Phytochemical and Antimicrobial Studies of the Methanol Extract of the Root of Napoleonaea Heudelotti (A.Juss)
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Lecythidaceae (G.T
Flora Malesiana, Series I, Volume 21 (2013) 1–118 LECYTHIDACEAE (G.T. Prance, Kew & E.K. Kartawinata, Bogor)1 Lecythidaceae A.Rich. in Bory, Dict. Class. Hist. Nat. 9 (1825) 259 (‘Lécythidées’), nom. cons.; Poit., Mém. Mus. Hist. Nat. Paris 13 (1835) 141; Miers, Trans. Linn. Soc. London, Bot. 30, 2 (1874) 157; Nied. in Engl. & Prantl, Nat. Pflanzenfam. 3, 7 (1892) 30; R.Knuth in Engl., Pflanzenr. IV.219, Heft 105 (1939) 26; Whitmore, Tree Fl. Malaya 2 (1973) 257; R.J.F.Hend., Fl. Australia 8 (1982) 1; Corner, Wayside Trees Malaya ed. 3, 1 (1988) 349; S.A.Mori & Prance, Fl. Neotrop. Monogr. 21, 2 (1990) 1; Chantar., Kew Bull. 50 (1995) 677; Pinard, Tree Fl. Sabah & Sarawak 4 (2002) 101; H.N.Qin & Prance, Fl. China 13 (2007) 293; Prance in Kiew et al., Fl. Penins. Malaysia, Ser. 2, 3 (2012) 175. — Myrtaceae tribus Lecythideae (A.Rich.) A.Rich. ex DC., Prodr. 3 (1828) 288. — Myrtaceae subtribus Eulecythideae Benth. & Hook.f., Gen. Pl. 1, 2 (1865) 695, nom. inval. — Type: Lecythis Loefl. Napoleaeonaceae A.Rich. in Bory, Dict. Class. Hist. Nat. 11 (1827) 432. — Lecythi- daceae subfam. Napoleonoideae Nied. in Engl. & Prantl., Nat. Pflanzenfam. 3, 7 (1893) 33. — Type: Napoleonaea P.Beauv. Scytopetalaceae Engl. in Engl. & Prantl, Nat. Pflanzenfam., Nachtr. 1 (1897) 242. — Lecythidaceae subfam. Scytopetaloideae (Engl.) O.Appel, Bot. J. Linn. Soc. 121 (1996) 225. — Type: Scytopetalum Pierre ex Engl. Lecythidaceae subfam. Foetidioideae Nied. in Engl. & Prantl, Nat Pflanzenfam. 3, 7 (1892) 29. — Foetidiaceae (Nied.) Airy Shaw in Willis & Airy Shaw, Dict. Fl. Pl., ed. -
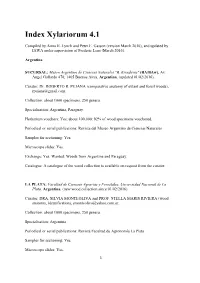
Index Xylariorum 4.1
Index Xylariorum 4.1 Compiled by Anna H. Lynch and Peter E. Gasson (version March 2010), and updated by IAWA under supervision of Frederic Lens (March 2016). Argentina SUCURSAL: Museo Argentino de Ciencias Naturales "B. Rivadavia" (BA/BAw), Av. Ángel Gallardo 470, 1405 Buenos Aires, Argentina. (updated 01/02/2016). Curator: Dr. ROBERTO R. PUJANA (comparative anatomy of extant and fossil woods), [email protected]. Collection: about 1000 specimens, 250 genera. Specialisation: Argentina, Paraguay. Herbarium vouchers: Yes; about 100,000; 92% of wood specimens vouchered. Periodical or serial publications: Revista del Museo Argentino de Ciencias Naturales Samples for sectioning: Yes. Microscope slides: Yes. Exchange: Yes. Wanted: Woods from Argentina and Paraguay. Catalogue: A catalogue of the wood collection is available on request from the curator. LA PLATA: Facultad de Ciencias Agrarias y Forestales, Universidad Nacional de La Plata. Argentina. (new wood collection since 01/02/2016). Curator: DRA. SILVIA MONTEOLIVA and PROF. STELLA MARIS RIVIERA (wood anatomy, identification), [email protected]. Collection: about 1000 specimens, 250 genera. Specialisation: Argentina Periodical or serial publications: Revista Facultad de Agronomía La Plata Samples for sectioning: Yes. Microscope slides: Yes. 1 Exchange: Yes. Wanted: woods from Argentina. Catalogue: A catalogue of the wood collection is available on request from the curator: www.maderasenargentina.com.ar TUCUMAN: Xiloteca of the Herbarium of the Fundation Miguel Lillo (LILw), Foundation Miguel Lillo - Institut Miguel Lillo, (LILw), Miguel Lillo 251, Tucuman, Argentina. (updated 05/08/2002). Foundation: 1910. Curator: MARIA EUGENIA GUANTAY, Lic. Ciencias Biologicas (anatomy of wood of Myrtaceae), [email protected]. Collection: 1,319 specimens, 224 genera. -

Public Health Implications of Continuous Ethnomedical Use of Some Plant Species Encounterd in Enyigba Lead-Zinc Mining Community of Ebonyi State, Nigeria
IOSR Journal of Environmental Science, Toxicology and Food Technology (IOSR-JESTFT) e-ISSN: 2319-2402,p- ISSN: 2319-2399.Volume 13, Issue 6 Ser. II (June. 2019), PP 62-68 www.iosrjournals.org Public Health Implications of Continuous Ethnomedical Use of Some Plant Species Encounterd in Enyigba Lead-Zinc Mining Community of Ebonyi State, Nigeria Shu Elvis N1, Otuu Fred C2*, Maduka Ignatius3, Tilako Bello H4, Nwadinigwe Alfreda O5, Ogbodo Ogbonna6, Nwando Obi-Ezeani7 1Deptartment of Pharmacology and Therapeutics, College of Medicine, University of Nigeria, Nsukka 2Department of Pharmaceutics, University of Nigeria, Nsukka 3Department of Human Biochemistry, Nnamdi Azikiwe University, Awka, Nigeria 4State Ministry of Health, Gombe, Gombe State, Nigeria 5Department of Plant Science and Biotechnology, University of Nigeria, Nsukka 6Department of Medical Biochemistry, Faculty of Basic Medical Sciences, College of Medicine, Enugu State University of Science and Technology, Enugu. 7Department of Chemical Pathology, College of Medicine, Chukwuemeka Odumegwu Ojukwu University, Awka, Anambra State, Nigeria *Corresponding Author: Otuu Fred C., Abstract: Introduction: The Public health implications of continuous ethnomedical use of some plant species encountered at Enyigba lead-zinc mining community, Ebonyi State, Nigeria were examined. Methodology: Plant species growing around the mining site were identified by a Botanical Taxonomist. Well structured questionnaires designed to reflect demography, the prevalent diseases among the inhabitants of the community and some common plants used in the management of the diseases were administered. Available literature on the heavy metal contents of soil and plants in the study area and its neighbourhood was searched. Results: One hundred and fifty (150) questionnaires were administered to males (48.7%) and females (51.3%) with 100% response. -

Evaluation of Antimicrobial Properties of Ethyl Acetate Extract of the Leaves of Napoleoneae Imperialis Family Lecythiaceae A.F
Int. J. Drug Res. Tech. 2011, Vol. 1 (1), 45-51 International Journal of Drug Research and Technology Available online at http://www.ijdrt.com/ Original Research Paper EVALUATION OF ANTIMICROBIAL PROPERTIES OF ETHYL ACETATE EXTRACT OF THE LEAVES OF NAPOLEONEAE IMPERIALIS FAMILY LECYTHIACEAE A.F. Onyegbule1*, C.F. Anowi2, T.H. Gugu3 and A.U. Uto-Nedosa4 1* Dept of Pharmaceutical and Medicinal Chemistry, Faculty of Pharmaceutical Sciences, Nnamdi Azikiwe University, Awka, Nigeria 2Dept of Pharmacognosy and Traditional Medicine, Faculty of Pharmaceutical sciences, Nnamdi Azikiwe University, Awka, Nigeria 3 Dept of Pharmaceutical Microbiology and Biotechnology, Faculty of Pharmaceutical Sciences, Nnamdi Azikiwe University, Awka, Nigeria 4Dept of Pharmacology and Toxicology, Faculty of Pharmaceutical Sciences, Nnamdi Azikiwe University, Awka, Nigeria ABSTRACT Napoleonaea imperialis is used to treat wounds in Anambra State, Nigeria. Against this background, ethyl acetate extract of the leaves were screened against some microorganisms so as to ascertain this claim and to recommend it for further investigation for possible inclusion into official compendium. The plant leaves were dried, powdered subjected to cold maceration with ethyl acetate for 24 hours. Phytochemical screening was done for alkaloids, saponin, essential oil, phenolic group, steroidal nucleus, simple sugar, starch, cyanogenic glycoside, proteins and flavonoid using standard procedures. Antimicrobial screenings were done using agar diffusion technique. Antibacterial activity test was conducted by screening against six pathogens comprising both Gram-positive and Gram-negative bacteria obtained from pharmaceutical microbiology laboratory stock. The extract was screened against 24 hour broth culture of bacteria seeded in the nutrient agar at concentrations 400, 200, 100, 50, 25, 12.5, 6.25 and 3.125 mg/ml in DMSO and incubated at 37oC, for 24 hours and measuring the inhibition zone diameter - IZD. -

Original Research Article Mid and Submontane Altitude Forests Communities on the West Hillside of Mount Bambouto (Cameroon)
1 Original Research Article 2 3 Mid and submontane altitude forests 4 communities on the West hillside of mount 5 Bambouto (Cameroon): Floristic originality and 6 comparisons ASTRACT Background and aims - Situated on the oceanic part of the Cameroon mountainous chain, the Western flank of Bambouto Mountains include the Atlantic biafran forests rich in endemic species but not well known. The objective of this work is to compare specific diversity, floristic composition and structure of two forests on this hillside. Methods - The inventories have been carried out in 18 plots of 20 m x 250 m plot established to cover all corners and centers of each forest in order to collect as many species as possible; also depending on the size of the forest block, vegetation physiognomy and altitude. Therefore, on a total area of nine hectares, all individuals with diameter at breast height ≥10 cm (dbh =1.30 m above ground) were counted. Phytodiversity has been assessed based on the usual diversity indices; these are the Shannon, Equitability and Simpson indices. The chi-square and Anova test were used to compare the data obtained. Keys results - With 168 species recorded in four hectares, the submontane forest noticeably appears richer than that of low and mid altitude (161 species in 5 hectares). Among these species, 46 are common to the two forests. The mean stands density with diameter at breast height (dbh) ≥ 10 cm recorded per hectare is 855 ± 32,7 at low and mid altitude forest and 1182 ± 38,4 at submontane forest. The diversity index, specific richness and the endemism rate values are comparable to those registered in other Central African sites. -

Floristic Diversity Across the Cameroon Mountains: the Case of Bakossi National Park and Mt Nlonako
Floristic Diversity across the Cameroon Mountains: The Case of Bakossi National Park and Mt Nlonako i Floristic Diversity across the Cameroon Mountains The case of Bakossi National Park and Mt Nlonako Technical Report Prepared and Submitted to the Rufford Small Grant Foundation, UK By Sainge Nsanyi Moses, Ngoh Michael Lyonga and Benedicta Jailuhge Tropical Plant Exploration Group (TroPEG) Cameroon June 2018 ii To cite this work: Sainge, MN., Lyonga, NM., Jailuhge B., (2018) Floristic Diversity across the Cameroon Mountains: The case of Bakossi National Park, and Mt Nlonako. Technical Report to the Rufford Small Grant Foundation UK, by Tropical Plant Exploration Group (TroPEG) Cameroon Authors: Sainge, MN., Lyonga NM., and Jailuhge B., Title: Floristic Diversity across the Cameroon Mountains: The case of Bakossi National Park, and Mt Nlonako. Tropical Plant Exploration Group (TroPEG) Cameroon P.O. Box 18 Mundemba, Ndian division, Southwest Region [email protected]; [email protected], Tel: (+237) 677513599 iii Acknowledgement We must comment that this is the fourth grant awarded as grant number 19476-D (being the second booster RSG ) which Tropical Plant Exploration Group (TroPEG) Cameroon has received from the Rufford Small Grant (RSG) Foundation UK. We are sincerely grateful and wish to express our deep hearted thanks for the immensed support since 2011. Our sincere appreciation also goes to the Government of Cameroon through the Ministry of Scientific Research and Innovation (MINRESI) and the Ministry of Forestry and Wildlife (MINFOF) for granting authorization to carry out this work. Special gratitute goes to Dr. Mabel Nechia Wantim of the University of Buea for her contribution in developing the maps. -

Smithsonian Libraries Baird Society Resident Scholar Program Project 2015
SMITHSONIAN LIBRARIES BAIRD SOCIETY RESIDENT SCHOLAR PROGRAM PROJECT 2015 National Museum of American History Tuesday Colloquium April 28, 2015 – 4 PM – East Conference Room, NMAH 4609 From corridors of knowledge to utopian highways in Africa: the explorer’s prelude to Western expansionism (ca.1800-1885) By Jan Vandersmissen Baird Fellow of the Smithsonian Institution Chargé de recherches du F.R.S.-FNRS Directeur au Centre d’Histoire des Sciences et des Techniques Université de Liège / Centre d’Histoire des Sciences et des Techniques 17 place Delcour, 4020 Liège (Belgium) / [email protected] It happened one Friday afternoon in March, in the reading room of the Joseph Cullman 3rd Library of Natural History. I was getting ready to terminate a week of intense investigation. But before storing my laptop, I asked permission to consult a final item. Daria Wingreen Mason, who in the past few weeks, together with Curator Leslie K. Overstreet, had made me acquainted with Smithsonian’s treasure house of natural history rare books, came out from the vault carrying a luxurious folio, which she placed on a lectern positioned in front of me. Having settled the paper work, she left me alone with a delicate work of art and science. In the tranquility of the reading room I opened the pages of Flore d’Oware en de Bénin, en Afrique. This book contains a fascinating study of the flora discovered in the late 1780s by the Frenchman Ambrose-Marie-Joseph Palisot de Beauvois (1752-1820) in a region situated near the delta of the Niger – which is in itself remarkable, taking into account the fact that European explorers had not yet determined the location of the swamps where the waters of that mighty stream mingle with those of the Atlantic Ocean. -

Out of Africa: Mysteries of Access and Benefit Sharing
Out of Africa: Mysteries of Access and Benefit Sharing a report by Jay McGown edited and introduced by Beth Burrows Edmonds Institute in cooperation with African Centre for Biosafety 2006 Material in this report may be freely quoted and reproduced, provided the material is quoted in its entirety and appropriate credit is given to the author, the editor, and the publishers. Out of Africa: Mysteries of Access and Benefit Sharing was published by The Edmonds Institute 20319-92nd Avenue West Edmonds, Washington 98020 USA Telephone: 001-425-775-5383 E-mail: [email protected] Website: www.edmonds-institute.org in cooperation with The African Centre for Biosafety Suite 3, 12 Clamart Road Richmond, South Africa 2092 Telephone: 27 11 646 0699 E-mail: [email protected] Website www.biosafetyafrica.net Under grants from: C.S. Fund and the Funding Exchange With graphics support from: Jay McGown ISBN 1-930169-49-3 Out of Africa: Mysteries of Access and Benefit Sharing TABLE OF CONTENTS Page INTRODUCTION i MEDICINE FROM BIODIVERSITY 1 OUT OF Diabetes Drug Produced by a Microbe Kenya 1 A Treatment for Diabetes Libya, Egypt 2 Antibiotics from a Termite Hill Gambia 3 An Antifungal from a Giraffe Namibia 3 Infection-fighting Amoeba Mauritius 4 A Treatment for Impotence Congo (Brazzaville) 5 Vaccines from Microbes Egypt 6 Four Multipurpose Medicinal Plants Ethiopia and neighboring 7 countries Hoodia, the Appetite Suppressant Namibia, South Africa, 8 Angola, Botswana Antibiotics from Giant Land Snails West Africa, from Sierra Leone 10 to Nigeria Drug Addiction Treatment from Iboga Central and West Africa 10 Multipurpose Kombo Butter Central and West Africa 12 COSMETICS FROM BIODIVERSITY 13 OUT OF Skin Whitener from an Aloe South Africa and Lesotho 13 Beauty and Healing from Okoumé Resin Gabon and Western Central Africa 14 Skin and Hair Care from the Argan Tree Morocco 16 Skin Care Plus from “Pharaoh’s Wheat” Egypt? 17 Skin Care, Etc. -

Chemical Composition, Pharmacological and Zootechnical Usefulness of Napoleonaea Vogelii Hook & Planch
American Journal of Plant Sciences, 2021, 12, 1288-1303 https://www.scirp.org/journal/ajps ISSN Online: 2158-2750 ISSN Print: 2158-2742 Zootechnical, Pharmacological Uses and Chemical Composition of Napoleonaea vogelii Hook & Planch (Lecythidaceae) in West Africa —A Review Pascal Abiodoun Olounladé1*, Christian Cocou Dansou1, Oriane Songbé1, Kisito Babatoundé Arigbo1, Tchégniho Géraldo Houménou1, André Boha Aboh1, Sylvie Mawulé Hounzangbé-Adoté2, Latifou Lagnika3 1Zootechnical Research and Livestock System Unit, Laboratory of Animal and Fisheries Science (LaSAH), National University of Agriculture (UNA), Porto-Novo, Benin 2Laboratory of Ethnopharmacology and Animal Health, Faculty of Agronomic Sciences, University of Abomey-Calavi, Cotonou, Benin 3Laboratory of Biochemistry and Bioactive Natural Substances, Faculty of Science and Technology, University of Abomey-Calavi, Cotonou, Benin How to cite this paper: Olounladé, P.A., Abstract Dansou, C.C., Songbé, O., Arigbo, K.B., Houménou, T.G., Aboh, A.B., Hounzangbé- Napoleonaea vogelii, Lecythidaceae family is a tropical evergreen shrub Adoté, S.M. and Lagnika, L. (2021) Zoo- widely distributed in the coastal regions of West African countries including technical, Pharmacological Uses and Chemi- Benin. It is a medicinal plant whose leaves and bark are of great utility in tra- cal Composition of Napoleonaea vogelii ditional medicine. Despite its importance, it is little used in ethnoveterinary Hook & Planch (Lecythidaceae) in West Africa. American Journal of Plant Sciences, medicine and its pharmacological basis in this field and especially in the 12, 1288-1303. treatment of parasitic diseases caused by Haemonchus contortus is very little https://doi.org/10.4236/ajps.2021.128090 documented. This review aims to synthesise existing data on the chemical composition, pharmacological and zootechnical usefulness of N. -

List of Plant Species Identified in the Northern Part of the Lope Reserve, Gabon*
TROPICS 3 (3/4): 249-276 Issued March, 1994 List of Plant Species Identified in the Northern Part of the Lope Reserve, Gabon* Caroline E.G. TUTIN Centre International de Recherche Medicales de Franceville, Franceville, Gabon; Department of Biological and Molecular Sciences, University of Stirling, Scotland. Lee J. T. WHITE NYZS-The Wildlife Conservation Society, U.S.A.; Institute of Cell, Animal and Population Biology, University of Edinburgh, Scotland; Programme de Conservation et Utilisation Rationelle des Ecosystemes Forestiers d'Afrique Centrale (ECOFAC), Composante Gabon (Projet FED, CCE DG VIII). Elizabeth A. WILLIAMSON Psychology Department, University of Stirling, Scotland. Michel FERNANDEZ Centre International de Recherche Medicales de Franceville, Franceville, Gabon; Department of Biological and Molecular Sciences, University of Stirling, Scotland; Programme de Conservation et Utilisation Rationelle des Ecosystemes Forestiers d' Afrique Centrale (ECOFAC), Composante Gabon (Projet FED, CCE DG VIII). Gordon MCPHERSON Missouri Botanical Garden, St. Louis, Missouri, U.S.A. ABSTRACT Research on lowland gorillas (Gorilla g. gorilla) and chimpanzees (Pan t. troglodytes) began at the 'Station d'Etudes des Gorilles et Chimpanzes' in the Lope Reserve, central Gabon, in 1983 and is on-going. This paper lists 676 species of plants belonging to 91 families that occur in the 50 sq. km study area. Data on trees with diameters of 10 cm or more were collected systematically along line transects and opportunistic collections of fertile plants were made. For each plant species, the life-form, habitat preference and density (for trees recorded on transects) are listed. For plants that provide food for gorillas and chimpanzees, the part eaten is given. -

Traditional Sources of Mosquito Repellents in Southeast Nigeria
Traditional mosquito control JBiopest 5(1): 1 - 6 JBiopest 6(2):104-107 Traditional sources of mosquito repellents in southeast Nigeria Nsirim L. Edwin-Wosu, Samuel N. Okiwelu and M. Aline E. Noutcha ABSTRACT Information was obtained over two-years, in randomly-selected villages across six states viz., Abia, Akwa Ibom, Bayelsa, Cross River, Enugu and Rivers in southeast Nigeria, from key informants (herbalists) on plant species used as repellents against malaria vectors. Twenty-four species in 16 families were identified. The Verbenaceae yielded 5 species, the Meliaceae 3 species and the Malvaceae and Labiatae 2 species each. Duranta repens, Duranta plumeri (Verbenaceae) and Ocimum gratissimum (Labiatae) were the most widely used. Sida acuta (Malvaceae) was used in four states. The data were compared to plant species used in other countries across the globe as mosquito repellents; this showed that southeast Nigeria has a potential array of plant species that may be sources of plant-based malaria vector repellents. MS History: 15.9.2013 (Received)-11.11.2013 (Revised)-16.12.2013 (Accepted) Key words: Verbnaceae, Duranta spp., Ocimum gratissimum, repellents, malaria vectors. INTRODUCTION the degree of protection against biting mosquitoes or It is estimated that about 1 million deaths (range, persistence on human skin afforded by DEET 744,000-13,000,000) from the direct effects of (Peterson and Coats, 2001). Concerns with the malaria occur annually in Africa, more than 75% of safety of DEET, especially in children have resulted them are often children (Snow et al., 2001). There in the search for natural alternatives (Isman, 2006). are two main strategies for malaria management: malaria prevention (vector control, prophylaxis and Scientific literature in the past 3 decades describes potential use of vaccines) and treatment (drugs and many isolated plant secondary metabolites that blood transfusions, among others). -

Recircumscription of the Lecythidaceae
TAXON 47 - NOVEMBER 1998 817 Recircumscription of the Lecythidaceae Cynthia M. Morton'", Ghillean T. Prance', Scott A. Mori4 & Lucy G. Thorburn' Summary Morton. C. M.• Prance, G. T., Mori, S. A. & Thorburn. L. G.: Recircumscriplion of the Le cythidaceae. Taxon 47: 817-827. 1998. -ISSN 004Q-0262. The phylogenetic relationships of the genera of Lecythidaceae and representatives of Scyto petalaceae were assessed using cladistic analysis of both molecular (rbcL and trnL se quences) and morphological data. The results show that the pantropical family Lecythida ceae is paraphyletic. Support was found for the monophyly of three of the four subfamilies: Lecythidoideae, Planchonioideae, and Foetidioideae. The fourth subfamily, Napoleonaeol deae, was found to be paraphyletic, with members of the Scytopetalaceae being nested within it forming a strong clade with Asteranthos. Both families share a number of mor phological features, including several distinct characters such as cortical bundles in the stem. The combined analysis produced three trees of 471 steps and consistency index Cl = 0.71 and retention index Rl = 0.70. Asteranthos !'P.~, members of Scytopetalaceae should be treated as a subfamily of Lecythidaceae, while Napoleonaea and Crateranthus (the latter based solely on morphological features) should remain in the subfamily Napoleo naeoideae.The Lecythldaceaeare recircumscribed, and Asteranthosand members of Scyto peta/aceae are included in Scytopetaloideae. A formal·llWJ!J-pmic synopsis accommodating this new circumscription is presented. Introduction The Lecythidaceae Poit, are 8 pantropical family of trees and shrubs consisting of . 20 genera split into four subfamilies in contemporary classifications (Cronquist, 1981; Prance & Mori, 1979; Takhtajan, 1987; ~ri & Prance, 1990; Thome, 1992).