Opened a Window Northwell Health Center Is a “Data- Center Operates
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Joseph Waters
Transcript of oral history interview with Joseph Waters Gladstone/ Maplewood Fire Department, 1980-2007 by Kate Cavett of HAND in HAND Productions and Bob Jensen, President, Maplewood Area Historical Society for the Maplewood Area Historical Society December 16, 2013 at HAND in HAND Productions’ office in Saint Paul, Minnesota 1 © Maplewood Area Historical Society 2014 This project has been made possible by the Arts and Cultural Heritage Fund through the vote of Minnesotans on November 4, 2008. Administered by the Minnesota Historical Society. All pictures are from the Waters family and Maplewood Area Historical Society 2 ORAL HISTORY Oral History is the spoken word in print. Oral histories are personal memories shared from the perspective of the narrator. By means of recorded interviews oral history documents collect spoken memories and personal commentaries of historical significance. These interviews are transcribed verbatim and minimally edited for accessibility. Greatest appreciation is gained when one can listen to an oral history aloud. Oral histories do not follow the standard language usage of the written word. Transcribed interviews are not edited to meet traditional writing standards; they are edited only for clarity and understanding. The hope of oral history is to capture the flavor of the narrator’s speech and convey the narrator’s feelings through the timbre and tempo of speech patterns. An oral history is more than a family tree with names of ancestors and their birth and death dates. Oral history is recorded personal memory, and that is its value. What it offers complements other forms of historical text, and does not always require historical corroboration. -
PROFILE Book 'Rank and O Host: Staughton Lynd's Nyder
page 6 ad lib thursday, September 14, 1978 Nelson, Taml Luchow and Elizabeth Taylor. A visit to Studio 54, New York's most popular disco will also be presented. (Premiere) DTDODIldlSlW CONTEMPORARY NEBRASKA ART AND ARTISTS O JOKER'S WILD 6:00 UO MONDAY NIGHT AT THE MOVIES 'Audrey Rose' Stars: concerts Marsha Mason, Anthony OPERATION Hopkins. An unsuspecting couple are suddenly confronted PETTICOAT by a man claiming that their daughter was really his daughter In her previous life. (2 hrs., IS When Lt. Cmdr. Mike Haller mins.) (Robert Hogan) needs emergency O Q MONDAY NIGHT surgery, the nurses have to play FOOTBALL Baltimore Colts vs i' "J J ' ' doctor and the lives of the Sea New England Patriots (2 hrs., 45 .. - mins.) ' Y . ' ' in Tiger's crew are also placed 0 M.A.S.H. Hawkeye un- jeopardy as command is transferred dergoes a drastic change when to Lt. Mike Bender he becomes temporary com- l!''''''"'x the bungling mander of the 4077th and learns on ABC-T- V (Randolph Mantooth) the the bureaucracy and ac- comedy series 'Operation Petticoat,' companying headaches that Col. returning Monday, Sept. 18. Potter deals with daily. (Season In the crew is Premiere) 'Operation Spleen,' THE with of (Bffi FABULOUS SIXTIES faced the problem reaching Nixon's inauguration, the Super the only one who can perform the Bowl and the Apollo moon lan- critical operation, an old Greek ding are among the subjects with a bad heart covered in 1969. (60 mins.) doctor who, -- m MOVIE (ORAMA)'Vi "Story unfortunately, lives on an island ofa Woman" 1969 Robert Stack, taken over by the Japanese Imperial Blbl Anderson. -
Presidents Notes N1EZH Barry Kennedy Presidents Monthly Message for December 2014 from Barry – N1EZH
December 2014 Volume 53 Issue 12 Presidents notes N1EZH Barry Kennedy Presidents Monthly Message for December 2014 from Barry – N1EZH: Please Note: There will NOT be a December MARA Monthly Meeting! Winter is almost upon us and judging from the weather, may be a long one this year! I was able to basically trade my Tipper Mount and masts that were for a 39’ Rohn 25G Tower that I may only put up about 29’ with a tilt over of some sort which I hope to be able to clean up, paint and put up in the Spring. With the additional Rotor and mast for the antennas will be about 36’ or so tall when I am done. This will make it a few feet higher than my old one from a couple of years ago before the storm took it down. If anyone else in our club has done a project this year, or may be planning one either during the Winter or next Spring, then please take some photos and submit them to Rick – [email protected] so he can put them in our MARA Newsletter. For those of you that are on Facebook, I began a Massasoit Amateur Radio Association Facebook Page and have posted several items of interest on there. I have been updating the page with Club Events, photos, etc.from time to time in the hope that it will become another avenue for us in which to spark interest in our club and keep members informed of what we are doing outside of our Club Meetings and in our Community. -

Oregon EMS Conference 2010
2 www.oregonemsconference.com Greetings from the Oregon EMS Conference Committee 2010 is shaping up to be quite the year for new events both locally and nationally. We’ve seen a number of high profile fire service management personnel within our state retire or change positions this year. We’ve seen Medicare (or should I say CMS) reimbursements go down and up in a few short months and we’ve seen historic disasters at home and around the Oregon EMS world. Conference 2010 And now your Oregon EMS Conference is having a number of “firsts” in Excellence in Education 2010. CONFERENCE LOCATION For the first time Salem, the State Capital, will be the host of The Oregon Salem Conference Center EMS Conference. The Salem Conference Center is shaping up to be a 200 Commercial St SE great facility to host what is the largest EMS Conference in Oregon. For that Salem, OR 97301 matter we are the only centralized EMS conference on the West Coast. www.salemconferencecenter.org Another first is our keynote speaker, Randolph Mantooth, (Johnny Gage The Grand Hotel (attached to the from the show Emergency), who will be making his debut for the first time. Salem Conference Center) Randolph’s character Johnny Gage and his partner Roy DeSoto (played www.phoenixgrandhotel.com by Kevin Tighe) were the motivation for thousands of folks to become 877-540-7800 (Say you are with paramedics and enter the world of EMS. While these actors played the role, the Oregon EMS Conference) it was really Jame’s Page the Grandfather of EMS that was the nuclei for the movement of pre-hospital care as we know it today. -

Changes at Honeycreek Will Impact Lowell's Chapter 1 Program by Thad Kraus Lowell Ledger Editor "We Depend a Lot on Fi- Nity
250 Volume 17, Issue 33 Wednesday, June 30,1993 Changes at Honeycreek will impact Lowell's Chapter 1 program By Thad Kraus Lowell Ledger Editor "We depend a lot on fi- nity. "Cift income permits us doing our job; two, Kent Critters says a decision on said. nancial gifts from the to continue to operate," he County Community of Men- what option to use will be A decision to relocate the Exploding needs and community to operate our S9 said. tal Health is doing its job; and made by the end of the sum- students to Pine Rest is not a shrinking resources have million budget," Critter says. Wedgwood provides ser- three, kids and adolescents can mer. reflection on Lowell Schools, united Wedgwood Christian "We can provide services for vices for 200 West Michigan better be served in homes If students are removed the executive director said. Youth and Family Services these children at about 25 kidson any given day. Critters closer to their communities," from the Honeycreek cam- "Just the opposite, Lowell and Honeycreek Christian percent of the cost to put them is proud to point out that there Critter explained. pus, the facility would then Schools have been outstand- in a state or psychiatric hos- are no children or adolescents The two facilities working be open to and for church Homes in order to provide Honeycreek, cont'd., p^. 8 better stewardship of funds. pital." from Kent County in a state as one allows them to operate operations and possibly hous- While it is not yet official, Critter said Wedgwood hospital. -
Mcswain-Dart-Article.Pdf
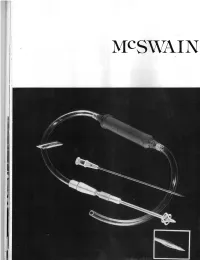
'T1 DART The McSwain Dart is a twelve cm. The pre-hospital care of tension latest model has a highly machine( long, 16 french, polyvinyl catheter over a pneumothorax has been clouded in catheter over metal stilet which can b( sharp metal stilet. It is intended to pro- controversy. This controversy has easily inserted. Additionally, a radio vide a rapid method of treating tension centered on whether or not tension paque stripe will soon be added to th( pneumothorax in either the pre or in- pneumothorax should be treated in the catheter to facilitate x-ray evaluation o hospital setting. This uniquely designed field, and if so, using what! Some of this the catheter and location. Lastly, one o catheter provides a device that can be hesitancy seems to stem from a lack of a the dart's greatest advantages is that i rapidly inserted; then flanged open to se- simple, safe, reliable, and effective de- provides not only a temporary, but ir cure in place. After removal of the vice for use by appropriately trained many cases, a definitive means o introducing stilet, a one way Heimlich paramedics. The McSwain Dart seems treating a tension or simple pneumo. valve completes the system. to fill that void. Experience by one pre- thorax. Thus while the decision to treat oi The McSwain Dart represents the first hospital care system (Bellingham, not to treat, pre-hospital, must be left ur device solely designed for treating Washington) is over eighteen field inser- to each system, that decision may hav( simple and tension pneumothorax. -
A Letter from the Publisher
Vol. 2, Issue 44 June 3, 2015 A Letter from the Publisher Shekóli. With the United States Congress in the control tween the two men and the high regard Nixon had for of the Republican Party, the close of the last term of argu- Newman—whom he felt would have been a more-famous ably the best president for Indian country ever nearly at football coach had he not been discriminated against for hand, and the 2016 elections looming on the horizon, it being Indian. The combination of personal affinity, in- is worth taking time to explore a notable moment in his- tellectual knowledge and a nose for sensible policy con- tory. In this week’s issue, ICTMN columnist and UCLA tributed in making Nixon the standard by which all U.S. Professor Duane Champagne writes about the politician presidents are judged when it comes to Indian affairs. who changed U.S. policy towards Native nations for the better: GOP President Richard M. Nixon. “Nixon’s pol- It is worth remembering that for Native nations, there icy change toward tribal self-determination was a land- are beneficial policies on both sides of the political aisle. mark initiative in Indian policy,” writes Champagne, “and Hallmark Republican policies—less governmental in- has characterized federal policy ever since.” terference and bureaucracy, more control at the local level—can be leveraged for the greater good of the U.S. In the recent book The Last Great Battle of the Indian and for Indians. As election season approaches, political Wars, author and ICTMN contributor Mark Trahant re- campaigns that seek Native support will be wise to craft counts how Forest Gerrard, the Blackfeet advisor to Sena- effective policies and messages that have worked in the tor Henry “Scoop” Jackson, crafted the policy presented past and will work again. -

Newsletter 19/07 DIGITAL EDITION Nr
ISSN 1610-2606 ISSN 1610-2606 newsletter 19/07 DIGITAL EDITION Nr. 216 - Oktober 2007 Michael J. Fox Christopher Lloyd LASER HOTLINE - Inh. Dipl.-Ing. (FH) Wolfram Hannemann, MBKS - Talstr. 3 - 70825 K o r n t a l Fon: 0711-832188 - Fax: 0711-8380518 - E-Mail: [email protected] - Web: www.laserhotline.de Newsletter 19/07 (Nr. 216) Oktober 2007 Neuankündigungen DVD BRD (Regionalcode 2) Audiokommentar, Featurettes, Trailer Zeichentrick/Fantasy 2001-2004 Ltbx 16x9 Animation DD 5.1 (D) DTS (D) DD 5.1 (Jap) 360min. AL!VE (Red Planet) 02.11.2007 79,90 EUR BestellNr.: 20023907 Avatar - Der Herr der Elemente, Buch 1: Wasser, Volume 3 Little Bee Movie - Ein Topf Honig- Avatar: The Last Airbender kompott Dir. Giancarlo Volpe, Dave Filoni, Lauren Little Bee Movie MacMullen, Anthony Lioi Kinderfilm/Zeichentrick 55min. Abenteuer/Zeichentrick 2005 FF DD 5.1 WVG Medien (Mondo Entertainment) (D) DD 5.1 (E) DD 5.1 (F) DD 2.0 (Holl) 07.12.2007 96min. 13,90 EUR BestellNr.: 20023985 Paramount 08.11.2007 13,90 EUR BestellNr.: 20023940 The Little Cars, Vol. 1-3 (3 DVDs) The Little Cars Basilisk, Vol. 07 - Chronik der Kinderfilm/Zeichentrick 130min. Koga-Ninja 79,90 EUR BestellNr.: 20024012 WVG Medien (Mondo Entertainment) Basilisk: Kôga Ninpô Chô 07.12.2007 Zeichentrick 2005 Ltbx 16x9 DD 5.1 (D) Happy Tree Friends - Die kom- 25,90 EUR BestellNr.: 20023986 DTS (D) DD 2.0 (Jap) 90min. plette erste Staffel (4 DVDs) AL!VE (OVA Films) 16.11.2007 Happy Tree Friends Magister Negi Magi Neo Box Vol. -

Volunteers Battle Multiple Fires in Week
Volume XXII No. 32 Hometown Newspaper for Glen Cove, Sea Cliff, Glen Head, Glenwood, Locust Valley and Brookville Week of 4/11/13 75C Volunteers Battle Multiple Fires In Week by Kevin C. Horton The Glen Cove Fire Department, aided by neighboring departments and Glen Cove EMS had a very active week battling large fires, burning cars, and building fires. On Saturday March 30 at 1:45am the Glen Cove Volunteers were alerted to a “signal 8,” an unknown type of fire at Ellwood Street and Valentine Street. Ac- cording to second assistant Chief Philip Grella Jr, Tom Kenary, Glen Cove Fire Dispatcher #4 received multiple calls for a big fire on Valentine Street so he upgraded the alarm to a General Alarm, “Possible house fire,” at 26 Coles Street. Firefighter and next door neighbor Robert “Rabbit” Budzenski saw that the rear of the next door neighbor’s house was on fire and two occupants were on the porch roof. He asked if anyone else was in the house and they stated no. Budzenski then got a ladder from his garage as 3rd assistant Chief Robert Marino arrived a the scene and declared the fire a “Signal 10,” a working house fire. Firefighter Budzenski put his ladder up and escorted the homeowners down unhurt and safe. Chief Joseph Solomito arrived right behind Chief Marino and set up com- continued on page 2 Firefighters battle the blaze on Coles Street (photos by Michael Marino) For the safety North Shore Relay for Life sets 2013 Fundraising Goal at $200,000! Please join us at April Team Meeting of the public- Wednesday, April 17th 2013 North Shore High School, Glen Head at 7:00 PM Please be advised that Sea June 1st-2nd, 2013 marks the 7th an- Cliff Avenue will be closed nual Relay for Life event at North Shore on April 17, 2013 High School. -
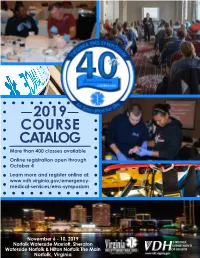
Catalog Course 2019
2019 COURSE CATALOG More than 400 classes available Online registration open through October 4 Learn more and register online at: www.vdh.virginia.gov/emergency- medical-services/ems-symposium November 6 - 10, 2019 Norfolk Waterside Marriott, Sheraton Waterside Norfolk & Hilton Norfolk The Main Norfolk, Virginia Index Registration Information 1 Wednesday Courses 9-15 On-site Check-in 2 Thursday Courses 15-22 Lodging 2 Class Worksheets Insert Parking 2 Friday Courses 23-36 Governor’s EMS Awards Reception 2 Saturday Courses 36-47 Symposium Policies 2 Sunday Courses 47 - 48 Youth and Teen Camps 2 Faculty 49-53 Continuing Education Information 3 Seminars & Meetings 54 Registration Form 4-7 Program Committee 54 Three-Day Courses 8 Steering Committee 54 Two-Day Courses 8 Exhibit Hall Vendors 55 *Note - Classes are arranged by day, time and track for ease of use when planning your schedule. Please be sure to plan for enough time to get to your classes when choosing your schedule. Cover Photo Credit: Waterside at night photo by Wayne Berry Thank You Sponsors! • Navy Region Mid-Atlantic • Virginia Department of • Virginia EMS for Children Fire & Emergency Services Fire Programs • Western Virginia EMS • Norfolk Fire/Rescue • Virginia Department of Council, Inc. Health • Regional EMS Councils Executive Directors Group • Virginia Emergency Nurses Association • State EMS Advisory Board Registration Information Registration Deadline - istrations and payment to the address in with the payment. Once the payment is October 4, 2019 the first column. You will receive a regis- processed, each registrant will receive an tration confirmation, which will include email that includes confirmation of their The Virginia EMS Symposium registration your registration information and course itinerary. -

Read the 2015-2016 Issue
THE AMERICAN PAPERS 2015-2016 The American Papers Volume 34 | 2015-2016 Faculty Advisor Dustin Abnet Co Editors-in-Chief Andrew Bahna | Kacie Hoppe Managing Editors Judson Barber | Darcy Mahoney | Liz Plett | Amanda Ritter Editorial Board Darcy Anderson | Paula Beckman | Jena Delgato-Sette Lisa Eisleben | Patricia M. Gomez | Aaron Mezzano Ashely Ongalibang | Bahar Tahamtani Layout and Design Nereida Moreno Copyright © 2016 The American Studies Student Association California State University, Fullerton. All rights reserved. All works published in The American Papers represent the views and work of individual authors. The American Papers, its Editorial Board, and publishers disclaim responsibility and liability for statements, either of fact or opinion, made by its contributors. The American Papers (ISSN 10598464) is published once yearly by the American Studies Student Association, California State University, Fullerton, P.O. Box 34080, Fullerton, California, 92634-9480. Professor Abnet would like to thank the editors for their hard work, camaraderie, and professionalism while preparing this edition of The American Papers. Their willingness to give freely of their time—even over summer break—to add to this institution is very much appreciated. He also would like to commend the authors for their exceptional papers and good-natured responses to the editorial process. Drew Bahna and Kacie Hoppe deserve special recognition for serving as this volume’s co-Editors in Chief as do Judson Barber, Darcy Mahoney, Elizabeth Plett, and Amanda Ritter for serving as the Managing Editors. Outside of the editorial board, American Studies Student Association member Jonathan Schreiber deserves thanks for his assistance in securing funding for this edition. -

Enovation Budget Swells 10 Percent Higher Than Projected Christmas
25C The Lowell Volume 15, Issue 8 Serving Lowell Area Readers Since 1893 Tuesday, December 31,1991 enovation budget swells 10 percent higher than projected Members of Lowell budgeted to make the neces- Esch said he believed one ries at a special meeting on creates logistical problems for should not precluded from pro- choofs Building and Site sary changes. of the main reasons for the Wednesday Jan. 8. the school. "We'll probably viding Lowell Schools with Committee will have more to Thoughts as to how the high bids were because reno- Of the bond issue money, have to use semi truck trailers water. "Lowell Township has weigh than just the size of school will deal with the prob- vation work would be spread S26 million is devoted to the for storage," Esch said. continued to work on a water theirholidayhillsas 1992 rolls lem include, using energy and over three summers when chil- new high school. Esch says the Balancing the disappoint- agreement with the City in. maintenance funds, but that dren are out of school. "Ide- actual transaction of the Prop- ing over-budget news was a throughout all of this," Esch Lowell Superintendentand would push back projects al- ally, we would like to be able erty Deed is expected to take letter from the City, which said. the Lowell Board, of Educa- ready planned (e.g. finishing to vacate an elementary school place in mid January. The bids stated its commitment to sup- Lowell Township has been tion learned that the budget the high school roof); re-bid- building and have the renova- for the new high school will be plying water and sewer to the asked to give a commitment for the renovation work at ding some of the work was tion work completed in nine put out in early April.