Driving Change in Immunisation: the Role of the National Immunisation Office 2005 - 2011
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Vaccine Information for PARENTS and CAREGIVERS
NATIONAL INSTITUTE FOR COMMUNICABLE DISEASES Division of the National Health Laboratory Service VACCINE INFOR MATION FOR PARENTS & CAREGIVERS First Edition November 2016 Editors-in-Chief Nkengafac Villyen Motaze (MD, MSc, PhD fellow), Melinda Suchard (MBBCh, FCPath (SA), MMed) Edited by: Cheryl Cohen, (MBBCh, FCPath (SA) Micro, DTM&H, MSc (Epi), Phd) Lee Baker, (Dip Pharm) Lucille Blumberg, (MBBCh, MMed (Micro) ID (SA) FFTM (RCPS, Glasgow) DTM&H DOH DCH) Published by: Ideas Wise and Wonderful (IWW) for National Institute for Communicable Diseases (NICD) First Edition: Copyright © 2016 Contributions by: Clement Adu-Gyamfi (BSc Hons, MSc), Jayendrie Thaver (BSc), Kerrigan McCarthy, (MBBCh, FCPath (SA), DTM&H, MPhil (Theol) Kirsten Redman (BSc Hons), Nishi Prabdial-Sing (PhD), Nonhlanhla Mbenenge (MBBCh, MMED) Philippa Hime (midwife), Vania Duxbury (BSc Hons), Wayne Howard (BSc Hons) Acknowledgments: Amayeza, Vaccine Information Centre (http://www.amayeza-info.co.za/) Centre for Communicable Diseases Fact Sheets (http://www.cdc.gov/vaccines/hcp/vis/) World Health Organization Fact Sheets (http://www.who.int/mediacentre/factsheets/en/) National Department of Health, South Africa (http://www.health.gov.za/) Disclaimer This book is intended as an educational tool only. Information may be subject to change as schedules or formulations are updated. Summarized and simplified information is presented in this booklet. For full prescribing information and contraindications for vaccinations, please consult individual package inserts. There has been -
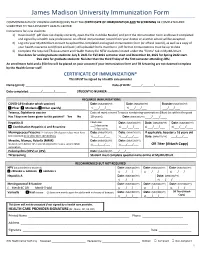
Immunization-Form.Pdf
James Madison University Immunization Form COMMONWEALTH OF VIRGINIA LAW REQUIRES THAT THE CERTIFICATE OF IMMUNIZATION AND TB SCREENING BE COMPLETED AND SUBMITTED TO THE UNIVERSITY HEALTH CENTER. Instructions for new students: 1) Download (if .pdf does not display correctly, open the file in Adobe Reader) and print the Immunization Form and have it completed and signed by a health care professional. An official immunization record from your doctor or another school will be accepted. 2) Log into your MyJMUChart account to upload the completed and signed immunization form (or official record), as well as a copy of your health insurance card (front and back.) All uploaded forms must be in .pdf format. Immunizations must be up to date. 3) Complete the required TB Assessment and Health History for NEW students located under the “forms” tab in MyJMUChart. Due dates for undergraduate students: July 8, 2021 for Fall 2021 semester start and December 10, 2021 for Spring 2022 start. Due date for graduate students: No later than the third Friday of the first semester attending JMU. An enrollment hold and a $50 fine will be placed on your account if your immunization form and TB Screening are not deemed complete by the Health Center staff. CERTIFICATE OF IMMUNIZATION* This MUST be signed by a health care provider Name (print): _______________________________________________ Date of Birth: ______/_______/_______________ Date completed: _______/_______/_______ STUDENT ID NUMBER: __________________________ REQUIRED IMMUNIZATIONS COVID-19 (indicate which -

Vaccine for New Mothers
Tdap Vaccine for New Mothers Special Deliveries Childbirth Center at Hartford Hospital Tetanus, Diphtheria, Pertussis (Tdap) What you need to know after the birth of your baby Why get vaccinated? Tdap and related vaccines The Tdap (Tetanus, Diphtheria, Pertussis) vaccine can protect Vaccines for adolescents and adults adolescents and adults against three serious diseases. • Tdap was licensed in 2005. It is the first vaccine for adolescents and adults that protects against all three diseases. Tetanus, Diphtheria, and Pertussis are all caused by bacteria. Diphtheria and Pertussis are spread from person to person. • Td (tetanus and diphtheria) vaccine has been used for many Tetanus enters the body through cuts, scratches, or wounds. years as booster doses for adolescents and adults. It does not contain Pertussis vaccine. Tetanus (Lockjaw) causes painful tightening of the muscles, usually all over the body. • It can lead to “locking” of the jaw so the victim cannot open Why should I get Tdap vaccine after his mouth or swallow. Tetanus leads to death in up to two cases out of ten. the birth of my baby? Infants are at highest risk of complications and death related Diphtheria causes a thick covering in the back of the throat. • to Pertussis when compared to older age groups. Vaccinating • It can lead to breathing problems, paralysis, heart failure, adults who have contact with infants less than 12 months and even death. helps to prevent Pertussis in infants. Pertussis (Whooping Cough) causes severe coughing spells, Adults who expect to have close contact with an infant vomiting, and disturbed sleep. • younger than 12 months of age should get a dose of Tdap. -

Trends in Vaccine Availability and Novel Vaccine Delivery Technologies: 2008–2025
Landscape Analysis Trends in vaccine availability and novel vaccine delivery technologies: 2008–2025 July 2008 Bâtiment Avant Centre Phone: 33.450.28.00.49 13 Chemin du Levant Fax: 33.450.28.04.07 01210 Ferney Voltaire www.path.org France www.who.int Landscape Analysis Trends in vaccine availability and novel vaccine delivery technologies: 2008–2025 July 1, 2008 Version: January 22, 2009 ii Table of contents Acronyms and abbreviations.......................................................................................................................................... iv Executive summary......................................................................................................................................................... 1 TRENDS IN VACCINE AVAILABILITY: 2008–2025 ............................................................................................. 2 Choice of vaccine types to be surveyed........................................................................................................................... 2 Vaccine availability and use: 2008–2025........................................................................................................................ 2 Vaccine availability............................................................................................................................................... 2 Delivery strategies................................................................................................................................................. 4 Extensions -

Vaccine Adjuvants Derived from Marine Organisms
biomolecules Review Vaccine Adjuvants Derived from Marine Organisms Nina Sanina Department of Biochemistry, Microbiology and Biotechnology, School of Natural Sciences, Far Eastern, Federal University, Sukhanov Str., 8, Vladivostok 690091, Russia; [email protected]; Tel.: +7-423-265-2429 Received: 10 July 2019; Accepted: 1 August 2019; Published: 3 August 2019 Abstract: Vaccine adjuvants help to enhance the immunogenicity of weak antigens. The adjuvant effect of certain substances was noted long ago (the 40s of the last century), and since then a large number of adjuvants belonging to different groups of chemicals have been studied. This review presents research data on the nonspecific action of substances originated from marine organisms, their derivatives and complexes, united by the name ‘adjuvants’. There are covered the mechanisms of their action, safety, as well as the practical use of adjuvants derived from marine hydrobionts in medical immunology and veterinary medicine to create modern vaccines that should be non-toxic and efficient. The present review is intended to briefly describe some important achievements in the use of marine resources to solve this important problem. Keywords: squalene; cucumariosides; chitosan; fucoidans; carrageenans; laminarin; alginate 1. Introduction The oil-in-water-based complete Freund’s adjuvant developed by Jules Freund and Katherine McDermott in 40s of last century is the first vaccine adjuvant. The basis of immune stimulation and provide immunologists with a way to stimulate the production of antibodies and cellular immune responses to weak antigens. This elaboration allowed to establish the basis of immune stimulation and provide immunologists with an instrument to stimulate the production of antibody and cellular immune responses to weak antigens. -

Ebook Diphtheria Antigen Review 2012.Pdf
2012 Antigen Review for the New Zealand National Immunisation Schedule: Diphtheria Auckland UniServices Limited A wholly owned company of The University of Auckland Prepared for: New Zealand Ministry of Health Prepared by a scientific team incorporating the Immunisation Advisory Centre, The University of Auckland Institute of Environmental Science and Research Ltd. February 2013 Contact details: Helen Petousis-Harris Immunisation Advisory Centre Tāmaki Innovation Campus The University of Auckland Private Bag 92019, Auckland 1142, New Zealand Phone: +64 9 923 2078 Fax: +64 9 373 7030 Mobile: +64 27 471 6749 Email: [email protected] 2 Antigen Review–2012: Diphtheria Executive summary As a result of the introduction of vaccines against diphtheria, the disease is now rare in developed countries. Evidence suggests that the Diphtheria, Tetanus, acellular Pertussis vaccine (DTaP) is safe and well tolerated in infants, toddlers, adolescents and adults. The adult reduced antigen concentration tetanus-diphtheria (Td) is not associated with any safety concerns in 10-64 year olds or in 65+ year olds. Administration of tetanus, diphtheria, acellular pertussis vaccine (Tdap) to pregnant women is not associated with any unexpected safety patterns in maternal, infant, or fetal outcomes. DTaP vaccines have been proven to be highly immunogenic as primary and booster vaccinations. When the primary series is given during the first few years of life, the antibody levels decrease over time with a booster dose being recommended around pre-school/early school and adolescence age. Adults who have received a primary course also require a booster dose at some time during their adulthood. For people who have never had a primary series of diphtheria vaccines as a child, three doses of the adult formulation vaccine has been found to induce an adequate immune response. -

Td Vaccine Can Prevent Tetanus and Diphtheria
VACCINE INFORMATION STATEMENT Many vaccine information statements are available in Spanish and other languages. Td (Tetanus, Diphtheria) Vaccine: See www.immunize.org/vis Hojas de información sobre vacunas están What You Need to Know disponibles en español y en muchos otros idiomas. Visite www.immunize.org/vis 1. Why get vaccinated? 3. Talk with your health care provider Td vaccine can prevent tetanus and diphtheria. Tell your vaccination provider if the person getting Tetanus enters the body through cuts or wounds. the vaccine: Diphtheria spreads from person to person. Has had an allergic reaction after a previous dose TETANUS (T) causes painful stiffening of the of any vaccine that protects against tetanus or muscles. Tetanus can lead to serious health diphtheria, or has any severe, life-threatening problems, including being unable to open the allergies mouth, having trouble swallowing and breathing, Has ever had Guillain-Barré Syndrome (also or death. called “GBS”) DIPHTHERIA (D) can lead to difficulty breathing, Has had severe pain or swelling after a previous heart failure, paralysis, or death. dose of any vaccine that protects against tetanus or diphtheria 2. Td vaccine In some cases, your health care provider may decide to postpone Td vaccination until a future visit. Td is only for children 7 years and older, adolescents, and adults. People with minor illnesses, such as a cold, may be vaccinated. People who are moderately or severely ill Td is usually given as a booster dose every 10 years, should usually wait until they recover before getting or after 5 years in the case of a severe or dirty wound Td vaccine. -
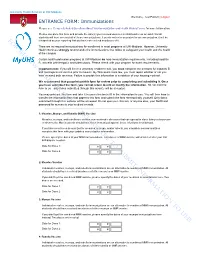
Do Not Use to Submit Information To
University Health Services at UW-Madison Welcome, Test Patient | Logout ENTRANCE FORM: Immunizations Please see Frequently Asked Questions About Your Immunization and Health History Forms for more information. Please complete this form and provide the date(s) you received vaccines in childhood or as an adult. Not all students will have received all of these immunizations. If you do not enter any dates for an immunization, it will be For interpreted as your reporting that you have not received any doses of it. There are no required immunizations for enrollment in most programs at UW-Madison. However, University review Health Services strongly recommends the immunizations that follow to safeguard your health and the health of the campus. Certain health profession programs at UW-Madison do have immunization requirements, including hepatitis B, varicella (chickenpox), and tuberculosis. Please check with your program for exact requirements. purposesImportant note: If you will live in a university residence hall, you must complete the sections for hepatitis B and meningococcal vaccine prior to move-in. By Wisconsin state law, you must report whether or not you have received both vaccines. Failure to provide this information is a violation of your housing contract. We recommend that you print out this form for review prior to completing and submitting it. Once you have submitted the form, you cannot return to add or modify the information. Do not mail the form to us—only forms submitted through this website will be accepted. You may print out onlythis form and take it to your clinician to fill in the information for you. -
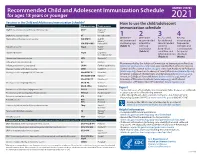
2021 Recommended Child and Adolescent Immunization Schedule
Recommended Child and Adolescent Immunization Schedule UNITED STATES for ages 18 years or younger 2021 Vaccines in the Child and Adolescent Immunization Schedule* How to use the child/adolescent Vaccines Abbreviations Trade names immunization schedule Diphtheria, tetanus, and acellular pertussis vaccine DTaP Daptacel® Infanrix® Diphtheria, tetanus vaccine DT No trade name 1 2 3 4 Haemophilus influenzae type b vaccine Hib (PRP-T) ActHIB® Determine Determine Assess need Review Hiberix® recommended recommended for additional vaccine types, Hib (PRP-OMP) PedvaxHIB® vaccine by age interval for recommended frequencies, Hepatitis A vaccine HepA Havrix® (Table 1) catch-up vaccines intervals, and Vaqta® vaccination by medical considerations (Table 2) condition and for special Hepatitis B vaccine HepB Engerix-B® Recombivax HB® other indications situations (Table 3) (Notes) Human papillomavirus vaccine HPV Gardasil 9® Influenza vaccine (inactivated) IIV Multiple Recommended by the Advisory Committee on Immunization Practices Influenza vaccine (live, attenuated) LAIV4 FluMist® Quadrivalent (www.cdc.gov/vaccines/acip) and approved by the Centers for Disease Measles, mumps, and rubella vaccine MMR M-M-R II® Control and Prevention (www.cdc.gov), American Academy of Pediatrics Meningococcal serogroups A, C, W, Y vaccine MenACWY-D Menactra® (www.aap.org), American Academy of Family Physicians (www.aafp.org), American College of Obstetricians and Gynecologists (www.acog.org), MenACWY-CRM Menveo® American College of Nurse-Midwives (www.midwife.org), American -

Control of Diphtheria, Pertussis, Tetanus, Haemoph1lus Influenzae
Scientific and Technical Publication No. 604 Control of Diphtheria, Pertussis, Tetanus, Haemoph1lus influenzae type b and Hepatitis B Field Guide (4\kEQo CONTROL OF DIPHTHERIA ) PERTUSSIS, TETANUS, HAEMOPHILUS INFLUENZAE TYPE B, AN D H E PATITIs B FIELD GUIDE Pan American Health Organization Regional Office of the ir6 .lI" World Health Organization Scientific and Technical Publication No. 604 PAN AMERICAN HEALTH ORGANIZATION Pan American Sanitary Burean, Regional Office of the WORLD HEALTH ORGANIZATION 525 Twenty-third Street, N,W, Washington, D.C. 20037 www.paho.org 2005 Also published in Spanish (2005) with the title: Control de la difteria, tos ferina, tétanos, Haemophi/us ¡rifluenzae tipo 6y hepatitis B. Guía práctica. (ISBN 92 75 31604 X) PAHO HQ Li brary Cataloguing-in-Publication Data Pan American Health Organization Control ofdiphtheria, pertussis, tetanus, Haemophilus ¡nfluenzae iype b, and hepatitis B: fleId guide. Washington, D.C.: PAHO, © 2005. (Scientific and Technical Publication No. 604) ISBN 9275 116040 1. Title II. Series 1. DIPHTHER1A - prevention & control 2. WHOOPING COUGH - prevention & control 3. TETANUS - prevention & control 4. HAEMOPHILUS INFLUENZAETYPE B S. HEPATITIS B - prevention & control 6. GUIDEBOOKS [PUBLICATION TYPE! NLM WC100 This guide was prepared by the Immunization Unit of the Pan American Health Organization. Cover photos: left, Stockbyte.com, © Stockbyte; center, courtesy of Ignacio Astorga; right, Stockbyte.com, © Stockbyte. The Pan American Health Organization welcomes requests for permission to reproduce or translate its publications, in part or in fuIl. Applications and inquines should be addressed to the Publications Program, Pan American Health Organization, Washington, D.C., U.S.A., which wilI be glad to provide the latest information on any changes made co the text, plans for new editions, and reprints and translations already available. -

(Tdap) Vaccine
Updated March 2016 For further information contact IPAC: Immunization Practices Advisory Council Maggie June • 505-272-3032 • [email protected] Tetanus, Diphtheria, Acellular Pertussis (Tdap) Vaccine IPAC and the New Mexico Immunization Coalition urge all medical practices and health professionals to offer Tdap booster immunization against pertussis in place of Tetanus Diphtheria vaccine or Tetanus Toxoid to adolescents and adults if that person has not previously received Tdap. Pertussis infection has been on the rise for the past 20 years and much of the increase has been in teens and young adults. Most reported pertussis cases among adolescents and adults occur because protective immunity against pertussis decreases within five to ten years of the last childhood vaccination. In both adults and adolescents, pertussis may cause severe and prolonged coughing, as well as vomiting, interrupted sleep, cyanosis, pneumonia, fractured ribs and hospitalizations. Adults and adolescents are capable of spreading the infection to vulnerable populations, particularly infants who are too young to have been fully immunized. 75% of infants with pertussis are infected by a close family member—almost half are infected by their mother or father. Who should receive Tdap? Giving Tdap with other vaccines Adolescents and adults in need of Td booster if they Tdap can conveniently and safely be given with other have never previously received Tdap should receive a vaccines. It is recommended (ACIP, AAFP, and AAP) to single dose of Tdap. be given with the other vaccines for 11‐12 year olds— There is no minimum interval between previous Td or TT the Human Papillomavirus (HPV) Vaccine and the and Tdap. -

A Quick Look at Using Td (Tetanus, Diphtheria) Vaccine
A Quick Look at Using Td (Tetanus, diphtheria) Vaccine Use Td for: · Persons 7 years and older Vaccine Administration · Anyone who has previously received a Tdap vaccine · Intramuscular (IM) injection in the deltoid of the arm · Pregnant adolescents and women* · 1-1.5 inch, 22-25 gauge needle · Person with a contraindication to pertussis vaccine · Professional judgment is appropriate when selecting needle length Schedule: · Can be given simultaneously with other vaccines · Routine Schedule: Booster dose every 10 years Catch-Up Schedule: Storage and Handling · 3 doses (primary series) of tetanus & diphtheria-containing Store in the refrigerator between vaccine are needed before a booster dose is effective · 35º-46º F (2º-8ºC) - Dose 1 to 2 4 weeks · Do NOT freeze - Dose 2 to 3 varies** Keep in the original box Td **8 weeks if 1st dose given at less than 12 months of age · Shake well before use **6 months if 1st dose given at 12 months of age and older · WOUND CARE • Administer Td to persons with a wound that is not clean and/or not minor and it has been 5 years since the last dose of tetanus containing vaccine if they are: - 7-9 years of age (Tdap may be used if there is an additional indication for a pertussis-containing vaccine***) - 10-64 years of age & have received a previous dose of Tdap vaccine - 65 years of age and older (Tdap may be used if there is an additional indication for a pertussis-containing vaccine***) • If Tdap vaccine is indicated but not available, use Td vaccine CONTRAINDICATIONS • Allergic reaction to a previous