stimulation.1 Diminished in¯ux of In this paper we will discuss the subject in the blood will lead to a slower onset of the erection, but following order: may be accepted. -

Classification of Medicinal Drugs and Driving: Co-Ordination and Synthesis Report
Project No. TREN-05-FP6TR-S07.61320-518404-DRUID DRUID Driving under the Influence of Drugs, Alcohol and Medicines Integrated Project 1.6. Sustainable Development, Global Change and Ecosystem 1.6.2: Sustainable Surface Transport 6th Framework Programme Deliverable 4.4.1 Classification of medicinal drugs and driving: Co-ordination and synthesis report. Due date of deliverable: 21.07.2011 Actual submission date: 21.07.2011 Revision date: 21.07.2011 Start date of project: 15.10.2006 Duration: 48 months Organisation name of lead contractor for this deliverable: UVA Revision 0.0 Project co-funded by the European Commission within the Sixth Framework Programme (2002-2006) Dissemination Level PU Public PP Restricted to other programme participants (including the Commission x Services) RE Restricted to a group specified by the consortium (including the Commission Services) CO Confidential, only for members of the consortium (including the Commission Services) DRUID 6th Framework Programme Deliverable D.4.4.1 Classification of medicinal drugs and driving: Co-ordination and synthesis report. Page 1 of 243 Classification of medicinal drugs and driving: Co-ordination and synthesis report. Authors Trinidad Gómez-Talegón, Inmaculada Fierro, M. Carmen Del Río, F. Javier Álvarez (UVa, University of Valladolid, Spain) Partners - Silvia Ravera, Susana Monteiro, Han de Gier (RUGPha, University of Groningen, the Netherlands) - Gertrude Van der Linden, Sara-Ann Legrand, Kristof Pil, Alain Verstraete (UGent, Ghent University, Belgium) - Michel Mallaret, Charles Mercier-Guyon, Isabelle Mercier-Guyon (UGren, University of Grenoble, Centre Regional de Pharmacovigilance, France) - Katerina Touliou (CERT-HIT, Centre for Research and Technology Hellas, Greece) - Michael Hei βing (BASt, Bundesanstalt für Straßenwesen, Germany). -

Health Reports for Mutual Recognition of Medical Prescriptions: State of Play
The information and views set out in this report are those of the author(s) and do not necessarily reflect the official opinion of the European Union. Neither the European Union institutions and bodies nor any person acting on their behalf may be held responsible for the use which may be made of the information contained therein. Executive Agency for Health and Consumers Health Reports for Mutual Recognition of Medical Prescriptions: State of Play 24 January 2012 Final Report Health Reports for Mutual Recognition of Medical Prescriptions: State of Play Acknowledgements Matrix Insight Ltd would like to thank everyone who has contributed to this research. We are especially grateful to the following institutions for their support throughout the study: the Pharmaceutical Group of the European Union (PGEU) including their national member associations in Denmark, France, Germany, Greece, the Netherlands, Poland and the United Kingdom; the European Medical Association (EMANET); the Observatoire Social Européen (OSE); and The Netherlands Institute for Health Service Research (NIVEL). For questions about the report, please contact Dr Gabriele Birnberg ([email protected] ). Matrix Insight | 24 January 2012 2 Health Reports for Mutual Recognition of Medical Prescriptions: State of Play Executive Summary This study has been carried out in the context of Directive 2011/24/EU of the European Parliament and of the Council of 9 March 2011 on the application of patients’ rights in cross- border healthcare (CBHC). The CBHC Directive stipulates that the European Commission shall adopt measures to facilitate the recognition of prescriptions issued in another Member State (Article 11). At the time of submission of this report, the European Commission was preparing an impact assessment with regards to these measures, designed to help implement Article 11. -

Deficits in Cholinergic Neurotransmission and Their Clinical
www.nature.com/npjparkd All rights reserved 2373-8057/16 REVIEW ARTICLE OPEN Deficits in cholinergic neurotransmission and their clinical correlates in Parkinson’s disease Santiago Perez-Lloret1 and Francisco J Barrantes2 In view of its ability to explain the most frequent motor symptoms of Parkinson’s Disease (PD), degeneration of dopaminergic neurons has been considered one of the disease’s main pathophysiological features. Several studies have shown that neurodegeneration also affects noradrenergic, serotoninergic, cholinergic and other monoaminergic neuronal populations. In this work, the characteristics of cholinergic deficits in PD and their clinical correlates are reviewed. Important neurophysiological processes at the root of several motor and cognitive functions remit to cholinergic neurotransmission at the synaptic, pathway, and circuital levels. The bulk of evidence highlights the link between cholinergic alterations and PD motor symptoms, gait dysfunction, levodopa-induced dyskinesias, cognitive deterioration, psychosis, sleep abnormalities, autonomic dysfunction, and altered olfactory function. The pathophysiology of these symptoms is related to alteration of the cholinergic tone in the striatum and/or to degeneration of cholinergic nuclei, most importantly the nucleus basalis magnocellularis and the pedunculopontine nucleus. Several results suggest the clinical usefulness of antimuscarinic drugs for treating PD motor symptoms and of inhibitors of the enzyme acetylcholinesterase for the treatment of dementia. Data also suggest that these inhibitors and pedunculopontine nucleus deep-brain stimulation might also be effective in preventing falls. Finally, several drugs acting on nicotinic receptors have proved efficacious for treating levodopa-induced dyskinesias and cognitive impairment and as neuroprotective agents in PD animal models. Results in human patients are still lacking. -

)&F1y3x PHARMACEUTICAL APPENDIX to THE
)&f1y3X PHARMACEUTICAL APPENDIX TO THE HARMONIZED TARIFF SCHEDULE )&f1y3X PHARMACEUTICAL APPENDIX TO THE TARIFF SCHEDULE 3 Table 1. This table enumerates products described by International Non-proprietary Names (INN) which shall be entered free of duty under general note 13 to the tariff schedule. The Chemical Abstracts Service (CAS) registry numbers also set forth in this table are included to assist in the identification of the products concerned. For purposes of the tariff schedule, any references to a product enumerated in this table includes such product by whatever name known. Product CAS No. Product CAS No. ABAMECTIN 65195-55-3 ACTODIGIN 36983-69-4 ABANOQUIL 90402-40-7 ADAFENOXATE 82168-26-1 ABCIXIMAB 143653-53-6 ADAMEXINE 54785-02-3 ABECARNIL 111841-85-1 ADAPALENE 106685-40-9 ABITESARTAN 137882-98-5 ADAPROLOL 101479-70-3 ABLUKAST 96566-25-5 ADATANSERIN 127266-56-2 ABUNIDAZOLE 91017-58-2 ADEFOVIR 106941-25-7 ACADESINE 2627-69-2 ADELMIDROL 1675-66-7 ACAMPROSATE 77337-76-9 ADEMETIONINE 17176-17-9 ACAPRAZINE 55485-20-6 ADENOSINE PHOSPHATE 61-19-8 ACARBOSE 56180-94-0 ADIBENDAN 100510-33-6 ACEBROCHOL 514-50-1 ADICILLIN 525-94-0 ACEBURIC ACID 26976-72-7 ADIMOLOL 78459-19-5 ACEBUTOLOL 37517-30-9 ADINAZOLAM 37115-32-5 ACECAINIDE 32795-44-1 ADIPHENINE 64-95-9 ACECARBROMAL 77-66-7 ADIPIODONE 606-17-7 ACECLIDINE 827-61-2 ADITEREN 56066-19-4 ACECLOFENAC 89796-99-6 ADITOPRIM 56066-63-8 ACEDAPSONE 77-46-3 ADOSOPINE 88124-26-9 ACEDIASULFONE SODIUM 127-60-6 ADOZELESIN 110314-48-2 ACEDOBEN 556-08-1 ADRAFINIL 63547-13-7 ACEFLURANOL 80595-73-9 ADRENALONE -

Wo 2010/075090 A2
(12) INTERNATIONAL APPLICATION PUBLISHED UNDER THE PATENT COOPERATION TREATY (PCT) (19) World Intellectual Property Organization International Bureau (10) International Publication Number (43) International Publication Date 1 July 2010 (01.07.2010) WO 2010/075090 A2 (51) International Patent Classification: (81) Designated States (unless otherwise indicated, for every C07D 409/14 (2006.01) A61K 31/7028 (2006.01) kind of national protection available): AE, AG, AL, AM, C07D 409/12 (2006.01) A61P 11/06 (2006.01) AO, AT, AU, AZ, BA, BB, BG, BH, BR, BW, BY, BZ, CA, CH, CL, CN, CO, CR, CU, CZ, DE, DK, DM, DO, (21) International Application Number: DZ, EC, EE, EG, ES, FI, GB, GD, GE, GH, GM, GT, PCT/US2009/068073 HN, HR, HU, ID, IL, IN, IS, JP, KE, KG, KM, KN, KP, (22) International Filing Date: KR, KZ, LA, LC, LK, LR, LS, LT, LU, LY, MA, MD, 15 December 2009 (15.12.2009) ME, MG, MK, MN, MW, MX, MY, MZ, NA, NG, NI, NO, NZ, OM, PE, PG, PH, PL, PT, RO, RS, RU, SC, SD, (25) Filing Language: English SE, SG, SK, SL, SM, ST, SV, SY, TJ, TM, TN, TR, TT, (26) Publication Language: English TZ, UA, UG, US, UZ, VC, VN, ZA, ZM, ZW. (30) Priority Data: (84) Designated States (unless otherwise indicated, for every 61/122,478 15 December 2008 (15.12.2008) US kind of regional protection available): ARIPO (BW, GH, GM, KE, LS, MW, MZ, NA, SD, SL, SZ, TZ, UG, ZM, (71) Applicant (for all designated States except US): AUS- ZW), Eurasian (AM, AZ, BY, KG, KZ, MD, RU, TJ, PEX PHARMACEUTICALS, INC. -
A Systematic Review of Combination and High-Dose Atypical
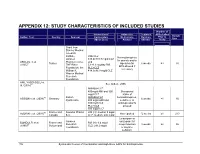
APPENDIX 12: STUDY CHARACTERISTICS OF INCLUDED STUDIES Number of Interventions/ Adjunctive Treatment APDs Failed Sample Author, Year Country Sponsor Comparators Medications Duration Prior to Size (Mean Dose) Allowed (Weeks) Study Grant from Stanley Medical research Institute, RIS+CLZ Benzodiazepines Janssen 515.6±138.7 mg/d CLZ for anxiety and/or AKDEDE et al. Pharmaceutica, and 42 Turkey biperiden for 6 weeks ≥3 30 (2005) THE Ritter 5.1±1.3 mg/day RIS EPS allowed if Foundation, the PLC+CLZ necessary William K. 414.3±96.9 mg/d CLZ Warren Medical Research Foundation ANIL YAGCIOGLU et 45 See Akdede 2006 al. (2005) AMI400+CLZ 400mg/d AMI and 300 Occasional mg/d CLZ intake of 49 Sanofi- AMI600+CLZ benzodiazepines, ASSION et al. (2008) Germany 6 weeks ≥1 16 Synthelabo 600 mg/d AMI and sedatives, or 300mg/d CLZ antidepressants PLC+CLZ allowed 300 mg/d CLZ 60 France and Novartis Phama RIS (H): median 9 mg/d AZORIN et al. (2001) Not reported 12 weeks ≥1 273 Canada S.A. CLZ: median: 600 mg/d Lorazepam or Janssen oxazepam for BONDOLFI et al. France and RIS (H): 6.4 mg/d 66 Research sleep induction 8 weeks ≥2 86 (1998) Switzerland CLZ: 291.2 mg/d Foundation or daytime sedation; 156 Systematic Review of Combination and High-Dose AAPs for Schizophrenia Number of Interventions/ Adjunctive Treatment APDs Failed Sample Author, Year Country Sponsor Comparators Medications Duration Prior to Size (Mean Dose) Allowed (Weeks) Study biperiden and procyclidine for EPS Supported by grants from Brain Research center, funded by the ARI+CLZ Antidepressants, Ministry of 15.5±7.1 mg/d ARI and 38 anticholinergics CHANG et al. -

Fisiopatologia Dei Tremori
FISIOPATOLOGIA DEI TREMORI Enrico Alfonsi Neurofisiopatologia IRCCS-Istituto Neurologico Nazionale «Casimiro Mondino» Pavia TREMOR A rhythmic involuntary movement of one or several regions of the body. It represents the most common neurological sign, as everyone has a ‘’physiological’’ tremor, which can only be measured with instrumental tools. 1 BACKGROUND Relation to Voluntary Movement Relation to Body Part Rest tremor Head tremor Parkinson’s disease Cerebellar disease Other parkinsonian syndromes Dystonia Tardive (drug-induced) parkinsonism Essential tremor (rarely when isolated) Vascular parkinsonism Chin tremor Hydrocephalus Parkinson’s disease Common Psychogenic (functional) tremor Hereditary geniospasm tremor Action tremor Jaw tremor disorders Postural tremor Parkinson’s disease classified Physiologic tremor and enhanced physiologic tremor Dystonia according Essential tremor Palatal tremor to two main Dystonic tremor Idiopathic (essential) criteria Parkinsonism Owing to brainstem lesions (secondary) Fragile X premutation (fragile X tremor–ataxia syndrome) Owing to degenerative disease (adult-onset Alexander’s disease) Neuropathies Arm tremor Tardive tremor Cerebellar disease Toxins (e.g., mercury) Dystonia Metabolic disorder (e.g., hyperthyroidism, hypoglycemia) Essential tremor Psychogenic (functional) tremor Parkinson’s disease Kinetic tremor Leg tremor Cerebellar disease Parkinson’s disease Holmes’ tremor Orthostatic tremor Wilson’s disease Psychogenic (functional) tremor 2 Essential tremor Features considered typical of the essential tremor syndrome Feature Description Tremor 4–12 Hz action tremor that occurs when patients voluntarily attempt • A resting tremor can appear only in advanced to maintain a steady posture stages. Other neurological signs (with the against gravity (postural tremor) or move (kinetic tremor) exception of cog-wheel phenomenon and Tremor may be suppressed by difficulties with tandem gait) are typically performing skilled manual tasks absent. -

(12) Patent Application Publication (10) Pub. No.: US 2006/0024365A1 Vaya Et Al
US 2006.0024.365A1 (19) United States (12) Patent Application Publication (10) Pub. No.: US 2006/0024365A1 Vaya et al. (43) Pub. Date: Feb. 2, 2006 (54) NOVEL DOSAGE FORM (30) Foreign Application Priority Data (76) Inventors: Navin Vaya, Gujarat (IN); Rajesh Aug. 5, 2002 (IN)................................. 699/MUM/2002 Singh Karan, Gujarat (IN); Sunil Aug. 5, 2002 (IN). ... 697/MUM/2002 Sadanand, Gujarat (IN); Vinod Kumar Jan. 22, 2003 (IN)................................... 80/MUM/2003 Gupta, Gujarat (IN) Jan. 22, 2003 (IN)................................... 82/MUM/2003 Correspondence Address: Publication Classification HEDMAN & COSTIGAN P.C. (51) Int. Cl. 1185 AVENUE OF THE AMERICAS A6IK 9/22 (2006.01) NEW YORK, NY 10036 (US) (52) U.S. Cl. .............................................................. 424/468 (22) Filed: May 19, 2005 A dosage form comprising of a high dose, high Solubility active ingredient as modified release and a low dose active ingredient as immediate release where the weight ratio of Related U.S. Application Data immediate release active ingredient and modified release active ingredient is from 1:10 to 1:15000 and the weight of (63) Continuation-in-part of application No. 10/630,446, modified release active ingredient per unit is from 500 mg to filed on Jul. 29, 2003. 1500 mg, a process for preparing the dosage form. Patent Application Publication Feb. 2, 2006 Sheet 1 of 10 US 2006/0024.365A1 FIGURE 1 FIGURE 2 FIGURE 3 Patent Application Publication Feb. 2, 2006 Sheet 2 of 10 US 2006/0024.365A1 FIGURE 4 (a) 7 FIGURE 4 (b) Patent Application Publication Feb. 2, 2006 Sheet 3 of 10 US 2006/0024.365 A1 FIGURE 5 100 ov -- 60 40 20 C 2 4. -

Partial Agreement in the Social and Public Health Field
COUNCIL OF EUROPE COMMITTEE OF MINISTERS (PARTIAL AGREEMENT IN THE SOCIAL AND PUBLIC HEALTH FIELD) RESOLUTION AP (88) 2 ON THE CLASSIFICATION OF MEDICINES WHICH ARE OBTAINABLE ONLY ON MEDICAL PRESCRIPTION (Adopted by the Committee of Ministers on 22 September 1988 at the 419th meeting of the Ministers' Deputies, and superseding Resolution AP (82) 2) AND APPENDIX I Alphabetical list of medicines adopted by the Public Health Committee (Partial Agreement) updated to 1 July 1988 APPENDIX II Pharmaco-therapeutic classification of medicines appearing in the alphabetical list in Appendix I updated to 1 July 1988 RESOLUTION AP (88) 2 ON THE CLASSIFICATION OF MEDICINES WHICH ARE OBTAINABLE ONLY ON MEDICAL PRESCRIPTION (superseding Resolution AP (82) 2) (Adopted by the Committee of Ministers on 22 September 1988 at the 419th meeting of the Ministers' Deputies) The Representatives on the Committee of Ministers of Belgium, France, the Federal Republic of Germany, Italy, Luxembourg, the Netherlands and the United Kingdom of Great Britain and Northern Ireland, these states being parties to the Partial Agreement in the social and public health field, and the Representatives of Austria, Denmark, Ireland, Spain and Switzerland, states which have participated in the public health activities carried out within the above-mentioned Partial Agreement since 1 October 1974, 2 April 1968, 23 September 1969, 21 April 1988 and 5 May 1964, respectively, Considering that the aim of the Council of Europe is to achieve greater unity between its members and that this