IFMSA Policy Document Disaster and Emergency Management
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Adversus Paganos: Disaster, Dragons, and Episcopal Authority in Gregory of Tours
Adversus paganos: Disaster, Dragons, and Episcopal Authority in Gregory of Tours David J. Patterson Comitatus: A Journal of Medieval and Renaissance Studies, Volume 44, 2013, pp. 1-28 (Article) Published by Center for Medieval and Renaissance Studies, UCLA DOI: 10.1353/cjm.2013.0000 For additional information about this article http://muse.jhu.edu/journals/cjm/summary/v044/44.patterson.html Access provided by University of British Columbia Library (29 Aug 2013 02:49 GMT) ADVERSUS PAGANOS: DISASTER, DRAGONS, AND EPISCOPAL AUTHORITY IN GREGORY OF TOURS David J. Patterson* Abstract: In 589 a great flood of the Tiber sent a torrent of water rushing through Rome. According to Gregory of Tours, the floodwaters carried some remarkable detritus: several dying serpents and, perhaps most strikingly, the corpse of a dragon. The flooding was soon followed by plague and the death of a pope. This remarkable chain of events leaves us with puzzling questions: What significance would Gregory have located in such a narrative? For a modern reader, the account (apart from its dragon) reads like a descrip- tion of a natural disaster. Yet how did people in the early Middle Ages themselves per- ceive such events? This article argues that, in making sense of the disasters at Rome in 589, Gregory revealed something of his historical consciousness: drawing on both bibli- cal imagery and pagan historiography, Gregory struggled to identify appropriate objects of both blame and succor in the wake of calamity. Keywords: plague, natural disaster, Gregory of Tours, Gregory the Great, Asclepius, pagan survivals, dragon, serpent, sixth century, Rome. In 589, a great flood of the Tiber River sent a torrent of water rushing through the city of Rome. -

Exposure and Vulnerability
Determinants of Risk: 2 Exposure and Vulnerability Coordinating Lead Authors: Omar-Dario Cardona (Colombia), Maarten K. van Aalst (Netherlands) Lead Authors: Jörn Birkmann (Germany), Maureen Fordham (UK), Glenn McGregor (New Zealand), Rosa Perez (Philippines), Roger S. Pulwarty (USA), E. Lisa F. Schipper (Sweden), Bach Tan Sinh (Vietnam) Review Editors: Henri Décamps (France), Mark Keim (USA) Contributing Authors: Ian Davis (UK), Kristie L. Ebi (USA), Allan Lavell (Costa Rica), Reinhard Mechler (Germany), Virginia Murray (UK), Mark Pelling (UK), Jürgen Pohl (Germany), Anthony-Oliver Smith (USA), Frank Thomalla (Australia) This chapter should be cited as: Cardona, O.D., M.K. van Aalst, J. Birkmann, M. Fordham, G. McGregor, R. Perez, R.S. Pulwarty, E.L.F. Schipper, and B.T. Sinh, 2012: Determinants of risk: exposure and vulnerability. In: Managing the Risks of Extreme Events and Disasters to Advance Climate Change Adaptation [Field, C.B., V. Barros, T.F. Stocker, D. Qin, D.J. Dokken, K.L. Ebi, M.D. Mastrandrea, K.J. Mach, G.-K. Plattner, S.K. Allen, M. Tignor, and P.M. Midgley (eds.)]. A Special Report of Working Groups I and II of the Intergovernmental Panel on Climate Change (IPCC). Cambridge University Press, Cambridge, UK, and New York, NY, USA, pp. 65-108. 65 Determinants of Risk: Exposure and Vulnerability Chapter 2 Table of Contents Executive Summary ...................................................................................................................................67 2.1. Introduction and Scope..............................................................................................................69 -
Psychological Issues in Escape, Rescue, and Survival in the Wake of Disaster
2008 Psychological Issues in Escape, Rescue, and Survival in the Wake of Disaster Report Submitted to the National Institute of Occupational Safety and Health, Pittsburgh Research Laboratory George S. Everly, Jr., PhD, ABPP Paul Perrin & George S. Everly, III Contents INTRODUCTION THE PSYCHOLOGICAL IMPACT OF CRISIS AND DISASTERS The Nature of Human Stress Physiology of Stress Psychology of Stress Excessive Stress Distress Depression Posttraumatic Stress Disorder (PTSD) Compassion Fatigue A Review of Empirical Investigations on the Mental Health Consequences of Crisis and Disaster Primary Victims/ Survivors Rescue and Recovery Personnel “RESISTANCE, RESILIENCE, AND RECOVERY” AS A STRATEGIC AND INTEGRATIVE INTERVENTION PARADIGM Historical Foundations Resistance, Resiliency, Recovery: A Continuum of Care Building Resistance Self‐efficacy Hardiness Enhancing Resilience Fostering Recovery LEADERSHIP AND THE INCIDENT MANAGEMENT AND INCIDENT COMMAND SYSTEMS (ICS) Leadership: What is it? Leadership Resides in Those Who Follow Incident Management Essential Information NIMS Components 1 Psychological Issues in Escape, Rescue, and Survival in the Wake of Disaster | George Everly, Jr. The Need for Incident Management Key Features of the ICS Placement of Psychological Crisis Intervention Teams in ICS Functional Areas in the Incident Command System Structuring the Mental Health Response Challenges of Rural and Isolated Response Caution: Fatigue in Incident Response Summary CONCLUSIONS AND RECOMMENDATIONS REFERENCES APPENDIX A – Training resources in disaster mental health and crisis intervention APPENDIX B – Psychological First Aid (PFA) 2 Psychological Issues in Escape, Rescue, and Survival in the Wake of Disaster | George Everly, Jr. Introduction The experience of disaster appears to have become an expected aspect of life. Whether it is a natural disaster such as a hurricane or tsunami, or a human‐made disaster such as terrorism, the effects can be both physically and psychological devastating. -
DISASTER MANAGEMENT in a PANDEMIC 1 STEPS to FOLLOW for an EFFECTIVE How to Create an Emergency Operations Center (EOC) PANDEMIC RESPONSE 1
DISASTER MANAGEMENT TOOL DISASTER MANAGEMENT 15 IN A PANDEMIC In any serious disaster a gap develops between resource needs and resource availability. In a severe pandemic this gap will be much worse due to global supply chain disruptions or delays and the fact that governments and aid organizations PREPAREDNESS RESPONSE will be overwhelmed responding to all who need assistance at the same time. Your This tool will help you to: plan should assume that there will be little or no assistance coming from outside • Develop an organizational the municipality. structure to manage a pandemic It is of prime importance that the municipal leaders read, discuss, and study their at a municipal level national, regional/state, and district pandemic response plans to understand: • Assess needs, identify resources, • What plans are already in place plan, and implement the • What preparedness and response resources are available municipality’s response to a pandemic • How the municipal level plan fits into the national pandemic response structure Who will implement this tool: As municipal leaders, you will be responsible for keeping the population healthy, calm, and safe during the 6 to 12 weeks of each severe pandemic wave (remember • The municipal leadership team there could be as many as three waves). Your actions can determine whether there • Individuals responsible are many deaths or relatively few. for disaster response and implementation The most important goals of successful municipal pandemic management are to: What Needs to Be Done? • Have a strong enough organizational structure to manage a pandemic in the municipality No one will be able to prevent a • Continually assess needs, identify resources, plan the response, and severe pandemic from coming to implement the plan your municipality. -

Natural Disaster Emergency Planning and Preparedness Risk Bulletin
Natural disaster emergency planning and preparedness An Environmental Risk Toolkit AXA XL Environmental Risk Bulletin Be prepared. Natural Disaster Emergency Planning and Preparedness . 1 Disasters can happen at any time. Imagine that your business or facility is hit by a natural disaster, such as a hurricane, tornado, flood, earthquake or large wildfire. How will you ensure that your business quickly returns to normal operations and profitability? How will you protect your employees? One way to help do this is to create a Natural Disaster Preparedness and Response Plan. Both the final plan and the planning process are useful tools to respond to emergencies and to minimize costs and business interruptions. It can also be a strategic tool in business planning to ensure operational continuity. Being prepared and having a written plan should also help companies more effectively respond to any third party liabilities and claims that may arise from the surrounding community in the aftermath of a disaster. Why Plan for Natural Disasters? But why should we plan since natural disasters are rare? One of the primary reasons is potential cost savings to the affected business. Preparedness saves time and money by allowing a faster and more efficient resumption of routine business activities. Preparedness and periodic planning help businesses return to normal operation after a man-made or natural disaster. A disaster plan may also help enable a firm to stay in business and survive catastrophic events. According to the U.S. Federal Emergency Management Agency (FEMA), small businesses that don’t have a plan in place generally don’t survive after a disaster. -

The Institutional Causes of China's Great Famine, 1959–1961
Review of Economic Studies (2015) 82, 1568–1611 doi:10.1093/restud/rdv016 © The Author 2015. Published by Oxford University Press on behalf of The Review of Economic Studies Limited. Advance access publication 20 April 2015 The Institutional Causes of China’s Great Famine, 1959–1961 Downloaded from XIN MENG Australian National University NANCY QIAN Yale University http://restud.oxfordjournals.org/ and PIERRE YARED Columbia University First version received January 2012; final version accepted January 2015 (Eds.) This article studies the causes of China’s Great Famine, during which 16.5 to 45 million individuals at Columbia University Libraries on April 25, 2016 perished in rural areas. We document that average rural food retention during the famine was too high to generate a severe famine without rural inequality in food availability; that there was significant variance in famine mortality rates across rural regions; and that rural mortality rates were positively correlated with per capita food production, a surprising pattern that is unique to the famine years. We provide evidence that an inflexible and progressive government procurement policy (where procurement could not adjust to contemporaneous production and larger shares of expected production were procured from more productive regions) was necessary for generating this pattern and that this policy was a quantitatively important contributor to overall famine mortality. Key words: Famines, Modern chinese history, Institutions, Central planning JEL Codes: P2, O43, N45 1. INTRODUCTION -
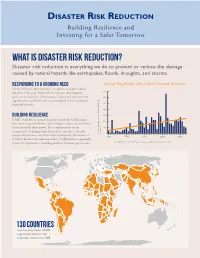
Disaster Risk Reduction Building Resilience and Investing for a Safer Tomorrow
DISASTER RISK REDUCTION Building Resilience and Investing for a Safer Tomorrow What is Disaster Risk Reduction? Disaster risk reduction is everything we do to prevent or reduce the damage caused by natural hazards like earthquakes, floods, droughts, and storms. Responding to a Growing Need Global Population Affected by Natural Disasters Natural disasters affect hundreds of millions of people around 700 the globe every year. With each new disaster, development gains are threatened as infrastructure is destroyed and economic 600 opportunities and livelihoods are interrupted or lost, leading to increased poverty. 500 400 Building Resilience 300 USAID responds to natural disasters around the world, saving 200 lives, protecting livelihoods, and working to reduce the economic losses caused by these events. Just as importantly, we are 100 committed to helping people lessen their exposure to hazards, Reported Number of People Affected Affected Reported Number of People (in Millions) 0 prepare for disasters, and better withstand shocks. The lessons of 1970 1980 1990 2000 2010 USAID’s disaster risk reduction efforts worldwide have repeatedly shown the importance of building resilience in hazard-prone areas. Source: EM-DAT - The OFDA/CRED International Disaster Database, www.emdat.be, April 2014 130 COUNTRIES have benefited from USAID- supported disaster risk reduction efforts since 1989. USAID’S DISASTER RISK REDUCTION PROGRAMS SAVE LIVES Strengthening Early Warning Since 1989, we have helped establish 17 global, regional, or national early warning systems for drought, volcanoes, cyclones, and floods. These early warning systems work. For example, in 2013, warnings issued days prior to Cyclone Phailin’s arrival in India gave local authorities time to coordinate preparedness measures, including the evacuation of 1 million people living in coastal areas. -

(COVID-19) Pandemic: an Opportunity for a Systemic Approach to Disaster Risk for the Caribbean
COVID-19 Report ECLAC-UNDRR March 2021 The coronavirus disease (COVID-19) pandemic: an opportunity for a systemic approach to disaster risk for the Caribbean Foreword by the Executive Secretary of the Economic Commission for Latin America and the Caribbean (ECLAC) The COVID-19 pandemic is a disaster that combines a biological threat with various vulnerabilities, such as the organizational and response Contents capacity of health systems, overcrowding, informality, social work Foreword by the Executive Secretary of the practices, and public transport. Disasters of this origin are not unknown Economic Commission for Latin America in Latin America and the Caribbean. Dengue and cholera have caused and the Caribbean (ECLAC) .................................1 the most epidemics in the region in the last fifty years. However, unlike other threats such as earthquakes, hurricanes and floods, which last Foreword by the Special Representative of the Secretary-General for Disaster for minutes, days, or weeks, an epidemic can last for years. In 2020, Risk Reduction .....................................................3 COVID-19 affected all the countries in the region. Introduction ...........................................................4 The human and economic impacts of the COVID-19 pandemic are unprecedented. According to World Health Organization (WHO) figures, I. Socioeconomic effects of COVID-19 by November 2020 it had caused more than 18 times more deaths than on the Caribbean .............................................5 all the epidemics that took place in Latin America and the Caribbean II. Towards a systemic approach to between 1970 and 2019. Furthermore, these deaths account for 63% of disaster risk in the Caribbean ......................14 all those caused by disasters in the region in the same period. -

Developing a Disaster Preparedness/ Emergency Response Plan
ALLIANCE REFERENCE GUIDE Developing a Disaster Preparedness/ Emergency Response Plan Preparing for disaster is one of the most important things a museum can do in order to safeguard its collections and protect staff and visitors from hazards. This guide provides a primer on disaster preparedness and helps museums understand the process of developing a disaster preparedness/emergency response plan. It reflects the standards of the field that all museums should adhere to and aligns with the requirements of the Alliance’s Core Documents Verification and Accreditation programs. What It Is A disaster preparedness/emergency response plan, or disaster plan, is a written policy accompanied by procedures that prevent harm in cases of emergency and minimize damage resulting from disasters (man-made or natural). All museums are expected to have a plan that addresses how it will protect its staff, visitors, and collections in case of emergency or disaster. The plan should be tailored to the museum’s specific circumstances and facilities and should cover all relevant threats and risks. Key components include emergency procedures, evacuation plans for staff and visitors, plans for how to protect or recover collections, and assignments of responsibility. Why It Is Important Museums care for resources in trust for the public and therefore must minimize risks to those resources. Having a strong disaster plan helps the museum safeguard its collections, buildings, staff, visitors, and community. It also has financial implications that include insurance and the conservation costs involved with salvage. Risk identification and management are a vital part of museum operations. Copyright American Alliance of Museums, 2018. -
Emergency Disaster Designation and Declaration Process Overview Agriculture-Related Disasters and Disaster Designations Are Quite Common
United States Department of Agriculture FARM SERVICE AGENCY DISASTER ASSISTANCE Emergency Disaster Designation and Declaration Process Overview Agriculture-related disasters and disaster designations are quite common. Many counties in the United States have been designated as disaster areas in the past several years, even in years of record crop production. The Secretary of Agriculture is authorized to designate counties as disaster areas to make emergency (EM) loans available to producers suffering losses in those counties and in counties that are contiguous to a designated county. In addition to EM loan eligibility, other emergency assistance programs, such as Farm Service Agency (FSA) disaster assistance programs, have historically used disaster designations as an eligibility trigger. Types of Disaster Designations What Does a Disaster Designation FSA administers four types of disaster designations: Specify? • U.S. Department of Agriculture (USDA) Secretarial disaster desig- A disaster designation specifies: nation; • Presidential major disaster and Presidential emergency declara- • The disaster that resulted in the desig- tion; nation; • FSA Administrator’s Physical Loss Notification (APLN); and • The incident period (dates) of that disas- • Quarantine designation by the Secretary under the Plant Protec- ter; and tion Act or animal quarantine laws. • The specific counties included in the designation. USDA Secretarial disaster designations must be requested of the Secretary of Agriculture by a governor or the governor’s authorized -

Preparing for Disaster for People with Disabilities and Other Special Needs Visit the Websites Listed Below to Obtain Additional Information
Preparing for Disaster for People with Disabilities and other Special Needs Visit the websites listed below to obtain additional information: www.access-board.gov The Access Board www.aoa.dhhs.gov DHHS Administration on Aging www.ncd.gov National Council on Disability www.nod.org/emergency National Organization on Disability www.prepare.org Prepare.org www.aapd.com American Association for People with Disabilities www.afb.org American Foundation for the Blind www.nad.org National Association of the Deaf www.lacity.org/DOD Los Angeles City Department on Disability www.easter-seals.org Easter Seals For more in-depth information, get a copy of "Disaster Preparedness for People with Disabilities" (A5091) from the American Red Cross, or visit www.redcross.org/services/disaster/beprepared/disability.pdf For the millions of Americans who have physical, medical, sensory or cognitive disabilities, emergencies such as fires, floods and acts of terrorism present a real challenge. The same challenge also applies to the elderly and other special needs populations. Protecting yourself and your family when disaster strikes requires planning ahead. This booklet will help you get started. Discuss these ideas with your family, friends and/or your personal care attendant, or anyone else in your support network and prepare an emergency plan. Post the plan where everyone will see it, keep a copy with you and make sure everyone involved in your plan has a copy. WHY PREPARE? Where will you, your family, your friends or personal care attendants be when an emergency or disaster strikes? You, and those you care about, could be anywhere – at home, work, school or in transit. -

ECHO Factsheet – Disaster Risk Reduction – October 2017
Disaster Risk Reduction ECHO FACTSHEET Facts & Figures shortage In 2016, 9% of the EU's humanitarian funding went to disaster risk reduction (DRR) activities, more than €175 million The EU is committed to strengthening resilience worldwide. Resilience is embedded into the majority of humanitarian and development actions. For example, more than 57% of all ECHO funded projects include DRR activities In 2016, EU funding for DRR activities reduced disaster Children in Nicaragua receive training on how to respond to a disaster. ©CRIC 2009 risks for approximately 24 Key messages million people worldwide Natural hazards such as earthquakes, floods, drought and cyclones cannot be Food, water and prevented but the number of lives they take and the damage they cause can be sanitation are the sectors greatly reduced thanks to preparation and protection measures. Disaster Risk where most ECHO funded Reduction (DRR) saves lives and strengthens the resilience of communities DRR activities are enabling them to anticipate, absorb, and bounce back from shocks. undertaken DRR programmes aim to protect lives and livelihoods. Communities are empowered to strengthen their capacities with simple measures such as training and community organising, establishing early warning systems and contingency plans, making shelters safe, and protecting livestock and assets from natural hazards. DRR is cost effective: on average, every euro spent of DRR activities saves between four and seven euros that would be spent to respond to the impact of disasters. European Civil Protection and Humanitarian Aid Operations In June 2016, the European Commission launched an action plan to implement the Sendai Framework and promote the integration of disaster risk reduction in B-1049 Brussels, Belgium EU policies.