2019 Greater Lowell Community Health Needs Assessment
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Older Workers Rock! We’Re Not Done Yet!
TM TM Operation A.B.L.E. 174 Portland Street Tel: 617.542.4180 5th Floor E: [email protected] Boston, MA 02114 W: www.operationable.net Older Workers Rock! We’re Not Done Yet! A.B.L.E. SCSEP Office Locations: SCSEP Suffolk County, MA Workforce Central SCSEP Hillsborough County, NH 174 Portland Street, 5th Floor 340 Main Street 228 Maple Street., Ste 300 Boston, MA 02114 Ste.400 Manchester, NH 03103 Phone: 617.542.4180 Worcester, MA 01608 Phone: 603.206.4405 eMail: [email protected] Tel: 508.373.7685 eMail: [email protected] eMail: [email protected] SCSEP Norfolk, Metro West & SCSEP Coos County, NH Worcester Counties, MA Career Center 961 Main Street Quincy SCSEP Office of North Central MA Berlin, NH 03570 1509 Hancock Street, 4th Floor 100 Erdman Way Phone: 603.752.2600 Quincy, MA 02169 Leominster, MA 01453 eMail: [email protected] Phone: 617-302-2731 Tel: 978.534.1481 X261 and 617-302-3597 eMail: [email protected] eMail: [email protected] South Middlesex GETTING WORKERS 45+ BACK TO WORK SINCE 1982 SCSEP Essex & Middlesex Opportunity Council Counties, MA 7 Bishop Street Job Search Workshops | Coaching & Counseling | Training | ABLE Friendly Employers | Resource Room Framingham, MA 01702 280 Merrimack Street Internships | Apprenticeships | Professional Networking | Job Clubs | Job Seeker Events Building B, Ste. 400 Tel: 508.626.7142 Lawerence, MA 01843 eMail: [email protected] Phone: 978.651.3050 eMail: [email protected] 2018 Annual Report September 2018 At Operation A.B.L.E., we work very hard to Operation A.B.L.E. Addresses the Changing Needs keep the quality of our programs up and our costs down. -

Tab11 Title I Performance Quarterly
TAB 11 FY05 WIA TITLE I PERFORMANCE MEASURE SUMMARY BY WIB AREA Quarterly Report Period Ending 6/30/05 ADULT MEASURES Chart 1: Entered Employment Chart 2: Credential Chart 3: Employment Retention Chart 4: Earnings Gain DISLOCATED WORKER MEASURES Chart 5: Entered Employment Chart 6: Credential Chart 7: Employment Retention Chart 8: Earnings Gain OLDER YOUTH MEASURES Chart 9: Entered Employment Chart 10: Credential Chart 11: Employment Retention Chart 12: Earnings Gain YOUNGER YOUTH MEASURES Chart 13: Skill Attainment Chart 14: Diploma/GED Attainment Chart 15: Employment/Education Retention Data Source: WIA Title I Quarterly Report Data (ETA 9090) Compiled by Performance and Reporting Department, Massachusetts Division of Career Services Report Date: 8/12/2005 COMMONWEALTH OF MASSACHUSETTS WIA TITLE I PERFORMANCE MEASURES: FY05 QUARTERLY PERIOD ENDING 06/30/2005 CHART 1- ADULT ENTERED EMPLOYMENT RATE IN FIRST QUARTER AFTER EXIT [B] [C] [D] [E=B-C-D] [F] [G] [H=F+G] [I=H/E] [J] [K=I/J] Total Medical & Employed at Adjusted Number of Number of Total Number Entered Local Percent of Workforce Number of Other Registration Number of Wage Record Supplemental of Entered Employment Performance Local Goal Investment Area Exiters Exclusions Exiters Matches Employments Employments Rate Level Goal Berkshire 47 4 3 40 28 3 31 78% 74% 105% Boston 196 4 36 156 115 4 119 76% 70% 109% Bristol 58 4 5 49 35 1 36 74% 71% 104% Brockton 59 2 8 49 35 6 41 84% 74% 113% Cape Cod, Vineyard, Nantucket 59 2 10 47 26 7 33 70% 70% 100% Central Mass 80 3 7 70 51 9 60 86% -

Your NAMI State Organization
Your NAMI State Organization State: Massachusetts State Organization: NAMI Massachusetts Address: NAMI Massachusetts 529 Main St Ste 1M17 Boston, MA 02129-1127 Phone: (617) 580-8541 Fax: (617) 580-8673 Email Address: [email protected] Website: http://www.namimass.org President: Mathieu Bermingham Affiliate Name Contact Info NAMI Berkshire County Address: NAMI Berkshire County 333 East St Room 417 Pittsfield, MA 01201-5312 Phone: (413) 443-1666 Email Address: [email protected] Website: http://www.namibc.org Serving: Berkshire County NAMI Bristol County, MA Email Address: [email protected] Website: http://www.namibristolcounty.org NAMI Cambridge/Middlesex Phone: (617) 984-0527 Email Address: [email protected] Website: http://www.nami-cambridgemiddlesex.org Serving: Allston, Arlington, Belmont, Brighton, Brookline, Cambridge, Charlestown, Somerville, Greater Boston NAMI Cape Ann Address: NAMI Cape Ann 43 Gloucester Avenue Gloucester, MA 01930 Phone: (978) 281-1557 Email Address: [email protected] Website: http://www.namicapeann.org Serving: Cape Ann area, MA NAMI Cape Cod Address: NAMI Cape Cod 5 Mark Ln Hyannis, MA 02601-3792 Phone: (508) 778-4277 Email Address: [email protected] Website: http://www.namiCapeCod.org Serving: Cape Cod and The Islands NAMI Central MA Address: NAMI Central MA 309 Belmont St Rm G1B9 Worcester, MA 01604-1059 Phone: (508) 368-3562 Email Address: [email protected] NAMI Central Middlesex Address: NAMI Central Middlesex PO Box 2793 Acton, MA 01720-6793 Phone: (781) 982-3318 -

Ocm85835802-2010-Lowell.Pdf (692.4Kb)
Massachusetts Department of WorkDevelopmentforce Regional LMI Profile Annual Profile for Greater Lowell Workforce Area May 2010 Commonwealth of Massachusetts Executive Office of Labor and Workforce Development MassLMI Labor Market Information Joanne F. Goldstein Table of Contents (Workforce Area) Overview and Highlights Pages 1-4 Labor market and population highlights of the workforce area. Workforce Area Maps Pages 5-7 Map of the 16 workforce areas in Massachusetts, map of individual workforce area, and an alphabetical listing of the cities and towns within each workforce area. Profile of Unemployment Insurance Claimants Page 8 Grid of unemployment claims statewide and by workforce area for March 2010. Demographic data is displayed for race, gender, and Hispanic or Latino status. Also provided is the duration of unemployment, the average weekly wage during the 12 months prior to the filing, age group, and level of educational attainment. Page 9 March 2010 data on continued claimants for unemployment insurance residing in the local workforce area. Demographic data are displayed for race, gender and Hispanic or Latino status of the claimants. Data are also provided for length of the current spell of unemployment, the average weekly wage during the 12 months prior to filing, age group, and level of educational attainment. For comparison purposes statewide statistics are also provided. Page 10 The occupational categories of the continued claimants arranged in accordance with 22 major groups of the Standard Occupational Classification (SOC) system. The accompanying chart compares the occupational distribution of claimants in the local area with the statewide claimants for the ten largest groups. Page 11 The industry distribution of the continued claimants’ former employer grouped into the 2-digit sectors of the North American Industry Classification System (NAICS). -

GREATER LOWELL REGIONAL OPEN SPACE STRATEGY: Analysis and Recommendations
. THE GREATER LOWELL REGIONAL OPEN SPACE STRATEGY: Analysis and Recommendations Prepared for The Trustees of Reservations by the Northern Middlesex Council of Governments Funding Provided by the Theodore Edson Parker Foundation and the Northern Middlesex Council of Governments December 2002 . The Trustees of Reservations 572 Essex Street Beverly, MA 01915 www.thetrustees.org Andrew Kendall, Executive Director Wesley T. Ward, Director of Land Conservation Chris Rodstrom, Land Protection Specialist Northern Middlesex Council of Governments Gallagher Terminal, Floor 3B 115 Thorndike Street Lowell, MA 01852 www.nmcog.org Ellen Rawlings, Chair Robert W. Flynn, Executive Director December 2002 Prepared by Larissa Brown, Chief Regional Planner, NMCOG John Matley, GIS Specialist, NMCOG . THE GREATER LOWELL REGIONAL OPEN SPACE STRATEGY: Analysis and Recommendations . Prepared for The Trustees of Reservations by the Northern Middlesex Council of Governments Funding Provided by the Theodore Edson Parker Foundation and the Northern Middlesex Council of Governments December 2002 . TABLE OF CONTENTS I. Executive Summary 1 II. Open Space, Regional Networks and Green Infrastructure 4 III. The Environmental and Development History of the Greater Lowell Region 7 IV. Current Conditions and Open Space Planning 11 V. The Landscape Ecology of the Greater Lowell Region 28 VI. Open Space Needs and Gaps 32 VII. Regional Opportunities and Strategies for Open Space Collaboration 35 VIII. An Open Space Strategy for the Greater Lowell Region 51 References 55 Maps Map 1: Environmental Resources Map 2: Land Use and Development Pressures Map 3: Protected Open Space, Recreational and Cultural Landscapes Map 4: Landscape Mosaic Map 5: Regional Open Space Opportunities . I. EXECUTIVE SUMMARY With its range of environments—from protected forests and wetlands to farms, suburbs, and an historic urban center—the Greater Lowell Region can offer its residents and visitors a variety of nature and landscape experiences. -

EM28819-16-60-A-25 Mod 0 Grant Agreement
GRANT AWARD - Grant No: EM-28819-16-60-A-25 Mod No.: 0 U.S. DEPARTMENT OF LABOR NOTICE OF EMPLOYMENT AND TRAINING AWARD (NOA) ADMINISTRATION (DOL/ETA) Under the authority of the Workforce Innovation and Opportunity Act (WIOA), Title I, Section 170, National Dislocated Worker Grant, this grant or agreement is entered into between the above named Grantor Agency and the following named Awardee, for a project entitled - MA-Regular~Greater Lowell Multi NDWG. Name & Address of Awardee: Federal Award Id. No. (FAIN): EM-28819-16-60-A-25 Massachusetts - EXECUTIVE OFFICE OF LABOR AND CFDA #: 17.277- Workforce Investment Act (WIA) WORKFORCE DEVELOPMENT National Emergency Grants 19 STANIFORD STREET Amount:$1,040,264.00 1ST FLOOR EIN: 046002284 BOSTON, MASSACHUSETTS 02114 DUNS #: 947581567 Accounting Code: 1630-2016-0501741616BD201601740003165DW093A0000AOWI00AOWI00-A90200-410023-ETA- DEFAULT TASK- The Period of Performance shall be from January 01, 2016 thru September 30, 2017. Total Government's Financial Obligation is $1,040,264.00 (unless other wise amended). Payments will be made under the Payments Management System, and can be automatically drawn down by the awardee on an as needed basis covering a forty-eight (48) hour period. In performing its responsibilities under this grant agreement, the awardee hereby certifies and assures that it will fully comply with all applicable Statute(s), and the following regulations and cost principles, including any subsequent amendments: Uniform Administrative Requirements, Cost Principles, and Audit Requirements: 2 CFR Part 200; Uniform Administrative Requirements, Cost Principles, and Audit Requirements; Final Rule 2 CFR Part 2900; DOL Exceptions to 2 CFR Part 200; Other Requirements (Included within this NOA): Condition(s) of Award (if applicable) Federal Award Terms, including attachments Contact Information The Federal Project Officer (FPO) assigned to this grant is Kathleen Mclaughlin. -
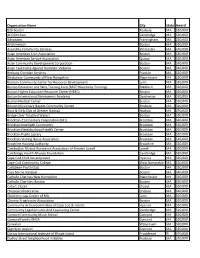
Organization Name
Organization Name City State Award 826 Boston Roxbury MA $10,000 ACCION East Cambridge MA $10,000 Advocates Framingham MA $10,000 ArtsEmerson Boston MA $10,000 Ascentria Community Services Worcester MA $10,000 Asian American Civic Association Boston MA $10,000 Asian American Service Association Quincy MA $10,000 Asian Community Development Corporation Boston MA $10,000 Asian Task Force Against Domestic Violence Boston MA $10,000 Bethany Christian Services Franklin MA $10,000 Bhutanese Community of New Hampshire Manchester NH $10,000 Bosnian Community Center for Resource Development Lynn MA $10,000 Boston Education and Skills Training Corp (BEST Hospitality Training) Medford MA $10,000 Boston Higher Education Resource Center (HERC) Boston MA $10,000 Boston International Newcomers Academy Dorchester MA $10,000 Boston Medical Center Boston MA $10,000 Boston Missionary Baptist Community Center Roxbury MA $10,000 Boys & Girls Club of Greater Nashua Nashua NH $10,000 Bridge Over Troubled Waters Boston MA $10,000 Brockton 21st Century Corporation (B21) Brockton MA $10,000 Brockton Interfaith Community Brockton MA $10,000 Brockton Neighborhood Health Center Brockton MA $10,000 Brockton Public Library Brockton MA $10,000 Brockton Visiting Nurse Association Brockton MA $10,000 Brookline Housing Authority Brookline MA $10,000 Cambodian Mutual Assistance Association of Greater Lowell Lowell MA $10,000 Cambridge Health Alliance Foundation Cambridge MA $10,000 Cape Cod Child Development Hyannis MA $10,000 Cape Cod Community College West Barnstable MA -
Ocm09668846-20012002.Pdf
2001-2002 Public Officers of the COMMONWEALTH of MASSACHUSETTS Prepared and printed under authority of Section 1 8 of Chapter 5 of the General Laws by PATRICK F. SCANLAN Senate Clerk and STEVEN T. JAMES Clerk of the House of Representatives SENATORS FROM MASSACHUSETTS IN THE CONGRESS OF THE UNITED STATES U.S. SENATE EDWARD M. KENNEDY Hyannisport, Democrat. Born: February 22, 1932. Education: Milton Academy; Harvard University, B.A., '56; International Law School, The Hague, Netherlands, '58; University of Virginia Law School, LL.B., '59. Profession: Lawyer. Organizations: Ranking Democrat, Senate Labor and Human Resources Committee; Member, Senate Judiciary Committee, Senate Armed Services Com- mittee, Congressional Joint Economic Committee; Member, Congressional Friends of Ireland, Senate Arms Control Observer Group; Trustee, John F. Kennedy Center for the Performing Arts. Public Office: United States Senate, 1962-2006. U.S. SENATE JOHN F. KERRY One Bowdoin Square, 10th Floor, Boston. Democrat. Born: Denver, CO, December 11, 1943. Education: Yale. '66; Boston College Law School, "76. Profession: Lawyer. Organizations: Vietnam Veterans of America; Honorary Trustee, Museum of Science. Public Office: First Assistant District Attorney , (Middlesex County) 1977- 79; Lieutenant Governor, 1983-'85; United States Senate, 1985- 2002. REPRESENTATIVES FROM MASSACHUSETTS IN THE CONGRESS UNITED STATES U.S. HOUSE MICHAEL EVERETT CAPUANO PO Box 440305, Somerville, 8th District, Democrat. Born: Somerville, January 9, 1952. Education: Dartmouth College; Boston College Law School. Profession: Attorney. Public Office: Alderman; Alderman-at-Large; Mayor of Somerville; Representative in Congress (106th - 107th) 1999-2002. U.S. HOUSE WILLIAM D. DELAHUNT 9 Ketch Lane, Quincy, 10th District, Democrat. Born: Quincy, July 18, 1941. -

About Masshire the Massachusetts State Workforce System
ABOUT MASSHIRE THE MASSACHUSETTS STATE WORKFORCE SYSTEM WHAT IS MASSHIRE? MassHire is a new brand unifying the entire Massachusetts Workforce Development System under a single name and shared mission. Commissioned by the Executive Office of Labor and Workforce Development (EOLWD), it signifies the state’s commitment to increasing meaningful career opportunities for job seekers and expanding the talent pool for businesses seeking trained, skilled employees. The brand, MassHire, unifies and empowers all state, regional, and local workforce entities. It enables them to communicate with clients — job seekers and businesses — with a clear, consistent, powerful message. MassHire provides a foundation for conveying the depth, breadth, and connectivity of its value and services across all audiences. What’s changing? 16 local boards will become MassHire Workforce Boards; 29 career centers will become MassHire Career Centers. The Massachusetts Workforce Development Board will become the MassHire State Workforce Board, and the Department of Career Services will be the MassHire Department of Career Services. When is this happening? Our statewide launch will be on August 29, 2018. Our local workforce boards and career centers will launch in their regions throughout the following two months. Why Rebrand? In discussions with businesses, jobseekers, education partners, workforce development professionals, and other stakeholders, EOLWD gathered extraordinary insight. For example: • It became evident that employers and job seekers are largely unaware of the resources provided by the state’s workforce system. In short, much of our target audience simply didn’t realize they could turn to a statewide network for employment or business services. • We unearthed new challenges and opportunities for more effectively addressing the unique employment and business needs for a dynamic 21st century economy. -

Greater Lowell Health Alliance Annual Report 2019 Letter from the Board Chair
Community and Collaboration Greater Lowell Health Alliance Annual Report 2019 Letter from the Board Chair We are pleased to share with you this annual report highlighting the activities and impact of the Greater Lowell Health Alliance. The growth, impact, and success of the GLHA over the past year—and over the past thirteen GLHA Board of Directors: Front Row: Kerrie D’Entremont, Susan Rosa, Deirdra years—is due in large part to our continued focus Murphy, Amanda Clermont. Back Row: Sovanna Pouv, Andrea Saunders Batchelder, Cece Lynch, Damian Folch. Not pictured: Jayne Andrews, Joel Boyd, Karen Frederick, on collaboration and engagement of individuals and Susan West Levine, Jeffrey Stephens, Kerran Vigroux. organizations throughout our region. The strength of the Alliance is in bringing together healthcare BOARD OF DIRECTORS providers, business leaders, educators, and civic and community leaders and inspiring them to work together to identify and EXECUTIVE COMMITTEE address the health priorities that directly impact our communities. DEIRDRA A. MURPHY, PT, DPT, MS, MHA, Chair As a member of the University of Massachusetts Lowell, I am particularly Associate Dean for Undergraduate Student Success, University of Massachusetts Lowell proud of UMass Lowell’s deep commitment to the GLHA mission. UMass SUSAN WEST LEVINE, Vice Chair Lowell faculty and students dedicated countless hours conducting the 2019 Chief Executive Officer, Lowell Community Greater Lowell Community Health Needs Assessment, including a first-ever Health Center region-wide needs assessment survey, that will provide a strong foundation JAYNE A. ANDREWS, CPA, Treasurer in setting future health priorities. And GLHA’s success simply would not Director of Not-for-Profit Services, Anstiss & Co. -

Greater Lowell Community Health Needs Assessment
Greater Lowell Community Health Needs Assessment Conducted on Behalf of: Lowell General Hospital Saints Medical Center Greater Lowell Health Alliance Authors: A. James Lee, PhD Leland K. Ackerson, ScD Kimberly Flodin, MS Craig Slatin, ScD University of Massachusetts Lowell September 2010 The authors thank the many individuals (as well as the organizations for which they work) who participated in focus group and personal interviews. We also thank Michelle Davis, and Erin Caples for coordinating the hospitals’ involvement and support of our work. Finally, we give special thanks to Alicia Rogers and Amy Stanley for recruiting and scheduling the focus groups and personal interviews. The research was conducted by the Center for Health Promotion and Research at University of Massachusetts Lowell. Executive Summary On behalf of Lowell General Hospital (LGH), Saints Medical Center (SMC) and the Greater Lowell Health Alliance (GLHA), a team of UMass Lowell researchers and students conducted a community health needs assessment study to distinguish the unmet medical and public health needs within the Greater Lowell community. The geographic area assessed included the communities of Lowell, Billerica, Chelmsford, Dracut, Dunstable, Tewksbury, Tyngsborough and Westford. The study had two objectives. One objective was to meet state and federal requirements that the two hospitals conduct a Comprehensive Health Needs Assessment every three years. The second, ultimately more important objective was to conduct a study that would provide a foundation for the GLHA and its partners, including LGH and SMC, in working to build consensus on the area’s health needs and plan coordinated activities to improve the health of the area’s residents. -

Girls Lacrosse
PROPOSED MIAA STATEWIDE POWER RATINGS GIRLS’ LACROSSE (With scoring margin capped at 10 GOALS for any game) TEAM’S AVERAGE AVERAGE OF OVERALL MARGIN OF OPPONENTS’ VICTORY RATINGS RATING Based on results from the 2019 regular season 2019 DIVISION 1 GIRLS' LACROSSE (Margin ratings … 10-goal cap) SEED TEAM W L T RATING 1 Notre Dame (Hingham) 17 3 0 17.09 2 Needham 16 4 0 15.84 1 Notre Dame (Hingham) Needham 2 3 Wellesley 16 4 0 14.13 4 Concord-Carlisle 15 4 0 13.78 5 Franklin 18 2 0 13.43 32 Framingham Brookline 31 6 Lincoln-Sudbury 13 5 0 13.11 7 Chelmsford 16 4 0 12.01 33 Methuen New Bedford 34 8 Natick 13 5 0 11.53 9 Central Catholic 13 5 0 10.46 10 North Andover 16 5 0 10.41 16 Boston Latin Peabody 15 11 Algonquin 13 5 0 10.14 12 Braintree 11 7 0 9.13 13 Woburn 13 6 0 8.87 14 Lexington 17 3 0 8.68 17 Newton North Acton-Boxboro 18 15 Peabody 13 5 0 7.70 16 Boston Latin 13 5 0 7.41 17 Newton North 13 8 0 7.20 18 Acton-Boxboro 8 10 0 7.13 8 Natick Chelmsford 7 19 Shrewsbury 9 9 0 6.95 20 Marshfield 11 7 0 6.83 21 Westford Academy 5 13 0 6.22 22 Lowell 14 3 0 5.99 25 Andover Mansfield 26 23 Beverly 8 10 0 5.57 24 Bishop Feehan 12 8 0 5.07 25 Andover 6 13 0 4.82 26 Mansfield 10 8 0 4.52 9 Central Catholic North Andover 10 27 Belmont 11 9 0 4.17 28 Westfield 12 6 0 4.04 29 Bridgewater-Raynham 7 6 0 3.66 30 Weymouth 5 15 0 3.41 24 Bishop Feehan Beverly 23 31 Brookline 5 14 0 3.21 32 Framingham 4 14 0 3.14 33 Methuen 9 9 0 2.06 Arlington 7 9 0 1.78 4 Concord-Carlisle Wellesley 3 Newton South 5 13 0 1.43 Wachusett 5 13 0 0.56 Cambridge 8 9 0