PSI Appendix F
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

The Relations Between Anemia and Female Adolescent's Dysmenorrhea
Universitas Ahmad Dahlan International Conference on Public Health The Relations Between Anemia and Female Adolescent’s Dysmenorrhea Paramitha Amelia Kusumawardani, Cholifah Diploma Program of Midwifery, Health Science Faculty , University of Muhammadiyah Sidoarjo Article Info ABSTRACT Keyword: Dysmenorrhea described as painful cramps in the lower abdomen that Anemia, occur during menstruation and the infection indications, pelvic disease Dysmenorrhea, moreover in the severe cases it caused fainted. The women who Female adolescents. complained dysmenorrhea problems mostly are who experience menstruation at any age. That means there is no limits age and usually dysmenorrhea often occur with dizziness, cold sweating, even fainted. In some countries the dysmenorrhea problem happens quite high as happened in the United States found 60-91% while in Indonesia amounted to 64.25%. as many as 45-75% of female adolescent experienced dysmenorrhea with the chronic or severe pain that effected to their everyday activities The number of teenagers who experience dysmenorrhea is due to high cases of anemia, irregular exercise, and lack of knowledge of nutritional status. In the previous study there are 85% of female adolescent experience dysmenorrhea. The method of this study is a correlational method with cross sectional approach. The data collecting method examining Hb levels. The population and sample of this study was 40 female adolescent The result showed that the female adolescent who had dysmenorrhea with anemia was 26 (92.4%). From the calculation by Exact Fisher the correlation between anemia and dysmenorrhea cases among female adolescent P <0.05 and p = 0.003, there was significant correlation between adolescent’s dysmenorrhea. Based on the result of statistic analysis, it can be concluded that the anemia can be categorized as one of dysmenorrhea causes. -

ICD10 Diagnoses FY2018 AHD.Com
ICD10 Diagnoses FY2018 AHD.com A020 Salmonella enteritis A5217 General paresis B372 Candidiasis of skin and nail A040 Enteropathogenic Escherichia coli A523 Neurosyphilis, unspecified B373 Candidiasis of vulva and vagina infection A528 Late syphilis, latent B3741 Candidal cystitis and urethritis A044 Other intestinal Escherichia coli A530 Latent syphilis, unspecified as early or B3749 Other urogenital candidiasis infections late B376 Candidal endocarditis A045 Campylobacter enteritis A539 Syphilis, unspecified B377 Candidal sepsis A046 Enteritis due to Yersinia enterocolitica A599 Trichomoniasis, unspecified B3781 Candidal esophagitis A047 Enterocolitis due to Clostridium difficile A6000 Herpesviral infection of urogenital B3789 Other sites of candidiasis A048 Other specified bacterial intestinal system, unspecified B379 Candidiasis, unspecified infections A6002 Herpesviral infection of other male B380 Acute pulmonary coccidioidomycosis A049 Bacterial intestinal infection, genital organs B381 Chronic pulmonary coccidioidomycosis unspecified A630 Anogenital (venereal) warts B382 Pulmonary coccidioidomycosis, A059 Bacterial foodborne intoxication, A6920 Lyme disease, unspecified unspecified unspecified A7740 Ehrlichiosis, unspecified B387 Disseminated coccidioidomycosis A080 Rotaviral enteritis A7749 Other ehrlichiosis B389 Coccidioidomycosis, unspecified A0811 Acute gastroenteropathy due to A879 Viral meningitis, unspecified B399 Histoplasmosis, unspecified Norwalk agent A938 Other specified arthropod-borne viral B440 Invasive pulmonary -
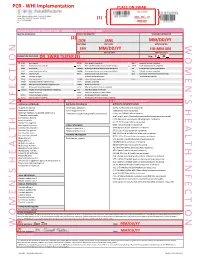
Womens Health Requisition Forms
PCR - WHI Implementation PLACE ON SWAB 10854 Midwest Industrial Blvd. St. Louis, MO 63132 MM DD YY Phone: (314) 200-3040 | Fax (314) 200-3042 (1) CLIA ID #26D0953866 JANE DOE v3 PCR MOLECULAR REQUISITION - WOMEN'S HEALTH INFECTION PRACTICE INFORMATION PATIENT INFORMATION *SPECIMEN INFORMATION (2) DOE JANE MM/DD/YY LAST NAME FIRST NAME DATE COLLECTED W O M E ' N S H E A L T H I F N E C T I O N SSN MM/DD/YY HH:MM AM SSN DATE OF BIRTH TIME COLLECTED REQUESTING PHYSICIAN: DR. SWAB TESTER (3) Sex: F X M (4) Diagnosis Codes X N76.0 Acute vaginitis B37.49 Other urogenital candidiasis A54.9 Gonococcal infection, unspecified N76.1 Subacute and chronic vaginitis N89.8 Other specified noninflammatory disorders of vagina A59.00 Urogenital trichomoniasis, unspecified N76.2 Acute vulvitis O99.820 Streptococcus B carrier state complicating pregnancy A64 Unspecified sexually transmitted disease N76.3 Subacute and chronic vulvitis O99.824 Streptococcus B carrier state complicating childbirth A74.9 Chlamydial infection, unspecified N76.4 Abscess of vulva B95.1 Streptococcus, group B, as the cause Z11.3 Screening for infections with a predmoninantly N76.5 Ulceration of vagina of diseases classified elsewhere sexual mode of trasmission N76.6 Ulceration of vulva Z22.330 Carrier of group B streptococcus Other: N76.81 Mucositis(ulcerative) of vagina and vulva N70.91 Salpingitis, unspecified N76.89 Other specified inflammation of vagina and vulva N70.92 Oophoritis, unspecified N95.2 Post menopausal atrophic vaginitis N71.9 Inflammatory disease of uterus, unspecified -

Endometritis Caused by Chlamydia Trachomatis
Br J Vener Dis 1981; 57:191-5 Endometritis caused by Chlamydia trachomatis P-A MARDH,* B R M0LLER,t H J INGERSELV,* E NUSSLER,* L WESTROM,§ AND P W0LNER-HANSSEN§ From the *Institute of Medical Microbiology, University of Lund, Sweden; the tlnstitute of Medical Microbiology, University of Aarhus, Denmark; the *Department of Obstetrics and Gynaecology, Municipal Hospital, Aarhus, Denmark; and the §Department of Obstetrics and Gynaecology, University Hospital, Lund, Sweden SUMMARY Chlamydia trachomatis was found to be the aetiological agent of endometritis in three women with concomitant signs of salpingitis. All patients developed a significant antibody response to the organism. Chlamydia were recovered from aspirated uterine contents of two patients and darkfield examination of histological sections showed chlamydial inclusions in endometrial cells in one patient. Thus, C trachomatis can be recovered from the endometrium of patients in whom the cervical culture result is negative. In one patient curettage showed endometritis with a characteristic plasma-cell infiltration. The occurrence of chlamydial endometritis may explain why irregular bleeding is a common finding in patients with salpingitis. It also suggests a canalicular spread of chlamydia from the cervix to the Fallopian tubes. Introduction hominis and Ureaplasma urealyticum by cotton- tipped wooden sticks. Specimens for the isolation of Chlamydia trachomatis has been associated with N gonorrhoeae from the cervix and rectum were cervicitis' and salpingitis,2 and perihepatitis may collected with cotton-tipped wooden swabs treated occur in women with chlamydial genital infection.3 with charcoal. Salpingitis caused by chlamydia4 and gonococci5 are histologically similar. Gonococcal salpingitis is an Endometrial contents endosalpingitis and the infection spreads to the For the collection of end6metrial contents, a plastic Fallopian tubes from the cervix via the tube (armoured with a mandrin) was introduced endometrium.5 Experimental salpingitis in monkeys through the cervical canal. -

N35.12 Postinfective Urethral Stricture, NEC, Female N35.811 Other
N35.12 Postinfective urethral stricture, NEC, female N35.811 Other urethral stricture, male, meatal N35.812 Other urethral bulbous stricture, male N35.813 Other membranous urethral stricture, male N35.814 Other anterior urethral stricture, male, anterior N35.816 Other urethral stricture, male, overlapping sites N35.819 Other urethral stricture, male, unspecified site N35.82 Other urethral stricture, female N35.911 Unspecified urethral stricture, male, meatal N35.912 Unspecified bulbous urethral stricture, male N35.913 Unspecified membranous urethral stricture, male N35.914 Unspecified anterior urethral stricture, male N35.916 Unspecified urethral stricture, male, overlapping sites N35.919 Unspecified urethral stricture, male, unspecified site N35.92 Unspecified urethral stricture, female N36.0 Urethral fistula N36.1 Urethral diverticulum N36.2 Urethral caruncle N36.41 Hypermobility of urethra N36.42 Intrinsic sphincter deficiency (ISD) N36.43 Combined hypermobility of urethra and intrns sphincter defic N36.44 Muscular disorders of urethra N36.5 Urethral false passage N36.8 Other specified disorders of urethra N36.9 Urethral disorder, unspecified N37 Urethral disorders in diseases classified elsewhere N39.0 Urinary tract infection, site not specified N39.3 Stress incontinence (female) (male) N39.41 Urge incontinence N39.42 Incontinence without sensory awareness N39.43 Post-void dribbling N39.44 Nocturnal enuresis N39.45 Continuous leakage N39.46 Mixed incontinence N39.490 Overflow incontinence N39.491 Coital incontinence N39.492 Postural -

Intravenous Drug Use-Associated Infective Endocarditis in Pregnant Patients at a Hospital in West Virginia
Open Access Original Article DOI: 10.7759/cureus.17218 Intravenous Drug Use-Associated Infective Endocarditis in Pregnant Patients at a Hospital in West Virginia Deena Dahshan 1 , Mohamed Suliman 2 , Ebad U. Rahman 3 , Zachary Curtis 1 , Ellen Thompson 2 1. Internal Medicine, Marshall University Joan C. Edwards School of Medicine, Huntington, USA 2. Cardiology, Marshall University Joan C. Edwards School of Medicine, Huntington, USA 3. Internal Medicine, St. Mary's Medical Center, Huntington, USA Corresponding author: Deena Dahshan, [email protected] Abstract Introduction Due to high levels of intravenous drug use (IVDU) in West Virginia (WV), there are increasing numbers of hospitalizations for infective endocarditis (IE). More specifically, pregnant patients with IE are a uniquely challenging population, with complex management and a clinical course that further affects the health of the fetus, with high morbidity and mortality. Timely recognition and awareness of the most common bacterial causes will provide hospitals and clinicians with valuable information to manage future patients. Methods This retrospective study analyzed the clinical course of pregnant patients admitted with IE and IVDU history presenting at Cabell Huntington Hospital from 2013 to 2018. Inclusion criteria were women between 16 and 45 years of age confirmed to be pregnant by urine pregnancy test and ultrasonography with at least eight weeks gestation, with a first-time diagnosis of endocarditis and an identified history of IVDU. We excluded charts with pre-existing risk factors including a history of valvular disease, rheumatic heart disease, surgical valve repair or mechanical valve replacement, or a diagnosis of coagulopathies. The resulting charts were evaluated for isolated organisms, reported clinical course, and complications of the pregnancy. -

Diseases of the Digestive System (KOO-K93)
CHAPTER XI Diseases of the digestive system (KOO-K93) Diseases of oral cavity, salivary glands and jaws (KOO-K14) lijell Diseases of pulp and periapical tissues 1m Dentofacial anomalies [including malocclusion] Excludes: hemifacial atrophy or hypertrophy (Q67.4) K07 .0 Major anomalies of jaw size Hyperplasia, hypoplasia: • mandibular • maxillary Macrognathism (mandibular)(maxillary) Micrognathism (mandibular)( maxillary) Excludes: acromegaly (E22.0) Robin's syndrome (087.07) K07 .1 Anomalies of jaw-cranial base relationship Asymmetry of jaw Prognathism (mandibular)( maxillary) Retrognathism (mandibular)(maxillary) K07.2 Anomalies of dental arch relationship Cross bite (anterior)(posterior) Dis to-occlusion Mesio-occlusion Midline deviation of dental arch Openbite (anterior )(posterior) Overbite (excessive): • deep • horizontal • vertical Overjet Posterior lingual occlusion of mandibular teeth 289 ICO-N A K07.3 Anomalies of tooth position Crowding Diastema Displacement of tooth or teeth Rotation Spacing, abnormal Transposition Impacted or embedded teeth with abnormal position of such teeth or adjacent teeth K07.4 Malocclusion, unspecified K07.5 Dentofacial functional abnormalities Abnormal jaw closure Malocclusion due to: • abnormal swallowing • mouth breathing • tongue, lip or finger habits K07.6 Temporomandibular joint disorders Costen's complex or syndrome Derangement of temporomandibular joint Snapping jaw Temporomandibular joint-pain-dysfunction syndrome Excludes: current temporomandibular joint: • dislocation (S03.0) • strain (S03.4) K07.8 Other dentofacial anomalies K07.9 Dentofacial anomaly, unspecified 1m Stomatitis and related lesions K12.0 Recurrent oral aphthae Aphthous stomatitis (major)(minor) Bednar's aphthae Periadenitis mucosa necrotica recurrens Recurrent aphthous ulcer Stomatitis herpetiformis 290 DISEASES OF THE DIGESTIVE SYSTEM Diseases of oesophagus, stomach and duodenum (K20-K31) Ill Oesophagitis Abscess of oesophagus Oesophagitis: • NOS • chemical • peptic Use additional external cause code (Chapter XX), if desired, to identify cause. -

Prioritization of Health Services
PRIORITIZATION OF HEALTH SERVICES A Report to the Governor and the 74th Oregon Legislative Assembly Oregon Health Services Commission Office for Oregon Health Policy and Research Department of Administrative Services 2007 TABLE OF CONTENTS List of Figures . iii Health Services Commission and Staff . .v Acknowledgments . .vii Executive Summary . ix CHAPTER ONE: A HISTORY OF HEALTH SERVICES PRIORITIZATION UNDER THE OREGON HEALTH PLAN Enabling Legislatiion . 3 Early Prioritization Efforts . 3 Gaining Waiver Approval . 5 Impact . 6 CHAPTER TWO: PRIORITIZATION OF HEALTH SERVICES FOR 2008-09 Charge to the Health Services Commission . .. 25 Biennial Review of the Prioritized List . 26 A New Prioritization Methodology . 26 Public Input . 36 Next Steps . 36 Interim Modifications to the Prioritized List . 37 Technical Changes . 38 Advancements in Medical Technology . .42 CHAPTER THREE: CLARIFICATIONS TO THE PRIORITIZED LIST OF HEALTH SERVICES Practice Guidelines . 47 Age-Related Macular Degeneration (AMD) . 47 Chronic Anal Fissure . 48 Comfort Care . 48 Complicated Hernias . 49 Diagnostic Services Not Appearing on the Prioritized List . 49 Non-Prenatal Genetic Testing . 49 Tuberculosis Blood Test . 51 Early Childhood Mental Health . 52 Adjustment Reactions In Early Childhood . 52 Attention Deficit and Hyperactivity Disorders in Early Childhood . 53 Disruptive Behavior Disorders In Early Childhood . 54 Mental Health Problems In Early Childhood Related To Neglect Or Abuse . 54 Mood Disorders in Early Childhood . 55 Erythropoietin . 55 Mastocytosis . 56 Obesity . 56 Bariatric Surgery . 56 Non-Surgical Management of Obesity . 58 PET Scans . 58 Prenatal Screening for Down Syndrome . 59 Prophylactic Breast Removal . 59 Psoriasis . 59 Reabilitative Therapies . 60 i TABLE OF CONTENTS (Cont’d) CHAPTER THREE: CLARIFICATIONS TO THE PRIORITIZED LIST OF HEALTH SERVICES (CONT’D) Practice Guidelines (Cont’d) Sinus Surgery . -

Practice Parameter for the Diagnosis and Management of Primary Immunodeficiency
Practice parameter Practice parameter for the diagnosis and management of primary immunodeficiency Francisco A. Bonilla, MD, PhD, David A. Khan, MD, Zuhair K. Ballas, MD, Javier Chinen, MD, PhD, Michael M. Frank, MD, Joyce T. Hsu, MD, Michael Keller, MD, Lisa J. Kobrynski, MD, Hirsh D. Komarow, MD, Bruce Mazer, MD, Robert P. Nelson, Jr, MD, Jordan S. Orange, MD, PhD, John M. Routes, MD, William T. Shearer, MD, PhD, Ricardo U. Sorensen, MD, James W. Verbsky, MD, PhD, David I. Bernstein, MD, Joann Blessing-Moore, MD, David Lang, MD, Richard A. Nicklas, MD, John Oppenheimer, MD, Jay M. Portnoy, MD, Christopher R. Randolph, MD, Diane Schuller, MD, Sheldon L. Spector, MD, Stephen Tilles, MD, Dana Wallace, MD Chief Editor: Francisco A. Bonilla, MD, PhD Co-Editor: David A. Khan, MD Members of the Joint Task Force on Practice Parameters: David I. Bernstein, MD, Joann Blessing-Moore, MD, David Khan, MD, David Lang, MD, Richard A. Nicklas, MD, John Oppenheimer, MD, Jay M. Portnoy, MD, Christopher R. Randolph, MD, Diane Schuller, MD, Sheldon L. Spector, MD, Stephen Tilles, MD, Dana Wallace, MD Primary Immunodeficiency Workgroup: Chairman: Francisco A. Bonilla, MD, PhD Members: Zuhair K. Ballas, MD, Javier Chinen, MD, PhD, Michael M. Frank, MD, Joyce T. Hsu, MD, Michael Keller, MD, Lisa J. Kobrynski, MD, Hirsh D. Komarow, MD, Bruce Mazer, MD, Robert P. Nelson, Jr, MD, Jordan S. Orange, MD, PhD, John M. Routes, MD, William T. Shearer, MD, PhD, Ricardo U. Sorensen, MD, James W. Verbsky, MD, PhD GlaxoSmithKline, Merck, and Aerocrine; has received payment for lectures from Genentech/ These parameters were developed by the Joint Task Force on Practice Parameters, representing Novartis, GlaxoSmithKline, and Merck; and has received research support from Genentech/ the American Academy of Allergy, Asthma & Immunology; the American College of Novartis and Merck. -

State Medicaid Manual
Page 1 of 37 Louisiana Medicaid Approved Pay and Chase Primary Prenatal Care Diagnosis Codes MCOs must use the "pay and chase" method of payment for prenatal services for individuals with other Health Insurance. The MCO must seek reimbursement from the third party within 60 days after the end of the month in which payment is made. Primary prenatal diagnoses which do not require primary health insurance claim filing by most providers are confined to those listed below. Hospitals are not included and must continue to file claims with the primary health insurance carriers. ICD-9-CM to ICD-10 crosswalk for Prenatal Diagnosis Codes ICD-9-CM Description Code V22.0 Supervision of normal pregnancy V22.1 V23 Supervision of high risk pregnancy V28 Antenatal screening 640-648 Complications related to pregnancy 651-658 Other conditions requiring care in 671 pregnancy 673 675-676 ICD-10-CM Diagnosis Codes – for Prenatal Services upon Implementation of ICD-10 ICD-9-CM code V22.0 maps to the following ICD-10-CM codes Z3400 Encounter for supervision of normal first pregnancy, unspecified trimester Z3403 Encounter for supervision of normal first pregnancy, third trimester Z3401 Encounter for supervision of normal first pregnancy, first trimester Z3402 Encounter for supervision of normal first pregnancy, second trimester ICD-9-CM code V22. -

Cervical Erosion As Result of Infectious Vaginitis
Available online a t www.pelagiaresearchlibrary.com Pelagia Research Library European Journal of Experimental Biology, 2012, 2 (5):1659-1663 ISSN: 2248 –9215 CODEN (USA): EJEBAU Cervical erosion as result of infectious vaginitis Sánchez A1, Rivera A 2* , Castillo F1 and Ortiz S1 1 Departamento de Biología Celular, Facultad de Medicina de la Benemérita Universidad Autónoma de Puebla, México. 2 Centro de Investigaciones en Ciencias Microbiológicas, Instituto de Ciencias de la Benemérita Universidad Autónoma de Puebla. _____________________________________________________________________________________________ ABSTRACT The vulvovaginitis can occur at any stage of life, being 90% of bacterial origin, parasitic and fungal agents such as Chlamydia trachomatis, Gardnerella vaginalis, Trichomonas vaginalis and Candida albicans causing erosion of cervical epithelium, so this study aims to demonstrate that vaginitis infectious agents cause erosion of the cervix of a total of 1033 patients who came to the Laboratorio de Biología Celular de la Facultad de Medicina de la Universidad Autónoma de Puebla, México in January 2001 to December 2009 the Cancer Screening Program which underwent Papanicolaou smears, the samples were stained by the modified Papanicolaou method and observed under a microscope. As for the results of 1033 patients, 378 showed vaginitis, of these, 301 were associated with infectious vaginitis and 77 without identified microorganisms but with signs of vaginitis (probably by irritation to some physical agent or vitamin A deficiency). The microorganisms found in 301 patients with vaginitis were as follows: 173 samples with abundant coccoid flora, 63 associated with flora coccoid and fungi, 37 fungi, 16 trichomonas, 3 coconuts associated with trichomonas, 3 fungi associated with Trichomonas, 2 with Trichomonas, fungi and coccoid, 2 with Gardnerella, 1 coccoid flora, and 1 Gardnerella associated with coconuts . -

Moraxella Catarrhalis and Haemophilus Influenzae
The Other Siblings: Respiratory Infections Caused by Moraxella catarrhalis and Haemophilus influenzae Larry Lutwick, MD, and Laila Fernandes, MD Corresponding author Moraxella catarrhalis Larry Lutwick, MD Infectious Diseases (IIIE), VA Medical Center, 800 Poly Place, Bacteriology Brooklyn, NY 11219, USA. M. catarrhalis is a Gram negative, aerobic diplococcus E-mail: [email protected] that was initially described by Anton Ghon and Rich- Current Infectious Disease Reports 2006, 8:215–221 ard Pfeiffer as Micrococcus catarrhalis at the end of the Current Science Inc. ISSN 1523-3847 19th century. For most of the first century of its rec- Copyright © 2006 by Current Science Inc. ognition, M. catarrhalis is considered to be a human mucosal commensal organism based on its common finding as an inhabitant of the oropharynx of healthy Respiratory infections remain substantial causes of mor- adults. During a significant amount of this time, based bidity and mortality globally. In this paper, two substantial on phenotypic characteristics as well as microbiologic players in bacterial-associated respiratory disease are colony appearances, the diplococcus was referred to assessed as to their respective roles in children and adults as Neisseria catarrhalis. Of note, in 1963, N. catarrhalis and in the developed and developing world. Moraxella was found to contain two distinct species, catarrhalis catarrhalis, although initially thought to be a nonpathogen, and cinerea [1]. continues to emerge as a cause of upper respiratory Reclassification of the genus of this microorganism disease in children and pneumonia in adults. No vaccine occurred in 1970 when significant phylogenetic dispari- is currently available to prevent M.