Antioxidative Effect of Far-Infrared Radiation in Human
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Computer Science & Information Technology (CS &
Computer Science & Information Technology 143 David C. Wyld, Dhinaharan Nagamalai (Eds) Computer Science & Information Technology 11th International Conference on Computer Science and Information Technology (CCSIT 2021), May 29~30, 2021, Vancouver, Canada. AIRCC Publishing Corporation Volume Editors David C. Wyld, Southeastern Louisiana University, USA E-mail: [email protected] Dhinaharan Nagamalai (Eds), Wireilla Net Solutions, Australia E-mail: [email protected] ISSN: 2231 - 5403 ISBN: 978-1-925953-41-1 DOI: 10.5121/csit.2021.110701 - 10.5121/csit.2021.110718 This work is subject to copyright. All rights are reserved, whether whole or part of the material is concerned, specifically the rights of translation, reprinting, re-use of illustrations, recitation, broadcasting, reproduction on microfilms or in any other way, and storage in data banks. Duplication of this publication or parts thereof is permitted only under the provisions of the International Copyright Law and permission for use must always be obtained from Academy & Industry Research Collaboration Center. Violations are liable to prosecution under the International Copyright Law. Typesetting: Camera-ready by author, data conversion by NnN Net Solutions Private Ltd., Chennai, India Preface The 11th International Conference on Computer Science and Information Technology (CCSIT 2021), May 29~30, 2021, Vancouver, Canada, 9th International Conference on Signal, Image Processing and Pattern Recognition (SIPP 2021), 10th International Conference on Parallel, Distributed Computing Technologies and Applications (PDCTA 2021), 9th International Conference on Artificial Intelligence, Soft Computing (AISC 2021), 2nd International Conference on Natural Language Processing & Computational Linguistics (NLPCL 2021), 2nd International conference on Big Data, Machine learning and Applications (BIGML 2021) and 6th International Conference on Networks, Communications, Wireless and Mobile Computing (NCWMC 2021) was collocated with 11th International Conference on Computer Science and Information Technology (CCSIT 2021). -
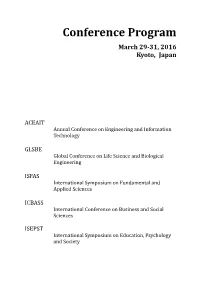
Conference Program
Conference Program March 29-31, 2016 Kyoto, Japan ACEAIT Annual Conference on Engineering and Information Technology GLSBE Global Conference on Life Science and Biological Engineering ISFAS International Symposium on Fundamental and Applied Sciences ICBASS International Conference on Business and Social Sciences ISEPST International Symposium on Education, Psychology and Society ACEAIT Annual Conference on Engineering and Information Technology ISBN 978-986-89298-6-9 GLSBE Global Conference on Life Science and Biological Engineering ISBN 978-986-5654-38-2 ISFAS International Symposium on Fundamental and Applied Sciences ISBN 978-986-89298-5-2 ICBASS International Conference on Business and Social Sciences ISBN 978-986-89298-7-6 ISEPST International Symposium on Education, Psychology and Society ISBN 978-986-89298-8-3 Content General Information for Participants ...................................................................................... 6 International Committees ............................................................................................................ 8 International Committee of ACEAIT ...................................................................................... 8 International Committee of GLSBE ........................................................................................ 9 International Committee of ISFAS ........................................................................................ 10 International Committee of ICBASS .................................................................................... -

Environmental Sciences/ Fundamental & Applied Sciences18 Social Studies / Psychology/ Business Management
Conference Program July 24-26, 2019 Bali, Indonesia ISEAS International Symposium on Engineering and Applied Science ICSSB International Conference on Social Science and Business ISEAS International Symposium on Engineering and Applied Science ISBN 978-986-5654-28-3 ICSSB International Conference on Social Science and Business ISBN 978-986-87417-7-5 Content Welcome Message ............................................................................................................................ 2 General Information for Participants ....................................................................................... 3 International Committees of Natural Sciences ...................................................................... 5 International Committees of Social Sciences.......................................................................... 8 Special Thanks to Session Chairs .............................................................................................. 11 Conference Venue Information ................................................................................................. 12 Conference Schedule ..................................................................................................................... 14 Natural Sciences Keynote Address ........................................................................................... 16 Social Sciences Keynote Address .............................................................................................. 17 Oral Sessions ................................................................................................................................... -

Curriculum Vitae
CURRICULUM VITAE IVAN Y. SUN Department of Sociology and Criminal Justice University of Delaware Newark, DE 19716 [email protected] (302) 831-8727 EDUCATION 2000 Ph.D. in Criminal Justice University at Albany, State University of New York, Albany, New York. 1997 M.A. in Criminal Justice University at Albany, State University of New York, Albany, New York. 1992 M.B.A. in Logistics, Operation, and Materials Management George Washington University, Washington D.C. 1982 B.A. in Economics Fu-Jen Catholic University, New Taipei City, Taiwan. EMPLOYMENT Teaching 09/12 – Present Professor, Department of Sociology and Criminal Justice, University of Delaware, Newark, DE. 09/05 – Present Faculty, Asian Studies, University of Delaware, Newark, DE. 09/06 – 08/12 Associate Professor, Department of Sociology and Criminal Justice, University of Delaware, Newark, DE. 09/04 – 08/06 Assistant Professor, Department of Sociology and Criminal Justice, University of Delaware, Newark, DE. 07/00 – 08/04 Assistant Professor, Department of Sociology and Criminal Justice, Old Dominion University, Norfolk, VA. 01/98 – 05/99 Graduate Teaching Instructor, School of Criminal Justice, University at Albany, State University of New York, Albany, NY. Research 05/96 – 08/96 Field Observer, Project on Policing Neighborhoods (POPN), School of Criminal Justice, Michigan State University, East Lansing, MI. Visiting Teaching/Research Professor 10/17 School of Law, Institute of Criminology, University of Leuven, Leuven, Belgium 09/17 School of Sociology, Central China Normal University, Wuhan, China 03/11 Department of Applied Social Sciences, City University of Hong Kong, Hong Kong, China. 09/10 – 01/11 Graduate Institute of Criminology, National Taipei University, New Taipei City, Taiwan. -

NIELSON-THESIS-2020.Pdf (850.0Kb)
ATTITUDINAL DIFFERENCES BETWEEN FEMALE AND MALE POLICE CADETS/OFFICERS IN TAIWAN: THE NEXUS BETWEEN GENDER, IMMIGRATION, AND CRIME ___________ A Thesis Presented to The Faculty of the Department of Criminal Justice and Criminology Sam Houston State University ___________ In Partial Fulfillment of the Requirements for the Degree of Master of Arts ___________ by Kyler R. Nielson August, 2020 ATTITUDINAL DIFFERENCES BETWEEN FEMALE AND MALE POLICE CADETS/OFFICERS IN TAIWAN: THE NEXUS BETWEEN GENDER, IMMIGRATION, AND CRIME by Kyler R. Nielson ___________ APPROVED: Jurg Gerber, PhD Thesis Director Yan Zhang, PhD Committee Member Furjen Deng, PhD Committee Member Phillip Lyons, PhD Dean, College of Criminal Justice DEDICATION This is dedicated to Amanda, Kenna, and Emmie for their constant love and support through it all. iii ABSTRACT Nielson, Kyler R., Attitudinal differences between female and male police cadets/officers in Taiwan: the nexus between gender, immigration, and crime. Master of Arts (Criminal Justice and Criminology), August, 2020, Sam Houston State University, Huntsville, Texas. Immigration is an increasingly salient issue throughout the world as the number of foreign residents continues to rise in many countries. In Taiwan, the foreign population has consistently increased in recent years. Immigrants in Taiwan are marginalized and are often subject to negative stereotypes from the media and public. As members of the public, police cadets/officers may be affected by such sentiments, but they should also maintain a neutral perspective and ensure equal treatment in various criminal justice processes. In particular, attitudes may differ based on cadet/officer gender. Males and females may have unique experiences in policing and inherent attitudinal differences. -

Wayfinding of Firefighters in Dark and Complex Environments
International Journal of Environmental Research and Public Health Article Wayfinding of Firefighters in Dark and Complex Environments Beckham Shih-Ming Lin 1 , Ching-Yuan Lin 1, Chun-Wei Kung 2, Yong-Jun Lin 3, Chung-Chyi Chou 4, Ying-Ji Chuang 1 and Gary Li-Kai Hsiao 5,* 1 Department of Architecture, National Taiwan University of Science and Technology, Taipei City 106335, Taiwan; [email protected] (B.S.-M.L.); [email protected] (C.-Y.L.); [email protected] (Y.-J.C.) 2 Department of Environmental Engineering, Da-Yeh University, Changhua 515006, Taiwan; [email protected] 3 Center for Weather Climate and Disaster Research, National Taiwan University, Taipei City 10617, Taiwan; [email protected] 4 Department of Fire and Safety, Da-Yeh University, Changhua 515006, Taiwan; [email protected] 5 Department of Disaster Management, Taiwan Police College, Taipei City 11696, Taiwan * Correspondence: [email protected] Abstract: Firefighters searching in dark and complex environments might lose their orientation and endanger themselves at the fireground. This study conducted experiments in the Training Facility of the New Taipei City Fire Department (NTFD), Taiwan. The objective of the experiments was to analyze the profile of each firefighter by a 13-factor self-report survey and their wayfinding time in dark and complex environments (DCEs). The results showed that age might be a marginally significant factor, and fear of confinement might be a significant factor that could affect firefighters’ wayfinding time in the DCEs. The findings could provide strategies for improving the safety of Citation: Lin, B.S.-M.; Lin, C.-Y.; firefighters working in such environments. -

A Community Policing Project in Taiwan
Chinese Public Administration CPAR Review Volume xx Issue x, Online First A Community Policing Project in Taiwan: The Developments, Challenges, and Prospects of Neighborhood Watch Fei-Lin Chen Taiwan Police College, Taiwan Neighborhood Watch is a community crime prevention program organized mainly by local residents to maintain order and deter crime. Neighborhood Watch is an important element of community policing in Taiwan. Relying on previous research, this study illustrates the implementation process of Neighborhood Watch in Taiwan. Starting in the 1970s, Neighborhood Watch in Taiwan evolved through several stages, shifting from a focus on moral alignment to community building and crime prevention. The central pillar of Neighborhood Watch is civilian patrol groups commonly organized by either the government at all levels as part of their civilian defense scheme or neighborhood patrol squads staffed by local volunteers. The organization and resources associated with Neighborhood Watch elucidate the government’s intention to integrate the program into community policing as an effective tool for building community safety and strengthening crime prevention. It is reasonable to predict that the Taiwanese government and police are likely to continue their support for the operation of Neighborhood Watch as part of collective efforts to build healthy and safe communities. Keywords: Neighborhood Watch; Taiwan police; civilian patrol squads; community policing; Taiwan INTRODUCTION policing in general (Kuo, & Shih, 2018; Wang, 2007) and Neighborhood Watch programs in Taiwan eighborhood Watch has received much in particular (Lee et al., 2000), none of them have attention in recent years due to its crime analyzed the implementation of Neighborhood Watch Nprevention value, which strengthens informal with a focus on policy analysis. -

Taiwan, March 2005
Library of Congress – Federal Research Division Country Profile: Taiwan, March 2005 COUNTRY PROFILE: TAIWAN March 2005 COUNTRY Formal Name: Taiwan (台灣); formally, Republic of China (Chung-hua Min-kuo—中華民國). Short Form: Taiwan (台灣). Term for Citizen(s): Chinese (Hua-jen—華人); Taiwanese (T’ai-wan-jen—台灣 人). Capital: The capital of central administration of Taiwan is Click to Enlarge Image Taipei (T’ai-pei—台北—literally, Taiwan North), located in T’ai-pei County in the north. Since 1967, Taipei has been administratively separate from Taiwan Province. Major Cities: The largest city is Taipei, with 2.6 million inhabitants in 2004. Other large cities are Kao-hsiung, with 1.5 million, and T’ai-chung, with 1 million. Fifteen other cities have populations ranging from 216,000 to 749,000 inhabitants. National Public Holidays: Founding Day (January 1, marking the founding of the Republic of China in 1912); Lunar New Year (also called Spring Festival, based on the lunar calendar, occurs between January 21 and February 19 and is preceded by eight days of preparatory festivities); Peace Memorial Day (February 28, commemorating the February 28, 1947, incident); Tomb Sweeping Day (Ching Ming, April 4); Dragon Boat Festival (fifth day of the fifth lunar month, movable date in June); Mid-Autumn Festival (15th day of the eighth lunar month, movable date in September); and Double Tenth National Day (October 10, also called Republic Day, commemorates the anniversary of the Chinese revolution in 1911 and the date from which years are sometimes counted). Also -

Hsu Jen-Shuo Phd Student, Graduate School of Law, Hokkaido University, Japan Taiwanese Police
The new challenge of Taiwanese police reform: performance management problem Hsu Jen-Shuo PhD student, Graduate School of Law, Hokkaido University, Japan Taiwanese police Size:64,800 officers(of 2,300,000 citizen) Hierarchy: Excutive Yuan(Cabinet)-Ministry of the Interior-National Police Agency(NPA) Ranks and Recruitment: Rank and File (Graduated or trained by Taiwan police college) Lieutenant, Director (Graduated or trained by Central police university) Crime Rate: 1,253 cases (per 100,000 citizen)(2016) History:Japanese Colonial(1895-9845)->Martial Law(1945-1987)- >Democracy(1987~) Changing after democratization Martial Law Period Democratic Period Ruling Party(KMT) Central Citizens Government Central Government Army Local Police Government (Central/Local) Military Police Police But…… What will happen while a police system without internal democracy faces democracy politic? The performance policy problem in judicial reform conference 2017 Judicial reform conference Under president. Second conference since 1999. The problem of performance policy was proposal by both judicial reform and police reform NGOs. The performance policy KPI (Key Performance Indicator) on specific time, area, number of cases or strategy of policing. Competition between different police precinct. Problems of performance policy Inefficiency and selective investigation Overwork Encouraging unjust and illegal policing Interrupting investigation and prosecution Response of NPA Data based KPI. No relating to promotion and punishment. Respecting local branches. Strict Monitoring. Discussion in conference More transparency and accountability. KPI does matter. Supervisor responsibility of NPA. Solving overwork problem Conclusion of conference and challenge Police Project and Performance Management Committee. under Ministry of the interior. half member should be rank and file officer and outsider expert. -

How the Sex Industry Market Determines the Distribution Of
How the Sex Industry Market Determines the Distribution of Smuggling Hot Spots in Taiwan: An Empirical Study of Illegal Immigration of Mainland Chinese Females to Taiwan Wang-Ting Lin and Cathy Tzu-Hsing Chen† Smuggling Mainland Chinese females into Taiwan has been a devastating problem in the past two decades, due to the fact that China and Taiwan are geographically close to each other and the fact that no major differences exist between these two places with respect to language and ethnic composition. The persistent attraction of huge profits resulting from smuggling is mainly responsible for this serious criminal problem. This paper is an extended study of previous research reported at the Annual ANZSOC conference (Chen 2006) where it was shown that, whether voluntary or coerced by Human Snake gangs (ie. criminal organisations responsible for illegally transporting people across borders), a majority of Mainland Chinese females smuggled into Taiwan are involved in the sex industry. The present research project, which continues to build on the key insight of the previous study, indicates that the need for, and supply of, sex industry workers in Taiwan substantively influences the smuggling of females. The focus of this research project is to investigate the co-variation between crime hot spots and the sex industry in Taiwan. We divided Taiwan into four areas - East, West, South and North - and examined the number of female illegal immigrants in these four areas, which encompass both coastal and inland areas. The results show that significant differences exist among these four areas. More specifically, the demands of the sex industry market in an area is positively correlated with the number of illegal immigrant females arrested. -
Towards Democratic Policing in Taiwan: a Longitudinal Study of the Effects of Police Education on Human Rights, Moral Reasoning
Towards Democratic Policing in Taiwan: A Longitudinal Study of the Effects of Police Education on Human Rights, Moral Reasoning, Prejudice and Receptivity to Evidence- Based Policing Keng-Hui Lin Department of Security and Crime Science University College London This Thesis is submitted in support of a PhD in Security and Crime Science August 2020 1 Declaration of Authorship ‘I, Keng-hui Lin, confirm that the work presented in this thesis is my own. Where information has been derived from other sources, I confirm that this has been indicated in the thesis.' Signed: Date: 2 Towards Democratic Policing in Taiwan and Police Education Abstract This thesis investigates how police socialisation, and in particular police education, influences police recruits in terms of several democratic policing indicators (DPI) and their receptivity to evidence-based policing (EBP). The DPI used here are derived from prior research and theory, namely: 1) human rights endorsement, 2) advanced moral reasoning, and 3) lack of prejudice. To observe temporal changes in DPI and receptivity to EBP, this thesis applies a multiple-group longitudinal design that includes both police recruits and university undergraduates (as a comparison group). This sample takes advantage of the centralised police education system in Taiwan – Central Police University (CPU) – and the fact that there is only one criminology department in Taiwan – National Chung Cheng University (NCCU). The sample used here comprises five cohorts: 1) police officers on in-service programs, 2) graduate recruits in police academy training, 3) new and 4) senior recruits on cadre programs at CPU, and 5) first-year undergraduates at NCCU. -
Curriculum Vitae
CURRICULUM VITAE IVAN Y. SUN Department of Sociology and Criminal Justice University of Delaware Newark, DE 19716 [email protected] (302) 831-8727 EDUCATION 2000 Ph.D. in Criminal Justice University at Albany, State University of New York, Albany, New York. 1997 M.A. in Criminal Justice University at Albany, State University of New York, Albany, New York. 1992 M.B.A. in Logistics, Operation, and Materials Management George Washington University, Washington D.C. 1982 B.A. in Economics Fu-Jen Catholic University, Taipei County, Taiwan. EMPLOYMENT Teaching 09/12 – Present Professor, Department of Sociology and Criminal Justice, University of Delaware, Newark, DE. 09/05 – Present Faculty, Asian Studies, University of Delaware, Newark, DE. 09/06 – 08/12 Associate Professor, Department of Sociology and Criminal Justice, University of Delaware, Newark, DE. 09/10 – 01/11 Visiting Associate Professor, Graduate School of Criminology, National Taipei University, Taipei, Taiwan. 09/04 – 08/06 Assistant Professor, Department of Sociology and Criminal Justice, University of Delaware, Newark, DE. 07/00 – 08/04 Assistant Professor, Department of Sociology and Criminal Justice, Old Dominion University, Norfolk, VA. 01/98 – 05/99 Graduate Teaching Instructor, School of Criminal Justice, University at Albany, State University of New York, Albany, NY. Research 05/96 – 08/96 Field Observer, Project on Policing Neighborhoods (POPN), School of Criminal Justice, Michigan State University, East Lansing, MI. Other 08/99 – 06/00 Undergraduate Advisor, School of Criminal Justice, University at Albany, State University of New York, Albany, NY. 09/96 – 12/97 Consultant, Rockefeller College Computer Lab, University at Albany, State University of New York, Albany, NY.