Plants and Parts of Plants Used in Food Supplements: an Approach to Their
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Evaluation of Antiurolithiatic Activity of Ethanolic Extract of Annona
S. Ramachandran et al. Int. Res. J. Pharm. 2014, 5 (11) INTERNATIONAL RESEARCH JOURNAL OF PHARMACY www.irjponline.com ISSN 2230 – 8407 Research Article EVALUATION OF ANTIUROLITHIATIC ACTIVITY OF ETHANOLIC EXTRACT OF ANNONA RETICULATA AGAINST ETHYLENE GLYCOL AND AMMONIUM CHLORIDE INDUCED UROLITHIASIS IN ALBINO WISTAR RATS S. Ramachandran1*, B Sandhya Rani2, Sahu Nimain Charan3, C Ramesh4 1Professor, Department of Pharmacology, GIET School of Pharmacy, Rajahmundry, Andhra Pradesh, India 2M Pharm, Department of Pharmacology, GIET School of Pharmacy, Rajahmundry, Andhra Pradesh, India 3Assistant Professor, Department of Pharmacology, GIET School of Pharmacy, Rajahmundry, Andhra Pradesh, India 4 Study director, Sicra labs, Andhra Pradesh, India *Corresponding Author Email: [email protected] Article Received on: 21/09/14 Revised on: 22/10/14 Approved for publication: 11/11/14 DOI: 10.7897/2230-8407.0511171 ABSTRACT Urinary stone disorder has afflicted humankind since antiquity and can persist, with serious medical consequences, throughout a patient’s lifetime. The common component of urinary stone is calcium oxalate (CaOx). In spite of tremendous advances in the field of medicine, there is no truly satisfactory drug for the treatment of renal calculi. In the indigenous system of medicine, the leaves of Annona reticulata (Family - Anonaceae) are reported to be useful in the treatment of urinary stones. Hence, in the present study, the Annona reticulata have been selected for their anti urolithiatic activity on experimentally induced urolithiatic rats. Keywords: Ammonium chloride, Ethylene glycol, Lithiasis, Annona reticulata. INTRODUCTION admixtures not adhering to the medicinal plant materials Traditional medicine using herbal drugs exists in every e.g. soil, stones, dust etc. -

Section 3417. Mexican Fruit Fly Interior Quarantine
Section 3417. Mexican Fruit Fly Interior Quarantine A quarantine is established against the following pest, its hosts and possible carriers: A. Pest. Mexican fruit fly (Anastrepha ludens) B. Area Under Quarantine. 1. An area shall be designed as under quarantine when survey results indicate an infestation is present, the Department has defined the infested area and the local California County Agricultural Commissioner(s) is notified and requests the quarantine area be established. The Department shall also provide electronic and/or written notification of the area designation(s) to other California County Agricultural Commissioners and other interested or affected parties and post the area description to its website at: https://www.cdfa.ca.gov/plant/mexfly/regulation.html. An interested party may also go to the above website and elect to receive automatic notifications of any changes in the regulated or quarantine areas through the list serve option. 2. If an area is not undergoing the sterile insect technique, an infestation is present when eggs, a larva, a pupa, a mated female or five or more male or unmated female Mexican fruit fly adults are detected within three miles of each other and within one life cycle. In an area undergoing sterile insect technique the criteria for an infestation are the same except a single mated female does not constitute an infestation but counts towards an adult for five or more. 3. The initial area under quarantine shall be a minimum of 4.5 mile radius surrounding the qualifying detections being used as an epicenter. Commercial host properties shall not be split by the quarantine boundary line and the boundary line shall be expanded beyond the 4.5 miles as necessary to encompass such host material in its entirety. -

Characterization of Polyphenol Oxidase and Antioxidants from Pawpaw (Asimina Tribola) Fruit
University of Kentucky UKnowledge University of Kentucky Master's Theses Graduate School 2007 CHARACTERIZATION OF POLYPHENOL OXIDASE AND ANTIOXIDANTS FROM PAWPAW (ASIMINA TRIBOLA) FRUIT Caodi Fang University of Kentucky, [email protected] Right click to open a feedback form in a new tab to let us know how this document benefits ou.y Recommended Citation Fang, Caodi, "CHARACTERIZATION OF POLYPHENOL OXIDASE AND ANTIOXIDANTS FROM PAWPAW (ASIMINA TRIBOLA) FRUIT" (2007). University of Kentucky Master's Theses. 477. https://uknowledge.uky.edu/gradschool_theses/477 This Thesis is brought to you for free and open access by the Graduate School at UKnowledge. It has been accepted for inclusion in University of Kentucky Master's Theses by an authorized administrator of UKnowledge. For more information, please contact [email protected]. ABSTRACT OF THESIS CHARACTERIZATION OF POLYPHENOL OXIDASE AND ANTIOXIDANTS FROM PAWPAW (ASIMINA TRIBOLA) FRUIT Crude polyphenol oxidase (PPO) was extracted from pawpaw (Asimina triloba) fruit. The enzyme exhibited a maximum activity at pH 6.5–7.0 and 5–20 °C, and had -1 a maximum catalysis rate (Vmax) of 0.1363 s and a reaction constant (Km) of 0.3266 M. It was almost completely inactivated when incubated at 80 °C for 10 min. Two isoforms of PPO (MW 28.2 and 38.3 kDa) were identified by Sephadex gel filtration chromatography and polyacrylamide gel electrophoresis. Both the concentration and the total activity of the two isoforms differed (P < 0.05) between seven genotypes of pawpaw tested. Thermal stability (92 °C, 1–5 min) and colorimetry (L* a* b*) analyses showed significant variations between genotypes. -

Acid-Catalysed Hydroaminations
Acid-Catalysed Hydroaminations A thesis submitted to Cardiff University by Laura Henderson MChem (Hons.) In candidature of the degree of Doctor of Philosophy School of Chemistry Cardiff University UMI Number: U557419 All rights reserved INFORMATION TO ALL USERS The quality of this reproduction is dependent upon the quality of the copy submitted. In the unlikely event that the author did not send a complete manuscript and there are missing pages, these will be noted. Also, if material had to be removed, a note will indicate the deletion. Dissertation Publishing UMI U557419 Published by ProQuest LLC 2013. Copyright in the Dissertation held by the Author. Microform Edition © ProQuest LLC. All rights reserved. This work is protected against unauthorized copying under Title 17, United States Code. ProQuest LLC 789 East Eisenhower Parkway P.O. Box 1346 Ann Arbor, Ml 48106-1346 Acknowledgments First of all I would like to thank Prof. David W. Knight, for all his support, great ideas and seemingly endless breadth of knowledge that made this project possible. Secondly, I would also like to thank Dr. Andrew C. Williams for all the support and advice he has given over the last three years. I am grateful to the many students whose have contributed towards this thesis; they were all a joy to work with. In particular, I want to thank Nena Christiansen, Jon Williams and Rhian Courtney for their work. I want to thank Dr Rob Jenkins, Robin Hicks and Dave Walker for all of their mass spec, and NMR support over the years. I also want to thank Dr John Brazier and Dr Jacky Yau for all the advice and help that they gave, and endless enthusiasm that they have shown. -

International Standard Iso 4720:2018(E)
This preview is downloaded from www.sis.se. Buy the entire standard via https://www.sis.se/std-80006399 INTERNATIONAL ISO STANDARD 4720 Fourth edition 2018-08 Essential oils — Nomenclature Huiles essentielles — Nomenclature Reference number ISO 4720:2018(E) © ISO 2018 This preview is downloaded from www.sis.se. Buy the entire standard via https://www.sis.se/std-80006399 ISO 4720:2018(E) COPYRIGHT PROTECTED DOCUMENT © ISO 2018 All rights reserved. Unless otherwise specified, or required in the context of its implementation, no part of this publication may be reproduced or utilized otherwise in any form or by any means, electronic or mechanical, including photocopying, or posting on the internet or an intranet, without prior written permission. Permission can be requested from either ISO at the address below or ISO’s member body in the country of the requester. ISO copyright office CP 401 • Ch. de Blandonnet 8 CH-1214 Vernier, Geneva Phone: +41 22 749 01 11 Fax:Website: +41 22www.iso.org 749 09 47 Email: [email protected] iiPublished in Switzerland © ISO 2018 – All rights reserved This preview is downloaded from www.sis.se. Buy the entire standard via https://www.sis.se/std-80006399 ISO 4720:2018(E) Contents Page Foreword ........................................................................................................................................................................................................................................iv Introduction ..................................................................................................................................................................................................................................v -
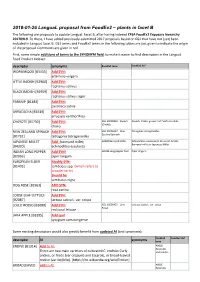
2018-01-26 Langual Proposal from Foodex2 – Plants in Facet B
2018-01-26 LanguaL proposal from FoodEx2 – plants in facet B The following are proposals to update LanguaL Facet B, after having indexed EFSA FoodEx2 Exposure hierarchy 20170919. To these, I have added previously-submitted 2017 proposals based on GS1 that have not (yet) been included in LanguaL facet B. GS1 terms and FoodEx2 terms in the following tables are just given to indicate the origin of the proposal. Comments are given in red. First, some simple additions of terms to the SYNONYM field, to make it easier to find descriptors in the LanguaL Food Product Indexer: descriptor synonyms FoodEx2 term FoodEx2 def WORMWOOD [B3433] Add SYN: artemisia vulgaris LITTLE RADISH [B2960] Add SYN: raphanus sativus BLACK RADISH [B2959] Add SYN: raphanus sativus niger PARSNIP [B1483] Add SYN: pastinaca sativa ARRACACHA [B3439] Add SYN: arracacia xanthorrhiza CHAYOTE [B1730] Add SYN: GS1 10006356 - Squash Squash, Choko, grown from Sechium edule (Choko) choko NEW ZEALAND SPINACH Add SYN: GS1 10006427 - New- Tetragonia tetragonoides Zealand Spinach [B1732] tetragonia tetragonoides JAPANESE MILLET Add : barnyard millet; A000Z Barnyard millet Echinochloa esculenta (A. Braun) H. Scholz, Barnyard millet or Japanese Millet. [B4320] echinochloa esculenta INDIAN LONG PEPPER Add SYN! A019B Long pepper fruit Piper longum [B2956] piper longum EUROPEAN ELDER Modify SYN: [B1403] sambucus spp. (which refers to broader term) Should be sambucus nigra DOG ROSE [B2961] ADD SYN: rosa canina LOOSE LEAF LETTUCE Add SYN: [B2087] lactusa sativa L. var. crispa LOLLO ROSSO [B2088] Add SYN: GS1 10006425 - Lollo Lactuca sativa L. var. crispa Rosso red coral lettuce JAVA APPLE [B3395] Add syn! syzygium samarangense Some existing descriptors would also greatly benefit from updated AI (and synonyms): FoodEx2 FoodEx2 def descriptor AI synonyms term ENDIVE [B1314] Add to AI: A00LD Escaroles There are two main varieties of cultivated C. -

Research Journal of Pharmaceutical, Biological and Chemical Sciences
ISSN: 0975-8585 Research Journal of Pharmaceutical, Biological and Chemical Sciences An Ethnobotanical Comparitive Analysis of the Pharmacological Aspects of Annona reticulata, Annona squamosa and Annona muricata, with Mathematical Modeling. Sandeep Suryan, Nagananda G.S*, Hamsapriye, Padmashree Anand, and Swetha Seshagiri. Centre for Incubation, Innovation, Research and Consultancy (CIIRC), Jyothy Institute of Technology, Tataguni, Off Kanakapura Road, Bangalore 560082, Karnataka, India. ABSTRACT Cancer is a major cause of morbidity and mortality worldwide. Since Annonacea members possess lot of medicinal properties such as cytotoxic, immune modulator, etc., they are being used as a natural remedy for a wide range of illnesses. The study accounts for the pharmacological applications of Annona reticulata, Annona squamosa, Annona muricata leaf extracts individually, and in combination. Annona squamosa extract exhibited highest antioxidant activity compared to the other two extracts which has been validated mathematically. The combination of all the three extracts has been found effective against both Bacillus cereus and Streptococci sp.. Annona squamosa significantly inhibited the growth of Staphylococcus aureus. Annona squamosa has been found to be effectual against Candida albicans, Aspergillus niger and Cryptococcus. The combination of all three samples exhibits higher apoptosis of cancer cells compared to Annona muricata extract. Keywords: Annona reticulata, Annona squamosa, Annona muricate, Ethnobotanical Comparitive. *Corresponding author January–February 2018 RJPBCS 9(1) Page No. 326 ISSN: 0975-8585 INTRODUCTION Increasing globalization and industrialization have profound impact on the life style of majority of the world population [1]. The change in the lifestyle in turn leads to the emergence of various chronic diseases which are the main threat to the population. -

Microgram Journal, Vol 3, Number 2
MICROGRAM Laboratory Operations Division Office Of Science And Drug Abuse Prevention BUREAU OF NARCOTICS & DANGEROUS DRUGS / U.S. DEPARTMENT OF JUSTICE / WASHINGTION, D.C. 20537 Vol.III, No. 2 March-April, 1970 STP (4-Methyl-2,5-dimethoxyamphetamine) hydrochloride was found coating the inside of capsules sent to BNDDfrom Germany. The capsules were clear, hard gelatin, standard shape size No. o. Average weight was 114 milligrams. Each capsule had a white crystalline coating on inner surface of capsule body. Apparently a measu~ed amount of solution had been placedin the cap·sule body, after which it was rotated to spread the solution on the inner surface. The substance contained 8. 7 milli grams STP (DOM)HCl per ca·psule. · These were the first STP capsules of this type seen by our laboratory. A few years ago, capsules were ob tained in the U.S. similarly coated with LSD. STP (Free Base) on laboratory filter paper, also from Germany, was seen for the first time in our laboratory. The STP spots, containing approxi mately 8 miliigrams STP base each, were 5/8 to 3/4 inch in diameter. The paper was 1\ inches square. Phencyclidine (Free Base) was recently analyzed on parsley leaves. Called "Angel DUst, 11 the phencyclidine on two samples of leaves was 2.6% and 3.6%. Approximately thirty pounds of 94% pure powder was also analyzed. (For identification of phencyclidine base, see Microgram, II, 1, p.3 (Jan 1969). IMITATIONSof well-known drug products are examined frequently in our Special Testing and Research Laboratory. Many of these are well made preparations and closely resemble the imitated product. -

Periodic Table of Herbs 'N Spices
Periodic Table of Herbs 'N Spices 11HH 1 H 2 HeHe Element Proton Element Symbol Number Chaste Tree Chile (Vitex agnus-castus) (Capsicum frutescens et al.) Hemptree, Agnus Cayenne pepper, Chili castus, Abraham's balm 118Uuo Red pepper 33LiLi 44 Be 5 B B 66 C 7 N 7N 88O O 99 F 1010 Ne Ne Picture Bear’s Garlic Boldo leaves Ceylon Cinnamon Oregano Lime (Allium ursinum) (Peumus boldus) (Cinnamomum zeylanicum) Nutmeg Origanum vulgare Fenugreek Lemon (Citrus aurantifolia) Ramson, Wild garlic Boldina, Baldina Sri Lanka cinnamon (Myristica fragrans) Oregan, Wild marjoram (Trigonella foenum-graecum) (Citrus limon) 11 Na Na 1212 Mg Mg 1313 Al Al 1414 Si Si 1515 P P 16 S S 1717 Cl Cl 1818 Ar Ar Common Name Scientific Name Nasturtium Alternate name(s) Allspice Sichuan Pepper et al. Grains of Paradise (Tropaeolum majus) (Pimenta dioica) (Zanthoxylum spp.) Perilla (Aframomum melegueta) Common nasturtium, Jamaica pepper, Myrtle Anise pepper, Chinese (Perilla frutescens) Guinea grains, Garden nasturtium, Mugwort pepper, Pimento, pepper, Japanese Beefsteak plant, Chinese Savory Cloves Melegueta pepper, Indian cress, Nasturtium (Artemisia vulgaris) Newspice pepper, et al. Basil, Wild sesame (Satureja hortensis) (Syzygium aromaticum) Alligator pepper 1919 K K 20 Ca Ca 2121 Sc Sc 2222 Ti Ti 23 V V 24 Cr Cr 2525 Mn Mn 2626 Fe Fe 2727 Co Co 2828 Ni Ni 29 Cu Cu 3030 Zn Zn 31 Ga Ga 3232 Ge Ge 3333As As 34 Se Se 3535 Br Br 36 Kr Kr Cassia Paprika Caraway (Cinnamomum cassia) Asafetida Coriander Nigella Cumin Gale Borage Kaffir Lime (Capsicum annuum) (Carum carvi) -

Petiole Usually Stipules at the Base
Umbelliferae P. Buwalda Groningen) Annual or perennial herbs, never woody shrubs (in Malaysia). Stems often fur- rowed and with soft pith. Leaves alternate along the stems, often also in rosettes; petiole usually with a sheath, sometimes with stipules at the base; lamina usually much divided, sometimes entire. Flowers polygamous, in simple or compound um- bels, sometimes in heads, terminal or leaf-opposed, beneath with or without in- volucres and involucels. Calyx teeth 5, often obsolete. Petals 5, alternate with the calyx teeth, equal or outer ones of the inflorescence enlarged, entire or more or less divided, often with inflexed tips, inserted below the epigynous disk. Stamens alter- nate with the petals, similarly inserted. Disk 2-lobed, free from the styles or con- fluent with their thickened base, forming a stylopodium. Ovary inferior; styles 2. Fruits with 2 one-seeded mericarps, connected by a narrow or broad junction (commissure) in fruit separating, leaving sometimes a persistent axis (carpophore) either entire or splitting into 2 halves; mericarps with 5 longitudinal ribs, 1 dorsal rib at the back of the mericarp, 2 lateral ribs at the commissure; 2 intermediate ribs between the dorsal and the lateral ones; sometimes with secondary ribs be- without fascicular often vittae in tween the primary ones, these bundles; the ridges between the ribs or under the secondary ribs, and in the commissure, seldom under the primary ribs. Numerous Distr. genera and species, all over the world. The representatives native in Malaysia belong geographically to five types. (1) Ubiquitous genera (Hydrocotyle, Centella, Oenanthe); one species, & Hydrocotyle vulgaris, shows a remarkable disjunction, occurring in Europe N. -

(+)-Catechin and Quercetin from Pawpaw Pulp A
Characterization of (+)-Catechin and Quercetin from Pawpaw Pulp A thesis presented to the faculty of the College of Health Sciences and Professions of Ohio University In partial fulfillment of the requirements for the degree Master of Science Jinsoo Ahn June 2011 © 2011 Jinsoo Ahn. All Rights Reserved. 2 This thesis titled Characterization of (+)-Catechin and Quercetin from Pawpaw Pulp by JINSOO AHN has been approved for the School of Applied Health Sciences and Wellness and the College of Health Sciences and Professions by Robert G. Brannan Assistant Professor of Applied Health Sciences and Wellness Randy Leite Interim Dean, College of Health Sciences and Professions 3 ABSTRACT AHN, JINSOO, M.S., June 2011, Human and Consumer Sciences, Food and Nutrition Characterization of (+)-Catechin and Quercetin from Pawpaw Pulp Director of Thesis: Robert G. Brannan This thesis investigates the concentration of total phenolics and total flavonoids in pulp extracts of pawpaw harvested in 2008, 2009, and 2010, and the concentration of (+)- catechin and quercetin flavonoids in 2010 pawpaw pulp extracts using high performance liquid chromatography (HPLC). Next, influence of frozen storage and air or vacuum packaging of pawpaw pulp on the concentration of (+)-catechin and quercetin flavonoids was examined. In addition, properties of pawpaw pulp such as moisture content, lipid content, percent sugar, color, and pH were measured. Total phenolics were determined using the Folin-Ciocalteu assay and reported as µmol gallic acid equivalent (GAE)/ g wet tissue. The concentration was observed in the order of 2009 sample (3.91 ± 1.61) < 2008 sample (11.19 ± 0.57) < 2010 sample (14.11 ± 1.90). -
Natives to Know: Pawpaw (Asimina Triloba) by Joyce Tuharsky The
Natives to Know: Pawpaw (Asimina triloba) By Joyce Tuharsky The Pawpaw is a small, understory tree with large, drooping leaves, rich red-purple or maroon flowers, and the largest edible fruit indigenous to the eastern United States. Seldom taller than 25 feet, Pawpaws spread locally primarily by root suckers. The dark green, deciduous leaves grow up to 12 inches long, 1-2 inches wide, and are simple, alternate and spirally arranged. These large leaves clustered at the ends of branches give the tree an interesting tropical appearance. In autumn, the leaves turn a rusty yellow. Pawpaw flowers bloom in early spring about the same time that new leaves emerge. The flowers are 1-2 inches across with six petals and three sepals and borne singly on stout, hairy stems. The flowers develop into large, yellowish brown berries, 2–6 inches long and weighing up to 18 ounces. The larger fruits are plump, soft and thin skinned, similar to mangos. Inside, there are 10 to 14 brown seeds in two rows embedded in soft, edible pulp. When mature, the large fruit will bend the weak branches down. Pawpaw fruits ripen in late August to mid-September and have long been a favorite treat, which is occasionally sold at local farmers' markets. The fruit has a fragrant aroma, custardy texture, and tastes some-what between a banana and a cantaloupe. Compared to apples or peaches, Pawpaws are higher in food energy and minerals, and have double the vitamin C. They are a good source of protein, fiber, carbohydrates, and antioxidants. Nevertheless, Pawpaws have never been cultivated on a large scale, because the fruits bruise easily and ripen to fermentation soon after picked.