Vaccine Adjuvants Derived from Marine Organisms
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Vaccine Information for PARENTS and CAREGIVERS
NATIONAL INSTITUTE FOR COMMUNICABLE DISEASES Division of the National Health Laboratory Service VACCINE INFOR MATION FOR PARENTS & CAREGIVERS First Edition November 2016 Editors-in-Chief Nkengafac Villyen Motaze (MD, MSc, PhD fellow), Melinda Suchard (MBBCh, FCPath (SA), MMed) Edited by: Cheryl Cohen, (MBBCh, FCPath (SA) Micro, DTM&H, MSc (Epi), Phd) Lee Baker, (Dip Pharm) Lucille Blumberg, (MBBCh, MMed (Micro) ID (SA) FFTM (RCPS, Glasgow) DTM&H DOH DCH) Published by: Ideas Wise and Wonderful (IWW) for National Institute for Communicable Diseases (NICD) First Edition: Copyright © 2016 Contributions by: Clement Adu-Gyamfi (BSc Hons, MSc), Jayendrie Thaver (BSc), Kerrigan McCarthy, (MBBCh, FCPath (SA), DTM&H, MPhil (Theol) Kirsten Redman (BSc Hons), Nishi Prabdial-Sing (PhD), Nonhlanhla Mbenenge (MBBCh, MMED) Philippa Hime (midwife), Vania Duxbury (BSc Hons), Wayne Howard (BSc Hons) Acknowledgments: Amayeza, Vaccine Information Centre (http://www.amayeza-info.co.za/) Centre for Communicable Diseases Fact Sheets (http://www.cdc.gov/vaccines/hcp/vis/) World Health Organization Fact Sheets (http://www.who.int/mediacentre/factsheets/en/) National Department of Health, South Africa (http://www.health.gov.za/) Disclaimer This book is intended as an educational tool only. Information may be subject to change as schedules or formulations are updated. Summarized and simplified information is presented in this booklet. For full prescribing information and contraindications for vaccinations, please consult individual package inserts. There has been -
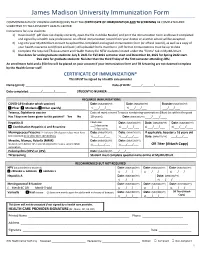
Immunization-Form.Pdf
James Madison University Immunization Form COMMONWEALTH OF VIRGINIA LAW REQUIRES THAT THE CERTIFICATE OF IMMUNIZATION AND TB SCREENING BE COMPLETED AND SUBMITTED TO THE UNIVERSITY HEALTH CENTER. Instructions for new students: 1) Download (if .pdf does not display correctly, open the file in Adobe Reader) and print the Immunization Form and have it completed and signed by a health care professional. An official immunization record from your doctor or another school will be accepted. 2) Log into your MyJMUChart account to upload the completed and signed immunization form (or official record), as well as a copy of your health insurance card (front and back.) All uploaded forms must be in .pdf format. Immunizations must be up to date. 3) Complete the required TB Assessment and Health History for NEW students located under the “forms” tab in MyJMUChart. Due dates for undergraduate students: July 8, 2021 for Fall 2021 semester start and December 10, 2021 for Spring 2022 start. Due date for graduate students: No later than the third Friday of the first semester attending JMU. An enrollment hold and a $50 fine will be placed on your account if your immunization form and TB Screening are not deemed complete by the Health Center staff. CERTIFICATE OF IMMUNIZATION* This MUST be signed by a health care provider Name (print): _______________________________________________ Date of Birth: ______/_______/_______________ Date completed: _______/_______/_______ STUDENT ID NUMBER: __________________________ REQUIRED IMMUNIZATIONS COVID-19 (indicate which -
Typhoid Vaccine W H a T Y O U N E E D T O K N O W
TYPHOID VACCINE W H A T Y O U N E E D T O K N O W Many Vaccine Information Statements are available in Spanish and other languages. See www.immunize.org/vis. What is typhoid? •Travelers to parts of the world where typhoid is 1 common. (NOTE: typhoid vaccine is not 100% Typhoid (typhoid fever) is a serious disease. It is effective and is not a substitute for being caused by bacteria called Salmonella Typhi. careful about what you eat or drink.) Typhoid causes a high fever, weakness, stomach •People in close contact with a typhoid carrier. pains, headache, loss of appetite, and sometimes a •Laboratory workers who work with Salmonella rash. If it is not treated, it can kill up to 30% of Typhi bacteria. people who get it. Some people who get typhoid become “carriers,” Inactivated Typhoid Vaccine (Shot) who can spread the •Should not be given to children younger than 2 disease to years of age. others. •One dose provides protection. It should be given Generally, at least 2 weeks before travel to allow the vaccine people get time to work. typhoid from contaminated •A booster dose is needed every 2 years for people food or water. Typhoid is not common in the U.S., who remain at risk. and most U.S. citizens who get the disease get it Live Typhoid Vaccine (Oral) while traveling. Typhoid strikes about 21 million people a year around the world and kills about •Should not be given to children younger than 6 200,000. years of age. -

Vaccine for New Mothers
Tdap Vaccine for New Mothers Special Deliveries Childbirth Center at Hartford Hospital Tetanus, Diphtheria, Pertussis (Tdap) What you need to know after the birth of your baby Why get vaccinated? Tdap and related vaccines The Tdap (Tetanus, Diphtheria, Pertussis) vaccine can protect Vaccines for adolescents and adults adolescents and adults against three serious diseases. • Tdap was licensed in 2005. It is the first vaccine for adolescents and adults that protects against all three diseases. Tetanus, Diphtheria, and Pertussis are all caused by bacteria. Diphtheria and Pertussis are spread from person to person. • Td (tetanus and diphtheria) vaccine has been used for many Tetanus enters the body through cuts, scratches, or wounds. years as booster doses for adolescents and adults. It does not contain Pertussis vaccine. Tetanus (Lockjaw) causes painful tightening of the muscles, usually all over the body. • It can lead to “locking” of the jaw so the victim cannot open Why should I get Tdap vaccine after his mouth or swallow. Tetanus leads to death in up to two cases out of ten. the birth of my baby? Infants are at highest risk of complications and death related Diphtheria causes a thick covering in the back of the throat. • to Pertussis when compared to older age groups. Vaccinating • It can lead to breathing problems, paralysis, heart failure, adults who have contact with infants less than 12 months and even death. helps to prevent Pertussis in infants. Pertussis (Whooping Cough) causes severe coughing spells, Adults who expect to have close contact with an infant vomiting, and disturbed sleep. • younger than 12 months of age should get a dose of Tdap. -

Trends in Vaccine Availability and Novel Vaccine Delivery Technologies: 2008–2025
Landscape Analysis Trends in vaccine availability and novel vaccine delivery technologies: 2008–2025 July 2008 Bâtiment Avant Centre Phone: 33.450.28.00.49 13 Chemin du Levant Fax: 33.450.28.04.07 01210 Ferney Voltaire www.path.org France www.who.int Landscape Analysis Trends in vaccine availability and novel vaccine delivery technologies: 2008–2025 July 1, 2008 Version: January 22, 2009 ii Table of contents Acronyms and abbreviations.......................................................................................................................................... iv Executive summary......................................................................................................................................................... 1 TRENDS IN VACCINE AVAILABILITY: 2008–2025 ............................................................................................. 2 Choice of vaccine types to be surveyed........................................................................................................................... 2 Vaccine availability and use: 2008–2025........................................................................................................................ 2 Vaccine availability............................................................................................................................................... 2 Delivery strategies................................................................................................................................................. 4 Extensions -

2021 Medicare Vaccine Coverage Part B Vs Part D
CDPHP® Medicare Advantage Vaccine Coverage Guide Part B (Medical) vs. Part D (Pharmacy) Medicare Part B (Medical): Medicare Part D (Pharmacy): Vaccinations or inoculations Vaccinations or inoculations are included when the administration is (except influenza, pneumococcal, reasonable and necessary for the prevention of illness. and hepatitis B for members at risk) are excluded unless they are directly related to the treatment of an injury or direct exposure to a disease or condition. • Influenza Vaccine (Flu) • BCG Vaccine • Pneumococcal Vaccine • Diphtheria/Tetanus/Acellular Pertussis Vaccine (ADACEL, (Pneumovax, Prevnar 13) BOOSTRIX, DAPTACEL, INFANRIX) • Hepatitis B Vaccine • Diphtheria/Tetanus/Acellular Pertussis/Inactivated Poliovirus (Recombivax, Engerix-B) Vaccine (KINRIX, QUADRACEL) for members at moderate • Diphtheria/Tetanus Vaccine (DT, Td, TDVAX, TENIVAC) to high risk • Diphtheria/Tetanus/Acellular Pertussis/Inactivated Poliovirus Vac • Other vaccines when directly cine/ Haemophilus Influenzae Type B Conjugate Vaccine (PENTACEL) related to the treatment of an • Diphtheria/Tetanus/Acellular Pertussis/Inactivated Poliovirus injury or direct exposure to a Vaccine/Hepatitis B Vaccine (PEDIARIX) disease or condition, such as: • Haemophilus Influenzae Type B Conjugate Vaccine (ActHIB, PedvaxHIB, • Antivenom Sera Hiberix) • Diphtheria/Tetanus Vaccine • Hepatitis A Vaccine, Inactivated (VAQTA) (DT, Td, TDVAX, TENIVAC) • Hepatitis B Vaccine, Recombinant (ENGERIX-B, RECOMBIVAX HB) • Rabies Virus Vaccine for members at low risk (RabAvert, -

Routine Immunizations
Drug and Biologic Coverage Policy Effective Date ............................................... 7/1/2021 Next Review Date ......................................... 4/1/2022 Coverage Policy Number .................................. 9001 Routine Immunizations Table of Contents Related Coverage Resources Coverage Policy ................................................... 1 Preventive Care Services General Background ............................................ 2 Covid-19 Vaccine Coding/Billing Information .................................... 3 References .......................................................... 7 INSTRUCTIONS FOR USE The following Coverage Policy applies to health benefit plans administered by Cigna Companies. Certain Cigna Companies and/or lines of business only provide utilization review services to clients and do not make coverage determinations. References to standard benefit plan language and coverage determinations do not apply to those clients. Coverage Policies are intended to provide guidance in interpreting certain standard benefit plans administered by Cigna Companies. Please note, the terms of a customer’s particular benefit plan document [Group Service Agreement, Evidence of Coverage, Certificate of Coverage, Summary Plan Description (SPD) or similar plan document] may differ significantly from the standard benefit plans upon which these Coverage Policies are based. For example, a customer’s benefit plan document may contain a specific exclusion related to a topic addressed in a Coverage Policy. In the event -
Integration of Typhoid Conjugate Vaccine in National Immunization Schedules: Opportunities and Challenges
Integration of typhoid conjugate vaccine in national immunization schedules: Opportunities and Challenges. Integration of typhoid9th conjugateInternational vaccine Conferencein national immunization on Typhoid schedules: and Opportunities and invasiveChallenges. NTS Disease 30/04 – 3/05, 2015. Nusa Dua, Bali Objective Review the existing clinical data on Vi conjugate vaccines, based on literature and our experience with Typbar-TCV to ascertain data sufficiency to assist global policy formualtion. Presentation Outline • Need for typhoid vaccine – Disease burden • Typhoid conjugate vaccines – Key considerations • Available data from typhoid conjugate vaccines (TCV) • Programmatic considerations • Integration of TCV into childhood immunization programs Typhoid epidemiology Disease Burden This disease is endemic in most developing countries. Cases/100,00 persons Highly Endemic >100 Endemic 10-100 Sporadic <10 21 million cases worldwide, mortality estimates of 216,000 to 600,000. http://www.who.int/immunization/topics/en/ http://www3.chu-rouen.fr/Internet/services/sante_voyages/pathologies/typhoide/ Age stratified disease burden 0.4 0.3 0.2 0.1 0 Proportion of Cases of Proportion Age groups Crump JA, et al. Bull World Health Organ 2004;82:346-353 Typhoid fever incidence – Asia and Africa • High incidence of typhoid fever in the region. • High incidence in urban slums; rates similar • Substantial regional variation in incidence. to those from Asia. • “Modified” Passive srvlnce. • Lower burden in rural children from Ghana (and Lwak, Kenya), compared to urban Ochiai RL, et al. Bull World Health Organ 2008;86:260-268. Breiman, RF et. al, PLoS One. 2012; 7(1): e29119. areas; regional differences Marks, F et. al, Emerg Infect Dis. 2010; 16(11): 1796–1797. -

Ebook Diphtheria Antigen Review 2012.Pdf
2012 Antigen Review for the New Zealand National Immunisation Schedule: Diphtheria Auckland UniServices Limited A wholly owned company of The University of Auckland Prepared for: New Zealand Ministry of Health Prepared by a scientific team incorporating the Immunisation Advisory Centre, The University of Auckland Institute of Environmental Science and Research Ltd. February 2013 Contact details: Helen Petousis-Harris Immunisation Advisory Centre Tāmaki Innovation Campus The University of Auckland Private Bag 92019, Auckland 1142, New Zealand Phone: +64 9 923 2078 Fax: +64 9 373 7030 Mobile: +64 27 471 6749 Email: [email protected] 2 Antigen Review–2012: Diphtheria Executive summary As a result of the introduction of vaccines against diphtheria, the disease is now rare in developed countries. Evidence suggests that the Diphtheria, Tetanus, acellular Pertussis vaccine (DTaP) is safe and well tolerated in infants, toddlers, adolescents and adults. The adult reduced antigen concentration tetanus-diphtheria (Td) is not associated with any safety concerns in 10-64 year olds or in 65+ year olds. Administration of tetanus, diphtheria, acellular pertussis vaccine (Tdap) to pregnant women is not associated with any unexpected safety patterns in maternal, infant, or fetal outcomes. DTaP vaccines have been proven to be highly immunogenic as primary and booster vaccinations. When the primary series is given during the first few years of life, the antibody levels decrease over time with a booster dose being recommended around pre-school/early school and adolescence age. Adults who have received a primary course also require a booster dose at some time during their adulthood. For people who have never had a primary series of diphtheria vaccines as a child, three doses of the adult formulation vaccine has been found to induce an adequate immune response. -

Td Vaccine Can Prevent Tetanus and Diphtheria
VACCINE INFORMATION STATEMENT Many vaccine information statements are available in Spanish and other languages. Td (Tetanus, Diphtheria) Vaccine: See www.immunize.org/vis Hojas de información sobre vacunas están What You Need to Know disponibles en español y en muchos otros idiomas. Visite www.immunize.org/vis 1. Why get vaccinated? 3. Talk with your health care provider Td vaccine can prevent tetanus and diphtheria. Tell your vaccination provider if the person getting Tetanus enters the body through cuts or wounds. the vaccine: Diphtheria spreads from person to person. Has had an allergic reaction after a previous dose TETANUS (T) causes painful stiffening of the of any vaccine that protects against tetanus or muscles. Tetanus can lead to serious health diphtheria, or has any severe, life-threatening problems, including being unable to open the allergies mouth, having trouble swallowing and breathing, Has ever had Guillain-Barré Syndrome (also or death. called “GBS”) DIPHTHERIA (D) can lead to difficulty breathing, Has had severe pain or swelling after a previous heart failure, paralysis, or death. dose of any vaccine that protects against tetanus or diphtheria 2. Td vaccine In some cases, your health care provider may decide to postpone Td vaccination until a future visit. Td is only for children 7 years and older, adolescents, and adults. People with minor illnesses, such as a cold, may be vaccinated. People who are moderately or severely ill Td is usually given as a booster dose every 10 years, should usually wait until they recover before getting or after 5 years in the case of a severe or dirty wound Td vaccine. -

Weekly Epidemiological Record Relevé Épidémiologique Hebdomadaire
2017, 92, 13-20 No 2 Weekly epidemiological record Relevé épidémiologique hebdomadaire 13 JANUARY 2017, 92th YEAR / 13 JANVIER 2017, 92e ANNÉE No 2, 2017, 92, 13–20 http://www.who.int/wer Global Advisory Committee Comité consultatif mondial Contents on Vaccine Safety, pour la sécurité des vaccins, er 13 Global Advisory Committee on 30 November – 1 December 30 novembre - 1 décembre Vaccine Safety, 30 November 2016 2016 – 1 December 2016 The Global Advisory Committee on Le Comité consultatif mondial pour la sécurité Vaccine Safety (GACVS), an independent des vaccins (GACVS) est un organe consultatif Sommaire expert clinical and scientific advisory indépendant composé d’experts cliniques et 13 Comité consultatif mondial body, provides WHO with scientifically scientifiques qui fournissent à l’OMS des pour la sécurité des vaccins, rigorous advice on vaccine safety issues of conseils d’une grande rigueur scientifique sur 30 novembre - 1er décembre potential global importance.1 GACVS held des problèmes de sécurité des vaccins suscep- 2016 its 35th meeting in Geneva, Switzerland, tibles d’avoir une portée mondiale.1 Le GACVS on 30 November and 1 December 2016.2 a tenu sa 35e réunion à Genève (Suisse) les The Committee examined 2 generic issues: 30 novembre et 1er décembre 2016.2 Il a abordé updates on its operations following a 2 questions génériques, avec une mise à jour review conducted in 2014, and progress sur ses activités suite à une analyse réalisée with developing the Vaccine Safety Net. It en 2014 et un aperçu des progrès accomplis also reviewed vaccine-specific safety issues dans la mise en place du Réseau pour la sécu- concerning typhoid vaccines, yellow fever rité des vaccins. -

Combined Hepatitis a Virus (Inactivated) and Typhoid Polysaccharide Vaccine Patient Group Direction (PGD)
PHE publications gateway number: GW-1014 Combined Hepatitis A Virus (Inactivated) and Typhoid Polysaccharide Vaccine Patient Group Direction (PGD) This PGD is for the administration of combined hepatitis A virus (inactivated) and typhoid polysaccharide vaccine (HepA/Typhoid) to individuals considered at risk of exposure to Salmonella enterica serovar typhi, (S. typhi) and hepatitis A virus in accordance with recommendations from the National Travel Health Network and Centre (NaTHNaC). This PGD is for the administration of HepA/Typhoid by registered healthcare practitioners identified in Section 3, subject to any limitations to authorisation detailed in Section 2. Reference no: HepA/Typhoid vaccine PGD Version no: V02.00 Valid from: 01 March 2020 Review date: 01 September 2021 Expiry date: 28 February 2022 Public Health England has developed this PGD to facilitate publicly-funded immunisation in line with national recommendations. Those using this PGD must ensure that it is organisationally authorised and signed in Section 2 by an appropriate authorising person, relating to the class of person by whom the product is to be supplied, in accordance with Human Medicines Regulations 2012 (HMR2012)1. The PGD is not legal or valid without signed authorisation in accordance with HMR2012 Schedule 16 Part 2. Authorising organisations must not alter, amend or add to the clinical content of this document (sections 4, 5 and 6); such action will invalidate the clinical sign-off with which it is provided. In addition authorising organisations must not alter section 3 ‘Characteristics of staff’. Only sections 2 and 7 can be amended within the designated editable fields provided. Operation of this PGD is the responsibility of commissioners and service providers.