A Large Spatial Survey of Colistin-Resistant Gene Mcr-1-Carrying E
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Study in Taiwan - 7% Rich and Colorful Culture - 15% in Taiwan, Ancient Chinese Culture Is Uniquely Interwoven No.7 in the Fabric of Modern Society
Le ar ni ng pl us a d v e n t u r e Study in Foundation for International Cooperation in Higher Education of Taiwan (FICHET) Address: Room 202, No.5, Lane 199, Kinghua Street, Taipei City, Taiwan 10650, R.O.C. Taiwan Website: www.fichet.org.tw Tel: +886-2-23222280 Fax: +886-2-23222528 Ministry of Education, R.O.C. Address: No.5, ZhongShan South Road, Taipei, Taiwan 10051, R.O.C. Website: www.edu.tw www.studyintaiwan.org S t u d y n i T a i w a n FICHET: Your all – inclusive information source for studying in Taiwan FICHET (The Foundation for International Cooperation in Higher Education of Taiwan) is a Non-Profit Organization founded in 2005. It currently has 114 member universities. Tel: +886-2-23222280 Fax: +886-2-23222528 E-mail: [email protected] www.fichet.org.tw 加工:封面全面上霧P 局部上亮光 Why Taiwan? International Students’ Perspectives / Reasons Why Taiwan?1 Why Taiwan? Taiwan has an outstanding higher education system that provides opportunities for international students to study a wide variety of subjects, ranging from Chinese language and history to tropical agriculture and forestry, genetic engineering, business, semi-conductors and more. Chinese culture holds education and scholarship in high regard, and nowhere is this truer than in Taiwan. In Taiwan you will experience a vibrant, modern society rooted in one of world’s most venerable cultures, and populated by some of the most friendly and hospitable people on the planet. A great education can lead to a great future. What are you waiting for? Come to Taiwan and fulfill your dreams. -

Fooyin University Department of Midwifery and Maternal-Infant Health Care Name Yi-Ling Chiou Extension Number +886 7 7811151 Ex
Fooyin University Department of Midwifery and Maternal-Infant Health Care Name Yi-Ling Chiou Extension number +886 7 7811151 ext. 6147 Fax number +886 7 7821845 E-mail [email protected] Education Kaohsiung Medical University Nursing PhD Student background University of Minnesota Master Degree in Nursing Fooyin University Midwifery and Maternal-Infant Health Care Current Job Department, Lecturer Working Experience: Griffith University & The University of Sunshine Coast Visiting Scholar 108.1.13~108.2.02 University of North Carolina at Chapel Hill Visiting Scholar 107.1.18~107.7.20 Fooyin University Midwifery and Maternal-Infant Health Care Department Lecturer(Full time) 08/2001~now Cheng Shiu University Department of Early Childhood Care Lecturer (Part time) 05/2005~07/2005 Shuren Medical Junior College Nursing Department Lecturer (Full time) 08/2000~07/2001 Daren Institute Technology Nursing Department Lecturer (Full time) 08/1999~07/2000 Foo-yin Institute Technology Nursing Department Lecturer (Full time) 08/1998~07/1999 University of Minnesota Nursing Department Research Assistant (Part time) 05/1996~12/1996 Daren Junior College of Pharmacy Nursing Department Teaching Assistant (Full time) 07/1994~07/1995 Cathay Pacific Hospital Nursing Department Register Nurse (Full time) 09/1989~06/1991 Fooyin University Academic Expertise and Research Area: Midwifery care, Obstetrical care, Infant massage, Infant yoga, High risk pregnancy, Gestational diabetes, Doing the month care Research: The Impact of Prepregnancy Body Mass Index and Gestational Weight Gain on Perinatal Outcomes for Women with Gestational Diabetes Mellitus,Worldviews on Evidence-based Nursing,2018,15(4) To Explore the application of the relieve labor pain in using massage techniques: T.S.M.H. -

APANE (Asian and Pacific Alliance for Nursing Education)
Asian and Pacific Alliance for Nursing Education Opening Ceremony and International Congress Multi-culture Collaboration in Nursing Education Friday, September 6, 2019 9:00 am Registration & Networking Opening Remarks 10:20 am CHAIR: Jing-Jy Wang 王靜枝, Chair of APANE Preparation Committee Keynote speech─ Nursing leadership: Bridging education and practice SPEAKER: 11:05 am MODERATOR: Professor Lian-Hua Huang 黃璉華 Hsiu-Hung Wang 王秀紅, President of Taiwan Nurses Association (TWNA) ICN Board Member 12:00 pm Lunch & Poster Exhibition, Networking Plenary speech ─Sustainable Development Goals and nursing education MODERATOR: SPEAKER: 1:30 pm Yu-Yun Hsu 許⽟雲, President of Taiwan Association of Nursing Education (TANE) Director Johnson Huang 黃兆聖 AdvMeds Co., Ltd., Taiwan Professor Patsy Yates Yann-Fen Chiou Chao 邱艷芬, Chair of College of Nursing, Hungkuang University Queensland University of Technology, Australia Associate Professor and Dean Yajai Sitthimongkol Shao-Yu Tsai 蔡劭瑜, Professor of School of Nursing, National Taiwan University ยาใจ สิทธิมงคล Mahidol University, Thailand 2:45 pm Refreshment Break & Poster Exhibition, Networking Partner Presentations & Exhibitions Jing-Jy Wang 王靜枝, Chair of Fan-Hao Chou 周汎澔, Vice Chair of Ying-Ju Chang 張瑩如, Director of APANE Preparation Committee Education Committee of TANE Nursing Department, NCKU Hospital 1. Asia University 12. Fu Jen Catholic University 22. National Taipei University of 2. Chang Gung University of Science 13. Hungkuang University Nursing and Health Sciences and Technology 14. Pham Ngoc Thach University of 23. National Taiwan University 3. Chang Jung Christian University Medicine 24. University of Puthisastra 3:00 pm 4. Association of Indonesian Nurse 15. Kaohsiung Medical University 25. National Yang-Ming University Education Center 16. -
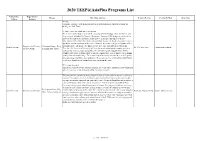
2020 TEEP@Asiaplus Programs List
2020 TEEP@AsiaPlus Programs List University / Department / Theme Brief Introduction Contact Person Contact E-Mail More Info College Institute ## Title: Ultrasonic Guidance System and Measurement Stand for Image Analysis of Artificial Intelligence Soft Tissue ## Project objectives and expected benefits: The features of this project focus on the category of biotechnology, smart machinery, and deep learning. Although the Magnetic Resonance Imaging (MRI) images are deliberate to know the location of the soft tissue injury, however, it is not convenient to operate immediately in the clinic. One of the standard clinic measure methods, ultrasound image, is quick and convenient to take in the clinic. However, the scanning angle and posture of the Department of Creative Ultrasound Image, Deep ultrasound probe often affect the image quality and cause difficulty in interpretation. Asia University Dr. Chi-Wen Lung [email protected] Product Design Learning, Soft Tissue. Therefore, the first step of this study will develop an ultrasound probe support system to accuracy the scanning angle and posture. The ultrasound probe support system will be automatically adjusted during different patient scanning processes to improve the scanning quality of the ultrasonic image. The second step of this study will take these benefit quality ultrasonic images to further data analyses in Deep learning. The results of this study would be better to classify the location of soft tissue injury in the clinic. ## Fee and dormitory This project offers $ 500 per person per month. The University can provide paid dormitories (4 beds / room) at a cost of about $ 100 per person per month. This program is a customized study program designed in particular for our sister university students. -

Department of Midwifery and Maternal-Infant Health Care
Fooyin University Department of Midwifery and Maternal-Infant Health Care Name Han-Fu Cheng Extension number +886 7 7811151 ext. 5477 Fax number +886 7 7821845 E-mail [email protected] Education Saint Louis University, USA background Current Job Assistant Professor Working Experience: School of Nursing, Saint Louis University. Research Assistant 2006/08-2008/06 Department of Early Childhood Care and Education, Cheng Shiu University. Instructor 2004/02-2004/07 Department of Obstetrics & Gynecology, Fooyin University Hospital. Nurse 1999/09-2004/07 Nursing Department, Meiho University. Instructor 1999/08-2000/07 Department of Nursing, Taipei City Hospital Yangming Branch. Nurse 1993/10-1997/09 Nursing Department, Kaohsiung Chang Gung Memorial Hospital. Nurse 1987/07-1993/10 Academic Expertise and Research Area: Women’s Health, Maternal and Fetal Care, Childbirth Care, and Perinatal Care Research: Fooyin University Publication 1. Midwifery 2-year program undergraduate students clinical practicum III experiences midwifery students (2012). The Journal of Midwifery, 54. 2. Perimenstrual Syndrome: Nursing Diagnosis Among Taiwanese Nursing Students (2011). International Journal of Nursing Terminologies and Classifications, 22(3). 3. The issue and it’s care of Infant and Toddler (2011). The Journal of Fooyin University, 69. 4. Factors Influencing Southern Taiwanese Men’s Acceptance of Prostate-Specific Antigen (2011). International Journal of Urological Nursing, 5(2). 5. Perinatal Nutrition (2011). The Journal of Fooyin University, 68. 6. Management of Perimenstrual Symptoms among Young Taiwanese Nursing Students (2011). Journal of Clinical Nursing, 20(7-8). 7. Selection and Efficacy of Self-Management Strategies for Dysmenorrhea in Young Taiwanese Women (2011). Journal of Clinical Nursing, 20(7-8). -

The Rankings of Research Funding Among Universities in Taiwan
Mar. 2010, Volume 7, No.3 (Serial No.64) US-China Education Review, ISSN 1548-6613, USA The rankings of research funding among universities in Taiwan WANG Ru-Jer (Department of Education, Graduate Institute of Educational Policy and Administration, National Taiwan Normal University, Taipei 106, Taiwan) Abstract: With the current trend that universities around the world have gradually stepped into higher education systems of popularization, there has been more diversity in universities; hence it has become necessary to increase the transparency of university governance. Since that university classification or university ranking is a powerful mechanism to demonstrate the diversity of an institute, the rankings of research funding have become desirable and also of great value. The main purpose of this study is to analyze the rankings of research funding among universities in Taiwan, and make relevant suggestions based on the findings. A secondary data analysis was conducted on the data obtained from the database of National Science Council, in order to develop the rankings of research funding among 164 universities in Taiwan. Based on the results, the conclusions are as follows: (1) The top three universities which won the funding of the National Science Council Research Project with the best overall strength were National Taiwan University, National Cheng Gung University, and National Chiao Tung University; (2) The top three universities which won the funding of the National Science Council Research Project with the best average faculty strength were National Tsing Hua University, National Chiao Tung University, and National Taiwan University. It is suggested that, when rating the strength of a university to win the research funding, both overall strength and average faculty strength should be considered to avoid the unfairness towards universities of smaller scale. -

Heteronemin Suppresses Lymphangiogenesis Through ARF-1 and MMP-9/VE-Cadherin/Vimentin
biomedicines Article Heteronemin Suppresses Lymphangiogenesis through ARF-1 and MMP-9/VE-Cadherin/Vimentin Hsien-Lin Chen 1,†, Yu-Chieh Su 2,3,†, Huang-Chi Chen 4,5, Jui-Hsin Su 6, Chang-Yi Wu 7,8, Shih-Wei Wang 9,10 , In-Pin Lin 11, Chung-Yi Chen 12 and Chien-Hsing Lee 13,14,15,* 1 Division of General Surgery, Department of Surgery, Liuying Chi-Mei Medical, Tainan 73657, Taiwan; [email protected] 2 Department of Medicine, School of Medicine, I-Shou University, Kaohsiung 840203, Taiwan; [email protected] 3 Division of Hematology-Oncology, Department of Internal Medicine, E-Da Hospital, Kaohsiung 824410, Taiwan 4 Department of Internal Medicine, Kaohsiung Municipal Siaogang Hospital, Kaohsiung 81267, Taiwan; [email protected] 5 Division of Pulmonary and Critical Care Medicine, Department of Internal Medicine, Kaohsiung Medical University Hospital, Kaohsiung 80708, Taiwan 6 National Museum of Marine Biology & Aquarium, Institute of Marine Biotechnology, National Dong Hwa University, Pingtung 94401, Taiwan; [email protected] 7 Department of Biotechnology, Kaohsiung Medical University, Kaohsiung 80708, Taiwan; [email protected] 8 Department of Biological Sciences, National Sun Yat-Sen University, Kaohsiung 804201, Taiwan 9 Department of Medicine, Mackay Medical College, New Taipei City 252005, Taiwan; [email protected] 10 Graduate Institute of Natural Products, College of Pharmacy, Kaohsiung Medical University, Citation: Chen, H.-L.; Su, Y.-C.; Kaohsiung 80708, Taiwan Chen, H.-C.; Su, J.-H.; Wu, C.-Y.; 11 Department of Pharmacology, College of Medicine, Kaohsiung Medical University, Kaohsiung 80708, Taiwan; Wang, S.-W.; Lin, I.-P.; Chen, C.-Y.; [email protected] Lee, C.-H. -

Surface Antimicrobial Effects of Zr61al7.5Ni10cu17.5Si4 Thin Film
Fooyin J Health Sci 2010;2(1):12−20 ORIGINAL ARTICLE Surface Antimicrobial Effects of Zr61Al7.5Ni10Cu17.5Si4 Thin Film Metallic Glasses on Escherichia coli, Staphylococcus aureus, Pseudomonas aeruginosa, Acinetobacter baumannii and Candida albicans Pai-Tsung Chiang1,2*, Guo-Ju Chen1, Sheng-Rui Jian1, Yung-Hui Shih1, Jason Shian-Ching Jang3, Chung-Hsu Lai4 1Department of Materials Science and Engineering, I-Shou University, Kaohsiung, Taiwan 2Department of Plastic Surgery, Fooyin University Hospital, Pingtung, Taiwan 3Department of Mechanical Engineering, Institute of Materials Science and Engineering, National Central University, Chung-Li, Taiwan 4Department of Infectious Disease, I-Shou University, Kaohsiung, Taiwan Received: November 11, 2009 Revised: January 21, 2010 Accepted: February 8, 2010 Zr61Al7.5Ni10Cu17.5Si4 (ZrAlNiCuSi) thin film metallic glasses (TFMGs) can modify the surface of 304 stainless steel, and they are widely used in health care systems. We investigated modified surfaces with ZrAlNiCuSi TFMGs and their anti- microbial effects on those five microbes which are the most common nosocomial infection pathogens. The transfor- mation of ZrAlNiCuSi bulk metallic glass into TFMG was achieved by sputtering onto stainless steel. Escherichia coli, Staphylococcus aureus, Pseudomonas aeruginosa, Acinetobacter baumannii and Candida albicans were then isolated. The microbes were sampled on ZrAlNiCuSi TFMGs, and this was compared with stainless steel plates. After microbe− material interaction under humidity at room temperature for 3 hours, the specimens were attached to a Mueller- Hinton agar plate (Gibco, Middleton, WI, USA) and incubated at 37.0ºC for 24, 48 and 96 hours. The areas of microbe growth were recorded by serial subtraction photography and then assessed using Image-Pro Plus software (Media Cybernetics, Bethesda, MD, USA). -

The Effect of Tertiary Education Expansion on Fertility: a Note on Identification
DISCUSSION PAPER SERIES IZA DP No. 14672 ‘Bachelors’ and Babies: The Effect of Tertiary Education Expansion on Fertility Tushar Bharati Simon Chang Qing Li AUGUST 2021 DISCUSSION PAPER SERIES IZA DP No. 14672 ‘Bachelors’ and Babies: The Effect of Tertiary Education Expansion on Fertility Tushar Bharati Qing Li University of Western Australia Business Shanghai University School Simon Chang University of Western Australia Business School and IZA AUGUST 2021 Any opinions expressed in this paper are those of the author(s) and not those of IZA. Research published in this series may include views on policy, but IZA takes no institutional policy positions. The IZA research network is committed to the IZA Guiding Principles of Research Integrity. The IZA Institute of Labor Economics is an independent economic research institute that conducts research in labor economics and offers evidence-based policy advice on labor market issues. Supported by the Deutsche Post Foundation, IZA runs the world’s largest network of economists, whose research aims to provide answers to the global labor market challenges of our time. Our key objective is to build bridges between academic research, policymakers and society. IZA Discussion Papers often represent preliminary work and are circulated to encourage discussion. Citation of such a paper should account for its provisional character. A revised version may be available directly from the author. ISSN: 2365-9793 IZA – Institute of Labor Economics Schaumburg-Lippe-Straße 5–9 Phone: +49-228-3894-0 53113 Bonn, Germany -

Academic Catalog 2015-2016
ACADEMIC CATALOG 2015-2016 2015 Fall 2015, Spring 2016, Summer 2016 2016 CATALOG University of the West has made every effort to ensure the information in this catalog and other published materials is accurate. University of the West reserves the right to change policies, tuition, fees, and other information in this catalog, with prior approval from the WASC Senior College and University Commission (WSCUC) where applicable. University of the West strives to inform students and stakeholders of changes in a timely fashion, but reserves the right to make changes without notice. University of the West is a private, non-profit, WSCUC-accredited campus founded by and affiliated with the Taiwan-based Buddhist order of Fo Guang Shan. The University of the West name, abstract lotus logo, and calligraphic logo are copyrighted to the university. Additional information is available at our website, www.uwest.edu. University of the West does not discriminate on the basis of sex, gender, age, race, color, religion, status as a veteran, physical disability, sexual orientation, gender identity, and/or national and ethnic origin in its educational programs, student activities, 1409 Walnut Grove Avenue, Rosemead, CA 91770 employment, or admission policies, in the administration of its scholarship and loan programs, or in any other school- Telephone 626.571.8811 administered programs. This policy complies with requirements of the Internal Revenue Service Procedure 321-1, Title VI of the Fax 626.571.1413 Civil Rights Act, and Title IX of the 1972 Educational Amendments Email [email protected] as amended and enforced by the Department of Health and Human Services. -
Study-In-Taiwan.Pdf
Table of Contents 1 Why Taiwan ? Study in Why Taiwan | 02 International Students’ Perspectives / Reason | 03 Taiwan! Getting to Know Taiwan Fascinating Taiwan | 08 2 History | 10 Climate | 10 Geography | 10 Culture | 11 Cuisine | 11 3 Campus Diary | 12 Studying in Taiwan The Educational System of Taiwan | 14 Choosing a School & Applying | 16 Knowing the Schools | 18 International Programs | 20 Visa & Arrival Information | 62 Scholarships | 64 Campus Diary | 68 4 Living in Taiwan FICHET: Your all – Accommodations | 70 Living cost | 70 Services | 72 inclusive information source Job Opportunities | 73 Campus Diary | 74 for studying in Taiwan FICHET (The Foundation for International Cooperation in Higher Education of Taiwan) Additional Information is TAIWAN?a Non-Profit Organization founded in 2005. It currently has 118 member universities. Useful Links | 76 Universities in Taiwan | 82 Chinese Language Centers | 88 ͙Why Taiwan? Tel: +886-2-23222280 Test of Chinese as a Foreign language (TOCFL) | 90 5 Fax: +886-2-23222528 International Students in Taiwan (Statistics) | 92 International Students’E-mail: [email protected] / Reasons www.fichet.org.tw ͙ The Reasons Why I Chose Taiwan Let’s listen to what international students say on “Why Taiwan?” Sharoon 1 Swaziland Why Taiwan? Identification Lungile Hlatshwayo Degree student Taiwan has an outstanding higher education system that provides opportunities for international students to Major Healthcare administration study a wide variety of subjects, ranging from Chinese language and history to tropical agriculture and forestry, genetic engineering, business, semi-conductors and more. Chinese culture holds education and scholarship in high Grade nd regard, and nowhere is this truer than in Taiwan. -

Application of Factor Analysis for Characterizing the Relationships Between Groundwater Quality and Land Use in Taiwan’S Pingtung Plain
sustainability Article Application of Factor Analysis for Characterizing the Relationships between Groundwater Quality and Land Use in Taiwan’s Pingtung Plain Ching-Ping Liang 1, Chia-Hui Wang 2, Sheng-Wei Wang 3 , Ta-Wei Chang 4 and Jui-Sheng Chen 2,* 1 Department of Nursing, Fooyin University, Kaohsiung City 831, Taiwan; [email protected] 2 Graduate Institute of Applied Geology, National Central University, Taoyuan City 320, Taiwan; [email protected] 3 Department of Water Resource and Environmental Engineering, Tamkang University, New Taipei City 251, Taiwan; [email protected] 4 Agricultural Engineering Research Center, Taoyuan City 320, Taiwan; [email protected] * Correspondence: [email protected]; Tel.: +886-2807427; Fax: +886-3-4263127 Received: 16 October 2020; Accepted: 23 November 2020; Published: 18 December 2020 Abstract: Although the average municipal water coverage in Taiwan is quite high, at 93.91%, only around half of the residents in the Pingtung Plain use tap water originating from the Taiwan Water Corporation to meet their needs. This means the exploitation of a substantial amount of groundwater as a source of water to meet drinking, agriculture, aquaculture, and industry requirements. Long-term groundwater quality surveys in Taiwan have revealed obvious contamination of the groundwater in several locations in the Pingtung Plain, with measured concentration levels of some groundwater quality parameters in excess of the permissible levels specified by the Taiwan Environmental Protection Administration. Clearly, establishing a sound plan for groundwater quality protection in this area is imperative for maximizing the protection of human health. The inappropriate use of hazardous chemicals and poor management of land use have allowed pollutants to permeate through unsaturated soil and ultimately reach the underlying shallow unconfined groundwater system.