Devriesea Agamarum in Lizards
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Reptiles of the Wet Tropics
Reptiles of the Wet Tropics The concentration of endemic reptiles in the Wet Tropics is greater than in any other area of Australia. About 162 species of reptiles live in this region and 24 of these species live exclusively in the rainforest. Eighteen of them are found nowhere else in the world. Many lizards are closely related to species in New Guinea and South-East Asia. The ancestors of two of the resident geckos are thought to date back millions of years to the ancient super continent of Gondwana. PRICKLY FOREST SKINK - Gnypetoscincus queenlandiae Length to 17cm. This skink is distinguished by its very prickly back scales. It is very hard to see, as it is nocturnal and hides under rotting logs and is extremely heat sensitive. Located in the rainforest in the Wet Tropics only, from near Cooktown to west of Cardwell. RAINFOREST SKINK - Eulamprus tigrinus Length to 16cm. The body has irregular, broken black bars. They give birth to live young and feed on invertebrates. Predominantly arboreal, they bask in patches of sunlight in the rainforest and shelter in tree hollows at night. Apparently capable of producing a sharp squeak when handled or when fighting. It is rare and found only in rainforests from south of Cooktown to west of Cardwell. NORTHERN RED-THROATED SKINK - Carlia rubrigularis Length to 14cm. The sides of the neck are richly flushed with red in breeding males. Lays 1-2 eggs per clutch, sometimes communally. Forages for insects in leaf litter, fallen logs and tree buttresses. May also prey on small skinks and own species. -
Printable PDF Format
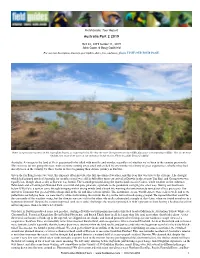
Field Guides Tour Report Australia Part 2 2019 Oct 22, 2019 to Nov 11, 2019 John Coons & Doug Gochfeld For our tour description, itinerary, past triplists, dates, fees, and more, please VISIT OUR TOUR PAGE. Water is a precious resource in the Australian deserts, so watering holes like this one near Georgetown are incredible places for concentrating wildlife. Two of our most bird diverse excursions were on our mornings in this region. Photo by guide Doug Gochfeld. Australia. A voyage to the land of Oz is guaranteed to be filled with novelty and wonder, regardless of whether we’ve been to the country previously. This was true for our group this year, with everyone coming away awed and excited by any number of a litany of great experiences, whether they had already been in the country for three weeks or were beginning their Aussie journey in Darwin. Given the far-flung locales we visit, this itinerary often provides the full spectrum of weather, and this year that was true to the extreme. The drought which had gripped much of Australia for months on end was still in full effect upon our arrival at Darwin in the steamy Top End, and Georgetown was equally hot, though about as dry as Darwin was humid. The warmth persisted along the Queensland coast in Cairns, while weather on the Atherton Tablelands and at Lamington National Park was mild and quite pleasant, a prelude to the pendulum swinging the other way. During our final hours below O’Reilly’s, a system came through bringing with it strong winds (and a brush fire warning that unfortunately turned out all too prescient). -

Body-Size Effect on Egg Size in Eublepharid Geckos (Squamata
Blackwell Publishing LtdOxford, UKBIJBiological Journal of the Linnean Society0024-4066The Linnean Society of London, 20062006 884 527532 Original Article EGG-SIZE ALLOMETRY IN EUBLEPHARID GECKOS L. KRATOCHVÍL and D. FRYNTA Biological Journal of the Linnean Society, 2006, 88, 527–532. With 2 figures Body-size effect on egg size in eublepharid geckos (Squamata: Eublepharidae), lizards with invariant clutch size: negative allometry for egg size in ectotherms is not universal LUKÁT KRATOCHVÍL1* and DANIEL FRYNTA2 1Department of Ecology, Charles University, Vinidná 7, CZ-128 44 Praha 2, the Czech Republic 2Department of Zoology, Charles University, Vinidná 7, CZ-128 44 Praha 2, the Czech Republic Received 1 February 2005; accepted for publication 5 December 2005 Within a single clutch, smaller species of ectotherms generally lay a smaller number of relatively larger eggs than do larger species. Many hypotheses explaining both the interspecific negative allometry in egg size and egg size– number trade-off postulate the existence of an upper limit to the egg size of larger species. Specifically, in lizards, large eggs of large species could have too long a duration of incubation, or they could be too large to pass through the pelvic opening, which is presumably constrained mechanically in larger species. Alternatively, negative allometry could be a result of limits affecting eggs of smaller species. Under the latter concept, hatchling size in smaller species may be close to the lower limit imposed by ecological interactions or physiological processes, and therefore smaller species have to invest in relatively larger offspring. Contrary to these lower limit hypotheses, explanations based on the existence of an upper limit always predict negative egg-size allometry even in animals with invariant clutch size, in which naturally there is no egg size–number trade-off. -

Literature Cited in Lizards Natural History Database
Literature Cited in Lizards Natural History database Abdala, C. S., A. S. Quinteros, and R. E. Espinoza. 2008. Two new species of Liolaemus (Iguania: Liolaemidae) from the puna of northwestern Argentina. Herpetologica 64:458-471. Abdala, C. S., D. Baldo, R. A. Juárez, and R. E. Espinoza. 2016. The first parthenogenetic pleurodont Iguanian: a new all-female Liolaemus (Squamata: Liolaemidae) from western Argentina. Copeia 104:487-497. Abdala, C. S., J. C. Acosta, M. R. Cabrera, H. J. Villaviciencio, and J. Marinero. 2009. A new Andean Liolaemus of the L. montanus series (Squamata: Iguania: Liolaemidae) from western Argentina. South American Journal of Herpetology 4:91-102. Abdala, C. S., J. L. Acosta, J. C. Acosta, B. B. Alvarez, F. Arias, L. J. Avila, . S. M. Zalba. 2012. Categorización del estado de conservación de las lagartijas y anfisbenas de la República Argentina. Cuadernos de Herpetologia 26 (Suppl. 1):215-248. Abell, A. J. 1999. Male-female spacing patterns in the lizard, Sceloporus virgatus. Amphibia-Reptilia 20:185-194. Abts, M. L. 1987. Environment and variation in life history traits of the Chuckwalla, Sauromalus obesus. Ecological Monographs 57:215-232. Achaval, F., and A. Olmos. 2003. Anfibios y reptiles del Uruguay. Montevideo, Uruguay: Facultad de Ciencias. Achaval, F., and A. Olmos. 2007. Anfibio y reptiles del Uruguay, 3rd edn. Montevideo, Uruguay: Serie Fauna 1. Ackermann, T. 2006. Schreibers Glatkopfleguan Leiocephalus schreibersii. Munich, Germany: Natur und Tier. Ackley, J. W., P. J. Muelleman, R. E. Carter, R. W. Henderson, and R. Powell. 2009. A rapid assessment of herpetofaunal diversity in variously altered habitats on Dominica. -

Global Patterns of Body Size Evolution in Squamate Reptiles Are Not Driven by Climate
This is a repository copy of Global patterns of body size evolution in squamate reptiles are not driven by climate. White Rose Research Online URL for this paper: http://eprints.whiterose.ac.uk/158006/ Version: Accepted Version Article: Slavenko, A. orcid.org/0000-0002-3265-7715, Feldman, A., Allison, A. et al. (17 more authors) (2019) Global patterns of body size evolution in squamate reptiles are not driven by climate. Global Ecology and Biogeography, 28 (4). pp. 471-483. ISSN 1466-822X https://doi.org/10.1111/geb.12868 This is the peer reviewed version of the following article: Slavenko, A, Feldman, A, Allison, A, et al. Global patterns of body size evolution in squamate reptiles are not driven by climate. Global Ecol Biogeogr. 2019; 28: 471– 483, which has been published in final form at https://doi.org/10.1111/geb.12868. This article may be used for non-commercial purposes in accordance with Wiley Terms and Conditions for Use of Self-Archived Versions. Reuse Items deposited in White Rose Research Online are protected by copyright, with all rights reserved unless indicated otherwise. They may be downloaded and/or printed for private study, or other acts as permitted by national copyright laws. The publisher or other rights holders may allow further reproduction and re-use of the full text version. This is indicated by the licence information on the White Rose Research Online record for the item. Takedown If you consider content in White Rose Research Online to be in breach of UK law, please notify us by emailing [email protected] including the URL of the record and the reason for the withdrawal request. -

Molecular Phylogenetics and Evolution 55 (2010) 153–167
Molecular Phylogenetics and Evolution 55 (2010) 153–167 Contents lists available at ScienceDirect Molecular Phylogenetics and Evolution journal homepage: www.elsevier.com/locate/ympev Conservation phylogenetics of helodermatid lizards using multiple molecular markers and a supertree approach Michael E. Douglas a,*, Marlis R. Douglas a, Gordon W. Schuett b, Daniel D. Beck c, Brian K. Sullivan d a Illinois Natural History Survey, Institute for Natural Resource Sustainability, University of Illinois, Champaign, IL 61820, USA b Department of Biology and Center for Behavioral Neuroscience, Georgia State University, Atlanta, GA 30303-3088, USA c Department of Biological Sciences, Central Washington University, Ellensburg, WA 98926, USA d Division of Mathematics & Natural Sciences, Arizona State University, Phoenix, AZ 85069, USA article info abstract Article history: We analyzed both mitochondrial (MT-) and nuclear (N) DNAs in a conservation phylogenetic framework to Received 30 June 2009 examine deep and shallow histories of the Beaded Lizard (Heloderma horridum) and Gila Monster (H. Revised 6 December 2009 suspectum) throughout their geographic ranges in North and Central America. Both MTDNA and intron Accepted 7 December 2009 markers clearly partitioned each species. One intron and MTDNA further subdivided H. horridum into its Available online 16 December 2009 four recognized subspecies (H. n. alvarezi, charlesbogerti, exasperatum, and horridum). However, the two subspecies of H. suspectum (H. s. suspectum and H. s. cinctum) were undefined. A supertree approach sus- Keywords: tained these relationships. Overall, the Helodermatidae is reaffirmed as an ancient and conserved group. Anguimorpha Its most recent common ancestor (MRCA) was Lower Eocene [35.4 million years ago (mya)], with a 25 ATPase Enolase my period of stasis before the MRCA of H. -

Lizards & Snakes: Alive!
LIZARDSLIZARDS && SNAKES:SNAKES: ALIVE!ALIVE! EDUCATOR’SEDUCATOR’S GUIDEGUIDE www.sdnhm.org/exhibits/lizardsandsnakeswww.sdnhm.org/exhibits/lizardsandsnakes Inside: • Suggestions to Help You Come Prepared • Must-Read Key Concepts and Background Information • Strategies for Teaching in the Exhibition • Activities to Extend Learning Back in the Classroom • Map of the Exhibition to Guide Your Visit • Correlations to California State Standards Special thanks to the Ellen Browning Scripps Foundation and the Nordson Corporation Foundation for providing underwriting support of the Teacher’s Guide KEYKEY CONCEPTSCONCEPTS Squamates—legged and legless lizards, including snakes—are among the most successful vertebrates on Earth. Found everywhere but the coldest and highest places on the planet, 8,000 species make squamates more diverse than mammals. Remarkable adaptations in behavior, shape, movement, and feeding contribute to the success of this huge and ancient group. BEHAVIOR Over 45O species of snakes (yet only two species of lizards) An animal’s ability to sense and respond to its environment is are considered to be dangerously venomous. Snake venom is a crucial for survival. Some squamates, like iguanas, rely heavily poisonous “soup” of enzymes with harmful effects—including on vision to locate food, and use their pliable tongues to grab nervous system failure and tissue damage—that subdue prey. it. Other squamates, like snakes, evolved effective chemore- The venom also begins to break down the prey from the inside ception and use their smooth hard tongues to transfer before the snake starts to eat it. Venom is delivered through a molecular clues from the environment to sensory organs in wide array of teeth. -

Scaling Up: the Contemporary Reptile Pet Market in Japan
S H O R T R E P O R T SCALING UP: THE CONTEMPORARY REPTILE PET MARKET IN JAPAN CHINESE WATER DRAGON / © J. JANSSEN J. © / DRAGON WATER CHINESE 64 TRAFFIC Bulletin 9RO1R SS H H O O R R T T R R E E P P O O R R T T 5HSRUWE\.HLNR:DNDR -RUGL-DQVVHQDQG 6HUHQH&KQJ TRAFFIC Bulletin9RO1R S H O R T R E P O R T ,ඇඍඋඈൽඎർඍංඈඇ 0ൾඍඁඈൽඌ he reptile pet industry has been scrutinised by • Market survey the international conservation community for In order to investigate the reptiles for sale in pet shops its role in the trade of a wide range of species, and expos in Japan, TRAFFIC investigators carried many of which are threatened by collection out surveys of eight outlets in Tokyo, six in Kanagawa for trade (Herrel and van der Meijden, 2014; Prefecture, and two in Osaka Prefecture in February TAuliya et al., ,QWHUPVRIPRQHWDU\YDOXH-DSDQ 2017. The Reptiles Fever—an exotic pet trade expo and was the fourth largest importer of live reptiles in 2016 the largest in the Kansai area, with about 40 trading stalls, &RPWUDGH ,QWKDW\HDU-DSDQLPSRUWHG was also surveyed. All reptile species were recorded to live reptiles and exported 8,702 live reptiles (Ministry of species or subspecies level where possible, as well as )LQDQFH 9LVLWRUVWRUHSWLOHH[SRVKDYHLQFUHDVHG information on the number of animals, price, origin, and over time, with over 20,000 people attending the Tokyo VRXUFH FDSWLYHEUHGRUZLOGFDXJKW ZKHUHSRVVLEOH1R Reptiles World 2016 Show, up from 8,343 in 2011 animals were purchased as part of the survey. -

Anolis Equestris) Should Be Removed When Face of a Watch
VOLUME 15, NUMBER 4 DECEMBER 2008 ONSERVATION AUANATURAL ISTORY AND USBANDRY OF EPTILES IC G, N H , H R International Reptile Conservation Foundation www.IRCF.org Central Netted Dragons (Ctenophorus nuchalis) from Australia are popular in captivity due to their striking appearance and great temperament. See article on p. 226. Known variously as Peters’ Forest Dragon, Doria’s Anglehead Lizard, or Abbott’s Anglehead Lizard (depending on subspecies), Gonocephalus doriae is known from southern Thailand, western Malaysia, and Indonesia west of Wallace’s Line SHANNON PLUMMER (a biogeographic division between islands associated with Asia and those with plants and animals more closely related to those on Australia). They live in remaining forested areas to elevations of 1,600 m (4,800 ft), where they spend most of their time high in trees near streams, either clinging to vertical trunks or sitting on the ends of thin branches. Their conservation status has not been assessed. MICHAEL KERN KENNETH L. KRYSKO KRISTA MOUGEY Newly hatched Texas Horned Lizard (Phrynosoma cornutum) on the Invasive Knight Anoles (Anolis equestris) should be removed when face of a watch. See article on p. 204. encountered in the wild. See article on p. 212. MARK DE SILVA Grenada Treeboas (Corallus grenadensis) remain abundant on many of the Grenadine Islands despite the fact that virtually all forested portions of the islands were cleared for agriculture during colonial times. This individual is from Mayreau. See article on p. 198. WIKIPEDIA.ORG JOSHUA M. KAPFER Of the snakes that occur in the upper midwestern United States, Populations of the Caspian Seal (Pusa caspica) have declined by 90% JOHN BINNS Bullsnakes (Pituophis catenifer sayi) are arguably the most impressive in in the last 100 years due to unsustainable hunting and habitat degra- Green Iguanas (Iguana iguana) are frequently edificarian on Grand Cayman. -

Describing Species
DESCRIBING SPECIES Practical Taxonomic Procedure for Biologists Judith E. Winston COLUMBIA UNIVERSITY PRESS NEW YORK Columbia University Press Publishers Since 1893 New York Chichester, West Sussex Copyright © 1999 Columbia University Press All rights reserved Library of Congress Cataloging-in-Publication Data © Winston, Judith E. Describing species : practical taxonomic procedure for biologists / Judith E. Winston, p. cm. Includes bibliographical references and index. ISBN 0-231-06824-7 (alk. paper)—0-231-06825-5 (pbk.: alk. paper) 1. Biology—Classification. 2. Species. I. Title. QH83.W57 1999 570'.1'2—dc21 99-14019 Casebound editions of Columbia University Press books are printed on permanent and durable acid-free paper. Printed in the United States of America c 10 98765432 p 10 98765432 The Far Side by Gary Larson "I'm one of those species they describe as 'awkward on land." Gary Larson cartoon celebrates species description, an important and still unfinished aspect of taxonomy. THE FAR SIDE © 1988 FARWORKS, INC. Used by permission. All rights reserved. Universal Press Syndicate DESCRIBING SPECIES For my daughter, Eliza, who has grown up (andput up) with this book Contents List of Illustrations xiii List of Tables xvii Preface xix Part One: Introduction 1 CHAPTER 1. INTRODUCTION 3 Describing the Living World 3 Why Is Species Description Necessary? 4 How New Species Are Described 8 Scope and Organization of This Book 12 The Pleasures of Systematics 14 Sources CHAPTER 2. BIOLOGICAL NOMENCLATURE 19 Humans as Taxonomists 19 Biological Nomenclature 21 Folk Taxonomy 23 Binomial Nomenclature 25 Development of Codes of Nomenclature 26 The Current Codes of Nomenclature 50 Future of the Codes 36 Sources 39 Part Two: Recognizing Species 41 CHAPTER 3. -

Invasive Reptiles and Amphibians of Florida!
1 Invasive Reptiles and Amphibians of Florida! 2 Created by: Thompson Antony Lauren Diaz Sean McKnight Alana Palau JoAnna Platzer Illustrated by Lauren Diaz Invasive Ecology of Reptiles and Amphibians Dr. Steven Johnson & Dr. Christina Romagosa University of Florida 2014 ---------------------------------------------------------------------------------------------------------------------------- Welcome What is an invasive species? Where are they found in Florida? What do they look like? How can I help? You came to the right coloring book, my friend! These questions and so many more can be answered by grabbing some crayons and turning the page. Things you will need: Your favorite coloring utensils Thinking cap 3 What is an INVASIVE SPECIES ??? An invasive species is a plant or animal that is moved from its native area to another and causes economic or environmental harm to the new area. There are 6 main ways a plant or animal can move from its native home to a non-native area: 1. Biological control: moved by humans to help control other animals 2. Hitchhike: catches a free ride on cars, boats, or planes 3. Food: Some people eat frog legs or other animal parts 4. Plant trade: hiding in a plant is a sneaky way to travel 5. Pet Trade: people want animals they can’t find in their backyard 6. Intentional: Someone brought it for some specific reason For many invasive reptiles and amphibians in Florida, the animals came through the pet trade. 4 Brown Anole Anolis sagrei This is a Cuban Brown Anole! The brown anole is originally from Cuba, but came to Florida when it hitched a ride on some cargo. -

Baseline Ecological Inventory for Three Bays National Park, Haiti OCTOBER 2016
Baseline Ecological Inventory for Three Bays National Park, Haiti OCTOBER 2016 Report for the Inter-American Development Bank (IDB) 1 To cite this report: Kramer, P, M Atis, S Schill, SM Williams, E Freid, G Moore, JC Martinez-Sanchez, F Benjamin, LS Cyprien, JR Alexis, R Grizzle, K Ward, K Marks, D Grenda (2016) Baseline Ecological Inventory for Three Bays National Park, Haiti. The Nature Conservancy: Report to the Inter-American Development Bank. Pp.1-180 Editors: Rumya Sundaram and Stacey Williams Cooperating Partners: Campus Roi Henri Christophe de Limonade Contributing Authors: Philip Kramer – Senior Scientist (Maxene Atis, Steve Schill) The Nature Conservancy Stacey Williams – Marine Invertebrates and Fish Institute for Socio-Ecological Research, Inc. Ken Marks – Marine Fish Atlantic and Gulf Rapid Reef Assessment (AGRRA) Dave Grenda – Marine Fish Tampa Bay Aquarium Ethan Freid – Terrestrial Vegetation Leon Levy Native Plant Preserve-Bahamas National Trust Gregg Moore – Mangroves and Wetlands University of New Hampshire Raymond Grizzle – Freshwater Fish and Invertebrates (Krystin Ward) University of New Hampshire Juan Carlos Martinez-Sanchez – Terrestrial Mammals, Birds, Reptiles and Amphibians (Françoise Benjamin, Landy Sabrina Cyprien, Jean Roudy Alexis) Vermont Center for Ecostudies 2 Acknowledgements This project was conducted in northeast Haiti, at Three Bays National Park, specifically in the coastal zones of three communes, Fort Liberté, Caracol, and Limonade, including Lagon aux Boeufs. Some government departments, agencies, local organizations and communities, and individuals contributed to the project through financial, intellectual, and logistical support. On behalf of TNC, we would like to express our sincere thanks to all of them. First, we would like to extend our gratitude to the Government of Haiti through the National Protected Areas Agency (ANAP) of the Ministry of Environment, and particularly Minister Dominique Pierre, Ministre Dieuseul Simon Desras, Mr.