Guidelines for Essential Trauma Care
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Arizona Guidelines for Field Triage of Injured Patients (Regional Modifications Are Permissible)
Arizona Guidelines for Field Triage of Injured Patients (Regional modifications are permissible) FIELD TRIAGE DECISION SCHEME Measure vital signs and level of consciousness Glasgow Coma Scale ≤13 Systolic blood pressure (mmHg) <90 mmHg Step One Respiratory rate <10 or >29 breaths per minute (<20 in infant aged < 1 year1), or need for ventilator support YES NO Transport to a Trauma Center2. Steps 1 and 2 attempt to identify the most seriously injured Assess anatomy of injury. patients. These patients should be transported preferentially to the highest level of care within the trauma system. • All penetrating injuries to head, neck, torso, and extremities proximal to elbow or knee • Chest wall instability or deformity (e.g., flail chest) • Two or more proximal long-bone fractures • Crushed, de-gloved, mangled, or pulseless extremity Step Two3 • Amputation proximal to wrist or ankle • Pelvic fractures • Open or depressed skull fracture • Paralysis YES NO Transport to a Trauma Center2. Steps 1 and 2 attempt to identify the most seriously injured Assess mechanism of injury patients. These patients should be transported preferentially to the highest level of care within the and evidence of high-energy trauma system. impact. • Falls o Adults: >20 feet (one story is equal to 10 feet) 4 o Children : >10 feet or two or three times the height of the child • High-risk auto crash 5 Intrusion , including roof: >12 inches occupant site; >18 inches any site Step Three3 o o Ejection (partial or complete) from automobile o Death in same passenger compartment o Vehicle telemetry data consistent with high risk of injury 6 • Auto vs. -

Recognizing When a Child's Injury Or Illness Is Caused by Abuse
U.S. Department of Justice Office of Justice Programs Office of Juvenile Justice and Delinquency Prevention Recognizing When a Child’s Injury or Illness Is Caused by Abuse PORTABLE GUIDE TO INVESTIGATING CHILD ABUSE U.S. Department of Justice Office of Justice Programs 810 Seventh Street NW. Washington, DC 20531 Eric H. Holder, Jr. Attorney General Karol V. Mason Assistant Attorney General Robert L. Listenbee Administrator Office of Juvenile Justice and Delinquency Prevention Office of Justice Programs Innovation • Partnerships • Safer Neighborhoods www.ojp.usdoj.gov Office of Juvenile Justice and Delinquency Prevention www.ojjdp.gov The Office of Juvenile Justice and Delinquency Prevention is a component of the Office of Justice Programs, which also includes the Bureau of Justice Assistance; the Bureau of Justice Statistics; the National Institute of Justice; the Office for Victims of Crime; and the Office of Sex Offender Sentencing, Monitoring, Apprehending, Registering, and Tracking. Recognizing When a Child’s Injury or Illness Is Caused by Abuse PORTABLE GUIDE TO INVESTIGATING CHILD ABUSE NCJ 243908 JULY 2014 Contents Could This Be Child Abuse? ..............................................................................................1 Caretaker Assessment ......................................................................................................2 Injury Assessment ............................................................................................................4 Ruling Out a Natural Phenomenon or Medical Conditions -
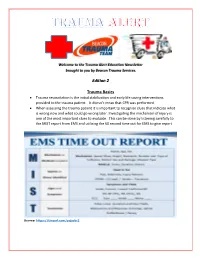
Edition 2 Trauma Basics
Welcome to the Trauma Alert Education Newsletter brought to you by Beacon Trauma Services. Edition 2 Trauma Basics Trauma resuscitation is the initial stabilization and early life saving interventions provided to the trauma patient. It doesn’t mean that CPR was performed. When assessing the trauma patient it is important to recognize clues that indicate what is wrong now and what could go wrong later. Investigating the mechanism of injury is one of the most important clues to evaluate. This can be done by listening carefully to the MIST report from EMS and utilizing the 60 second time out for EMS to give report Source: https://tinyurl.com/ycjssbr3 What is wrong with me? EMS MIST 43 year old male M= unrestrained driver, while texting drove off road at 40 mph into a tree, with impact to driver’s door, 20 minute extrication time I= Deformity to left femur, pain to left chest, skin pink and warm S= B/P- 110/72, HR- 128 normal sinus, RR- 28, Spo2- 94% GCS=14 (Eyes= 4 Verbal= 4 Motor= 6) T= rigid cervical collar, IV Normal Saline at controlled rate, splint left femur What are your concerns? (think about the mechanism and the EMS report), what would you prepare prior to the patient arriving? Ten minutes after arrival in the emergency department the patient starts to have shortness of breath with stridorous sound. He is now diaphoretic and pale. B/P- 80/40, HR- 140, RR- 36 labored. Absent breath sounds on the left. What is the patients’ underlying problem?- Answer later in the newsletter Excellence in Trauma Nursing Award Awarded in May for National Trauma Month This year the nominations were very close so we chose one overall winner and two honorable mentions. -

Incidence, Risk Factors and Management of Severe Post-Transsphenoidal Epistaxis Q ⇑ Kenneth M
Journal of Clinical Neuroscience 22 (2015) 116–122 Contents lists available at ScienceDirect Journal of Clinical Neuroscience journal homepage: www.elsevier.com/locate/jocn Clinical Study Incidence, risk factors and management of severe post-transsphenoidal epistaxis q ⇑ Kenneth M. De Los Reyes a, Bradley A. Gross a, , Kai U. Frerichs a, Ian F. Dunn a, Ning Lin a, Jordina Rincon-Torroella a, Donald J. Annino b, Edward R. Laws a a Department of Neurological Surgery, Brigham and Women’s Hospital and Harvard Medical School, 75 Francis Street, Boston, MA, 02115, USA b Department of Otolaryngology, Brigham and Women’s Hospital and Harvard Medical School, Boston, MA, USA article info abstract Article history: Among the major complications of transsphenoidal surgery, less attention has been given to severe post- Received 16 June 2014 operative epistaxis, which can lead to devastating consequences. In this study, we reviewed 551 consec- Accepted 2 July 2014 utive patients treated over a 4 year period by the senior author to evaluate the incidence, risk factors, etiology and management of immediate and delayed post-transsphenoidal epistaxis. Eighteen patients (3.3%) developed significant postoperative epistaxis – six immediately and 12 delayed (mean postoper- Keywords: ative day 10.8). Fourteen patients harbored macroadenomas (78%) and 11 of 18 (61.1%) had complex Endoscopic nasal/sphenoid anatomy. In the immediate epistaxis group, 33% had acute postoperative hypertension. Epistaxis In the delayed group, one had an anterior ethmoidal pseudoaneurysm, and one had restarted anticoagu- Management Microscopic lation on postoperative day 3. We treated the immediate epistaxis group with bedside nasal packing fol- Pituitary lowed by operative re-exploration if conservative measures were unsuccessful. -

National Referral Facility State-Of-The-Art Teaching Hospital in Central Haiti Hospital Dr
“For some of us, this hospital is the culmination of a dream dating back a quarter century, and underlines our commitment to the country and people of Haiti, which is 2010 stronger than ever after the earthquake.” – Dr. Paul Farmer Mirebalais National Referral Facility State-of-the-Art Teaching Hospital in Central Haiti Hospital Dr. Paul Farmer, co-founder of PIH, Chair of the Harvard Medical School’s Department of Global Health and Social Medicine and Chief of the Division of Global Health Equity at Brigham and Women’s Hospital in Boston, says of the facility, “For some of us, this hospital is the culmination of a dream dating back a quarter century, and underlines our commitment to the country and Mirebalais Hospital Mirebalais Hospital background people of Haiti, which is stronger than ever after National Referral Facility, State-of-the-Art Before the earthquake hit Haiti on January 12, 2010, the town of Mirebalais, located at the intersection of the earthquake. It is also a manifestation of our Teaching Hospital in Central Haiti two main roads in Central Haiti, was the hub of a catchment area with a population of more than 140,000 residents. These two roads have been major thoroughfares for earthquake refugees fleeing Port-au-Prince in integrated model of research, teaching and service, In Haiti, an impoverished country of almost 9 million people with search of new places to call home. Due to its high-traffic location, an estimated 20,000 new residents have the worst basic health indicators and highest rates of extreme and will serve as a site for all three. -

Hospitalists in Teaching Hospitals: Opportunities but Not Without Danger
HospitalistsORIGINALBlackwellEditorials Publishing, ARTICLE Ltd. in Teaching Hospitals: Opportunities but Not Without Danger One thing seems clear: hospitalists do not appear to be have developed or are developing such a “hospitalist-only” going away. After Wachter and Goldman first used the term service. hospitalist to describe a new type of U.S. physician 8 years What about the hospitalist educator’s role within ago,1 the concept of hospital medicine was not warmly teaching hospitals? The study by Kulaga et al.7 in this issue embraced by all.2–4 Even at the 1999 Society of General of the Journal of General Internal Medicine sheds light on Internal Medicine’s 22nd annual meeting in San Francisco, this issue. The authors found that hiring two hospitalist more than a few boos were heard when the topic of hos- educators at their community-based teaching hospital led pitalists came up. Hospital medicine is now one of the fast- to decreased resource utilization and improved resident est growing medical “specialties” in the United States. The education when compared to having private physicians Society of Hospital Medicine, the national organization that manage hospitalized patients.7 Enhanced efficiency due represents hospitalists, boasts upward of 3,500 members. to hospitalists has been demonstrated in several previous The number of want ads in the New England Journal of studies, in both community and academic settings.8 The Medicine and Annals of Internal Medicine for hospitalists finding of an educational benefit for hospitalists in a com- rivals those for primary care-based internists. Medical resi- munity teaching hospital, however, is relatively new. -

Title: ED Trauma: Trauma Nurse Clinical Resuscitation
Title: ED Trauma: Trauma Nurse Clinical Resuscitation Document Category: Clinical Document Type: Policy Department/Committee Owner: Practice Council Original Date: Approved By (last review): Director of Emergency Services, Approval Date: 07/28/2014 Trauma Medical Director, Medical Director Emergency (Complete history at end of document.) Services POLICY: To provide immediate, effective and efficient patient care to the trauma patient, designated nursing staff will respond to the trauma room when a trauma page is received. TRAUMA CONTROL NURSE: 1) Role: a) The trauma control nurse (TCN) is a registered nurse (RN) with specialized training in the care of the traumatized patient, and who will function as the trauma team’s lead nurse. b) The TCN shall have successfully completed the Trauma Nurse Core Course (TNCC), Advanced Cardiac Life Support (ACLS), Emergency Nurse Pediatric Course (ENPC) or Pediatric Advanced Life Support (PALS), and role orientation with trauma services. c) Full-time employee or regularly scheduled part-time Emergency Department (ED) nurse. d) RN must have 6 months of LMH ED experience. 2) Trauma Control Duties: a) Inspects and stocks trauma room at beginning of each shift and after each trauma patient is discharged from the ED. b) Attempts to maintain trauma room temperature at 80-82 degrees Fahrenheit. c) Communicates with pre-hospital personnel to obtain patient information and prior field treatment and response. d) Makes determination that a patient meets Type I or Type II criteria and immediately notifies LMH’s Call System to initiate the Trauma Activation System. e) Assists physician with orders as directed. f) Acts as liaison with patient’s family/law enforcement/emergency medical services (EMS)/flight crews. -
Thoracic and Abdominal Trauma
INJURIESINJURIES TOTO THETHE TRUNKTRUNK THROACIC AND ABDOMINAL INJURIES INITIALINITIAL ASSESSMENTASSESSMENT 1. PRIMARY SURVEY (1. MIN) 2. VITAL FUNCTIONS TREAT LIFE THREATENING FIRST 3. SECONDARY SURVEY 4. DEFINITIVE CARE A.B.C.D.E. LIFELIFE THREATENINGTHREATENING INJURIESINJURIES A. INJURIES TO THE AIRWAYS B. TENSION PTX SUCKING CHEST WOUND MASSIVE HEMOTHORAX FLAIL CHEST C. CARDIAC TAMPONADE MASSIVE HEMOTHORAX LIFELIFE THREATENINGTHREATENING CHESTCHEST INJURIESINJURIES •PNEUMOTHORAX •HEMOTHORAX •PULMONARY CONTUSION •TRACHEBRONCHIAL TREE INJURY •BLUNT CARDIAC INJURY •TRAUMATIC AORTIC INJURY •TRAMATIC DIAPHRAGMATIG INJURY •MEDIASTINAL TRANSVERSING WOUNDS PNEUMOTHORAXPNEUMOTHORAX AIR BETWEEN THE PARIETAL AND VISCERAL PLEURA RIB FRACTURES INJURIES TO THE LUNG INJURIES TO THE AIRWAYS BULLAS IATROGENIG FROM THE RETROPERITONEUM PNEUMOTHORAXPNEUMOTHORAX 1. 2. TENSIONTENSION PNEUMOTHORAXPNEUMOTHORAX ONE WAY VALVE – AIR FROM THE LUNG OR THROUGH THE CHEST WALL INTO THE THORACIC CAVITY CONSEQUENCE: HYPOXIA, BLOCKING OF THE VENOUS INFLOW CHEST PAIN, AIR HUNGER, HYPOTENSION, NECK VEIN DISTENSION, TACHYCARDIA CARDIAC TAMPONADE – NO BREATH SOUNDS IMMEDIATE TREATMENT TENSIONTENSION PNEUMOTHORAXPNEUMOTHORAX TENSION PTX NEEDLE THORACOCENTESIS HEMOTHORAXHEMOTHORAX BLOOD IN THE THORACIC CAVITY LUNG LACERATION RIB FRACTURE INTERCOSTAL VESSEL INJURY ART. MAMMARY INJURY PENETRATING OR BLUNT INJURY HEMOTHORAXHEMOTHORAX 1. ? 2. ! HTXHTX HEMOTHORAXHEMOTHORAX TREATMENT : CHEST TUBE – THORACOTOMY IS RARELY INDICATED THORACOTOMY: 1500 ML / DRAINAGE OR 200 ML/ HOUR -

Anesthesia for Trauma
Anesthesia for Trauma Maribeth Massie, CRNA, MS Staff Nurse Anesthetist, The Johns Hopkins Hospital Assistant Professor/Assistant Program Director Columbia University School of Nursing Program in Nurse Anesthesia OVERVIEW • “It’s not the speed which kills, it’s the sudden stop” Epidemiology of Trauma • ~8% worldwide death rate • Leading cause of death in Americans from 1- 45 years of age • MVC’s leading cause of death • Blunt > penetrating • Often drug abusers, acutely intoxicated, HIV and Hepatitis carriers Epidemiology of Trauma • “Golden Hour” – First hour after injury – 50% of patients die within the first seconds to minutesÆ extent of injuries – 30% of patients die in next few hoursÆ major hemorrhage – Rest may die in weeks Æ sepsis, MOSF Pre-hospital Care • ABC’S – Initial assessment and BLS in trauma – GO TEAM: role of CRNA’s at Maryland Shock Trauma Center • Resuscitation • Reduction of fractures • Extrication of trapped victims • Amputation • Uncooperative patients Initial Management Plan • Airway maintenance with cervical spine protection • Breathing: ventilation and oxygenation • Circulation with hemorrhage control • Disability • Exposure Initial Assessment • Primary Survey: – AIRWAY • ALWAYS ASSUME A CERVICAL SPINE INJURY EXISTS UNTIL PROVEN OTHERWISE • Provide MANUAL IN-LINE NECK STABILIZATION • Jaw-thrust maneuver Initial Assessment • Airway cont’d: – Cervical spine evaluation • Cross table lateral and swimmer’s view Xray • Need to see all seven cervical vertebrae • Only negative CT scan R/O injury Initial Assessment • Cervical -

World Journal of Hepatology
World Journal of W J H Hepatology Submit a Manuscript: https://www.f6publishing.com World J Hepatol 2020 June 27; 12(6): 288-297 DOI: 10.4254/wjh.v12.i6.288 ISSN 1948-5182 (online) ORIGINAL ARTICLE Retrospective Cohort Study Hospital teaching status on the outcomes of patients with esophageal variceal bleeding in the United States Pavan Patel, Laura Rotundo, Evan Orosz, Faiz Afridi, Nikolaos Pyrsopoulos ORCID number: Pavan Patel Pavan Patel, Faiz Afridi, Nikolaos Pyrsopoulos, Division of Gastroenterology and Hepatology, (0000-0001-5682-4939); Laura Rutgers - New Jersey Medical School, Newark, NJ 07101-1709, United States Rotundo (0000-0002-4094-3682); Evan Orosz (0000-0003-2474-5501); Laura Rotundo, Evan Orosz, Department of Medicine, Rutgers - New Jersey Medical School, Faiz Afridi (0000-0002-0172-0486); Newark, NJ 07101-1709, United States Nikolaos Pyrsopoulos (0000-0002-6950-8174). Corresponding author: Nikolaos Pyrsopoulos, FACP, MD, PhD, Chief Doctor, Professor, Division of Gastroenterology and Hepatology, Rutgers – New Jersey Medical School, 185 S. Author contributions: Patel P Orange Avenue, MSB H-535, Newark, NJ 07101-1709, United States. provided conception and design of [email protected] the study, acquisition and analysis of data, and drafting of the manuscript; Rotundo L, Afridi F and Orosz E drafted the manuscript; Pyrsopoulos N Abstract contributed to the manuscript by BACKGROUND providing revision and oversight Acute variceal bleeding is a major complication of portal hypertension and is a of its writing. leading cause of death in patients with cirrhosis. There is limited data on the Institutional review board outcomes of patients with esophageal variceal bleeding in teaching versus statement: This study did not nonteaching hospitals. -

A BRI H IEF HISTO Howard R. C ORY of TH the Champion, K HE
A BRIEF HISTORY OF THE FOUNDING OF THE EASTERN ASSOCIATION FOR THE SURGERY OF TRAUMA (EAST) Howard R. Champion, Kimball I. Maull, Lenworth M. Jacobs, Burton H. Harris A BRIEF HISTORY OF THE FOUNDING OF THE EASTERN ASSOCIATION FOR THE SURGERY OF TRAUMA (EAST) Howard R. Champion, Kimball I. Maull, Lenworth M. Jacobs, Burton H. Harris The Eastern Association for the Surgery of Trauma (EAST) was founded by a group of surgeons each of whom had somewhat established themselves in the field of trauma and surgical critical care by the early 1980s and were in the process of developing these disciplines and mentoring young surgeons. EAST has widely exceeded the original aspirations of that group of then-young surgeons. To understand why EAST was created and why it succeeded, it is necessary to glance back to the mid 1980s. The notion of EAST occurred in 1985 within a context of a growing demand for organized trauma care but no appropriate opportunities for young aspiring trauma surgeons to exchange knowledge, discuss advances in patient care, or develop their careers in this field within the discipline of surgery. No vehicle adequately nurtured young surgeons into the field of trauma. Today, EAST is an established and respected surgical organization reaching its 25-year mark with membership (Figure 1) of 1363 now exceeding that of the premier global trauma organization, the American Association for the Surgery of Trauma (AAST) (1227 members). Then The world of the young trauma surgeon in the early to mid 1980s was a very different place than it is more than 25 years later. -

Management of Acute Liver Failure In
Management of Acute Liver Failure in ICU Philip Berry MRCP, Clinical Research Fellow, Institute of Liver Studies, Kings College Hospital, London, UK Email: [email protected] Self assessment questions Scenario: A twenty-year-old female is brought into the Emergency Department having been found unconscious in her bedsit. There is no other recent history. She did not respond to a bolus of 50% dextrose in the ambulance, despite having an unrecordable blood glucose when tested by the paramedics. While she is being intubated on account of reduced level of consciousness, an arterial blood gas sample reveals profound lactic acidosis (pH 7.05, pCO2 2.5 kPa, base deficit – 10, lactate 13 mg/L). Blood pressure is 95/50 mmHg. 1. What are the possible explanations for her presentation? Laboratory tests demonstrate hepatocellular necrosis (AST 21,000 U/L) and coagulopathy (INR 9.1) with thrombocytopenia (platelet count 26 x 109/L). Acute liver failure appears the most likely diagnosis. 2. What are the most likely causes of acute liver failure (ALF) in this previously well patient? Her mean arterial blood pressure remains low (50mmHg) after 3 litres of colloid and crystalloid. The casualty nurse, who is doing half-hourly neurological observations, reports reduced pupillary response to light. 3. What severe complications of ALF may result in death within hours, and what are the immediate management priorities for this patient? Introduction Successful management of this rare but potentially devastating disorder relies on early recognition. The hallmark of acute liver failure (ALF) is encephalopathy (ranging from a subtle alterations in consciousness level to coma) in the context of an acute, severe liver injury.