Profiling the Effects of Rifaximin on the Healthy Human Colonic Microbiota Using A
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Antibiotic Treatment in Inflammatory Bowel Disease: Rifaximin, a New Possible Approach
European Review for Medical and Pharmacological Sciences 1999; 3: 27-30 Review – Antibiotic treatment in inflammatory bowel disease: rifaximin, a new possible approach P. GIONCHETTI, F. RIZZELLO, A. VENTURI, F. UGOLINI*, M. ROSSI**, P. BRIGIDI**, R. JOHANSSON, A. FERRIERI***, G. POGGIOLI*, M. CAMPIERI Clinica Medica I, Nuove Patologie, Bologna University (Italy) *Istituto di Clinica Chirurgica II, Bologna University (Italy) **Dipartimento di Scienze Farmaceutiche, Bologna University (Italy) ***Direzione Medica Alfa Wassermann, Bologna (Italy) Abstract. – The etiology of inflammatory ported the presence of a breakdown of toler- disease is still unknown, but a body of evidence ance to the normal commensal intestinal flora from clinical and experimental observation indi- in active IBD2-3. Reduction of microflora by cates a role for intestinal microflora in the pathogenesis of this disease. Reduction of mi- antibiotics, bowel rest and fecal diversion de- croflora using antibiotics, bowel rest and fecal creases inflammatory activity in Crohn’s dis- diversion decreases activity in Crohn’s disease ease and to a lesser extent in ulcerative colitis and in ulcerative colitis. Several trials have been (UC). The pathogenetic role of intestinal mi- carried out on the use of antibiotic treatment in croflora is further suggested by the observa- patients with active ulcerative colitis with con- tion that experimental colitis, in germ-free or trasting results. A number of trials have been antibiotic treated animals, is less severe com- carried out using Rifaximin, a non-absorbable broad-spectrum antibiotic, confirming the ab- pared to that inducible in normal animals or sence of systemic bioavalaibility of the drug at times is not inducible at all. -

FDA Warns About an Increased Risk of Serious Pancreatitis with Irritable Bowel Drug Viberzi (Eluxadoline) in Patients Without a Gallbladder
FDA warns about an increased risk of serious pancreatitis with irritable bowel drug Viberzi (eluxadoline) in patients without a gallbladder Safety Announcement [03-15-2017] The U.S. Food and Drug Administration (FDA) is warning that Viberzi (eluxadoline), a medicine used to treat irritable bowel syndrome with diarrhea (IBS-D), should not be used in patients who do not have a gallbladder. An FDA review found these patients have an increased risk of developing serious pancreatitis that could result in hospitalization or death. Pancreatitis may be caused by spasm of a certain digestive system muscle in the small intestine. As a result, we are working with the Viberzi manufacturer, Allergan, to address these safety concerns. Patients should talk to your health care professional about how to control your symptoms of irritable bowel syndrome with diarrhea (IBS-D), particularly if you do not have a gallbladder. The gallbladder is an organ that stores bile, one of the body’s digestive juices that helps in the digestion of fat. Stop taking Viberzi right away and get emergency medical care if you develop new or worsening stomach-area or abdomen pain, or pain in the upper right side of your stomach-area or abdomen that may move to your back or shoulder. This pain may occur with nausea and vomiting. These may be symptoms of pancreatitis, an inflammation of the pancreas, an organ important in digestion; or spasm of the sphincter of Oddi, a muscular valve in the small intestine that controls the flow of digestive juices to the gut. Health care professionals should not prescribe Viberzi in patients who do not have a gallbladder and should consider alternative treatment options in these patients. -
Formulary Additions
JUNE 2016 FORMULARY ADDITIONS MELOXICAM (MOBIC®) Rationale for Addition: Meloxicam is a once daily NSAID used for the treatment of rheumatoid arthritis and osteoarthritis. Meloxicam will provide another oral NSAID option to Celecoxib for patients who are being discharged home and whose insurance does not cover celecoxib. Adverse Effects: abdominal pain, diarrhea, dyspepsia, flatulence, nausea, edema, influenza-like symptoms, dizziness, headache, rash Contraindications: peri-operative pain in setting of coronary artery bypass graft surgery Drug Interactions: other NSAIDS, antiplatelet agents, calcium polysterene sulfonate, cyclosporine, digoxin, lithium, methotrexate, vancomycin, vitamin K antagonist, corticosteroids Dosage & Administration: meloxicam 7.5 mg PO daily, some patients my experience some benefit by increasing to 15 mg PO daily Renal Impairment: not recommended in patients with renal function ≤ 20 mL/min Dosage Form & Cost: meloxicam 7.5 mg tablet $0.02/day meloxicam 15 mg $0.03/day IVABRADINE (CORLANOR®) *Restrictions*: restricted to cardiology only for initiation of therapy Rationale for Addition: Ivabradine blocks the funny current leading to a reduction in heart rate at the sinoatrial node. Ivabradine is indicated to reduce the risk of hospitalization for worsening heart failure in patients with stable symptomatic chronic heart failure with LVEF ≤ 35% who are in sinus rhythm with resting heart rate (HR) ≥ 70 beats per minute and either on maximally tolerated doses of β-blockers or have a contraindication to β-blockers. -

Rifaximin (XIFAXAN)
Rifaximin (XIFAXAN) for Irritable Bowel Syndrome with Diarrhea National Drug Monograph March 2016 VA Pharmacy Benefits Management Services, Medical Advisory Panel, and VISN Pharmacist Executives The purpose of VA PBM Services drug monographs is to provide a focused drug review for making formulary decisions. Updates will be made when new clinical data warrant additional formulary discussion. Documents will be placed in the Archive section when the information is deemed to be no longer current. FDA Approval Information Description/Mechanism of Minimally absorbed, broad-spectrum antibacterial that inhibits bacterial RNA Action synthesis. The specific mechanism of action of rifaximin in irritable bowel syndrome (IBS) has not been determined. The most likely mechanism of rifaximin is reduction in overall bacterial load, particularly in the large bowel1; however, rifaximin also seems to modulate gut microenvironment and produce cytoprotective effects.2 Indication(s) Under Review in Treatment of IBS with diarrhea (IBS-D) in adults this Document Dosage Form(s) Under 550 mg tablet Review REMS REMS No REMS Postmarketing Requirements Pregnancy Rating No data available on pregnant women to inform any drug associated risks. Executive Summary Efficacy Rifaximin had a small, statistically significant beneficial effect relative to placebo in global IBS symptom response using pooled data: 40.7% vs. 31.7%, with a difference of 9.0 percentage points, p < 0.001; NNT = 11. Rifaximin had a small, statistically significant beneficial effect relative to placebo in terms of the response rate for adequate relief of bloating (the key secondary efficacy measure): 40.2% vs. 30.3%, difference of 9.9 percentage points, p < 0.001; NNT = 10 (pooled results). -
What's New with ADHD?
winter 2020 | volume 34 | issue 1 A journal of Dayton Children’s Hospital what’s new with ADHD? by Mollie Walton, MD and Craig Boreman, MD 1 learning objectives recommended (CPG) and the 2011 behavioral rating scales revision, the AAP Following the completion of this article, to help establish the collaborated with the reader should be able to: diagnosis, and outlined several organizations 1. Utilize the updated clinical practice standards for follow-up to form an ADHD guideline for diagnosis and treatment and monitoring.12 The subcommittee un- of ADHD. guidelines were revised der the oversight of 2. Describe the approach to the evaluation in 2011 and published the AAP Council on and treatment of ADHD in the primary with an accompany- Quality Improvement practice setting. ing process of care and Patient Safety.13 3. Give examples of co-existing conditions algorithm (PoCA). The This subcommittee’s associated with ADHD. major change with this membership included revision was the appli- representation of a cable age for diagnosis wide range of primary Attention-deficit/ toms tend to persist.1, 2 and treatment, previ- care and subspecial- hyperactivity Learning and language ously 6-12 years of age, ty groups. The group difficulties are common and was broadened met over a 3.5-year disorder (ADHD) comorbid conditions to include age 4- to period (2015-2018) to is one of the most associated with ADHD.3 6-year-olds and review practice chang- common neuro- Boys are twice as likely as adolescents up to es and newly identified behavioral girls to receive the ADHD age 18 years.12 Since issues since the 2011 4, 5, 6 disorders of diagnosis, perhaps the release of the guidelines. -

Therapeutic Class Overview Irritable Bowel Syndrome and Constipation Agents
Therapeutic Class Overview Irritable Bowel Syndrome and Constipation Agents INTRODUCTION Irritable bowel syndrome (IBS) is a gastrointestinal disorder that most commonly manifests as chronic abdominal pain and altered bowel habits in the absence of any organic disorder (Wald 2017). IBS may consist of diarrhea-predominant (IBS-D), constipation-predominant (IBS-C), IBS with a mixed symptomatology (IBS-M), or unclassified IBS (IBS-U). Switching between the subtypes of IBS is also possible (Ford et al 2018). IBS is a functional disorder of the gastrointestinal tract characterized by symptoms of abdominal pain, discomfort and bloating, and abnormal bowel habits with bouts of diarrhea and/or constipation. The exact pathogenesis of the disorder is unknown; however, it is believed that altered gastrointestinal tract motility, visceral hypersensitivity, autonomic dysfunction, and psychological factors indicate disturbances within the enteric nervous system, which controls the gastrointestinal system (Andresen et al 2008, Ford et al 2009, Quigley et al 2012, World Gastroenterology Organization [WGO] 2015). Prevalence estimates of IBS range from 10 to 12%, and it typically occurs in young adulthood (Ford et al 2018). IBS-D is more common in men, and IBS-C is more common in women (WGO 2015). Symptoms of IBS often interfere with daily life and social functioning (WGO 2015). The general goals of therapy in IBS are to alleviate the patient’s symptoms and to target any specific exacerbating factors (eg, medications, dietary changes), concerns about serious illness, stressors, or potential psychiatric comorbidities that may exist (Wald 2017). Non-pharmacological interventions to combat IBS symptoms include dietary modifications such as exclusion of gas- producing foods (eg, beans, prunes, Brussel sprouts, bagels, etc.), and consumption of probiotics, as well as psychosocial therapies (eg, hypnosis, biofeedback, etc.) (Ford et al 2018). -

Effects of the Antibiotic Rifaximin on Cortical Functional Connectivity Are
www.nature.com/scientificreports OPEN Efects of the antibiotic rifaximin on cortical functional connectivity are mediated through insular cortex Davide Sometti1,2,3*, Chiara Ballan1,3, Huiying Wang4, Christoph Braun1,2,3,5 & Paul Enck6 It is well-known that antibiotics afect commensal gut bacteria; however, only recently evidence accumulated that gut microbiota (GM) can infuence the central nervous system functions. Preclinical animal studies have repeatedly highlighted the efects of antibiotics on brain activity; however, translational studies in humans are still missing. Here, we present a randomized, double-blind, placebo-controlled study investigating the efects of 7 days intake of Rifaximin (non-absorbable antibiotic) on functional brain connectivity (fc) using magnetoencephalography. Sixteen healthy volunteers were tested before and after the treatment, during resting state (rs), and during a social stressor paradigm (Cyberball game—CBG), designed to elicit feelings of exclusion. Results confrm the hypothesis of an involvement of the insular cortex as a common node of diferent functional networks, thus suggesting its potential role as a central mediator of cortical fc alterations, following modifcations of GM. Also, the Rifaximin group displayed lower connectivity in slow and fast beta bands (15 and 25 Hz) during rest, and higher connectivity in theta (7 Hz) during the inclusion condition of the CBG, compared with controls. Altogether these results indicate a modulation of Rifaximin on frequency-specifc functional connectivity that could involve cognitive fexibility and memory processing. Te interest in human gut microbiota and its efects on CNS functioning increased exponentially over the last decade1–9. Strong preclinical evidence testifed an efect of the GM on brain functioning and development 10. -

Rifaximin, a Non-Absorbable Antibiotic, Inhibits the Release of Pro-Angiogenic Mediators in Colon Cancer Cells Through a Pregnane X Receptor-Dependent Pathway
INTERNATIONAL JOURNAL OF ONCOLOGY 49: 639-645, 2016 Rifaximin, a non-absorbable antibiotic, inhibits the release of pro-angiogenic mediators in colon cancer cells through a pregnane X receptor-dependent pathway GIUSEPPE Esposito1*, Stefano GIGLI1*, LUISA SEGUELLA1, NICOLA NOBILE1, ALESSANDRA D'ALESSANDRO2, MARCEllA PESCE2, ELENA CAPOCCIA1, LUCA STEARDO1, CARLA CIRILLO3, ROSARIO CuOMO2 and Giovanni SARNELLI2 1Department of Physiology and Pharmacology, ‘Vittorio Erspamer’, La Sapienza University of Rome, I-00185 Rome; 2Department of Clinical Medicine and Surgery, ‘Federico II’ university of Naples, I-80131 Naples, Italy; 3Laboratory for Enteric NeuroScience (LENS), Translational Research Center for Gastrointestinal Disorders (TARGID), University of Leuven, 3000 Leuven, Belgium Received February 22, 2016; Accepted March 3, 2016 DOI: 10.3892/ijo.2016.3550 Abstract. Activation of intestinal human pregnane X receptor VEGF secretion, NO release, VEGFR-2 expression, MMP-2 (PXR) has recently been proposed as a promising strategy for and MMP-9 expression vs. untreated cells. Rifaximin treat- the chemoprevention of inflammation-induced colon cancer. ment also resulted in a concentration-dependent decrease in The present study was aimed at evaluating the effect of rifax- the phosphorylation of Akt, mTOR, p38MAPK and inhibition imin, a non-absorbable antibiotic, in inhibiting angiogenesis of hypoxia-inducible factor 1-α (HIF-1α), p70S6K and NF-κB. in a model of human colorectal epithelium and investigating Ketoconazole (PXR antagonist) treatment inhibited these the role of PXR in its mechanism of action. Caco-2 cells were effects. These findings demonstrated that rifaximin causes treated with rifaximin (0.1, 1.0 and 10.0 µM) in the presence PXR-mediated inhibition of angiogenic factors in Caco-2 cell or absence of ketoconazole (10 µM) and assessed for cell line and may be a promising anticancer tool. -

Xifaxan (Rifaximin)
Xifaxan (rifaximin) Policy Number: 5.01.745 Last Review: 06/2021 Origination: 06/2021 Next Review: 06/2022 Policy Blue Cross and Blue Shield of Kansas City (Blue KC) will provide coverage for Xifaxan (Rifaximin) when it is determined to be medically necessary because the criteria shown below are met. When Policy Topic is covered Xifaxan may be considered medically necessary for the following FDA Approved indications when criteria are met: FDA Approved Indications 1. Travelers' Diarrhea (TD). Approve 1 time only if patient meets the following: a. Diagnosis of travelers' diarrhea (TD); AND b. One of the following: i. Trial and failure of one of the following: • Zithromax (Azithromycin) • Cipro (Ciprofloxacin) • Levaquin (Levofloxacin) • Ofloxacin OR ii. Resistance, contraindication, or intolerance to all the following antibiotics: • Zithromax (Azithromycin) • Cipro (Ciprofloxacin) • Levaquin (Levofloxacin) • Ofloxacin 2. Small Bowel Bacterial Overgrowth (SBBO)/Small Intestinal Bacterial overgrowth (SIBO) (off-label). Approve for 3 months of Initial treatment if patient meets the following: a. Diagnosis of Small Bowel Bacterial Overgrowth (SBBO)/Small Intestinal Bacterial Overgrowth (SIBO); AND b. One of the following: i. Trial and failure of two of the following antibiotics: • Neomycin • Augmentin (amoxicillin/clavulanic acid) • Cipro (ciprofloxacin) • Bactrim (trimethoprim-sulfamethoxazole) • Vibramycin (doxycycline) OR Minocin (minocycline) OR Tetracycline • Flagyl (metronidazole) • Keflex (Cephalexin) OR ii. Resistance, contraindication, or intolerance to all the following antibiotics: • Neomycin • Augmentin (amoxicillin/clavulanic acid) • Cipro (ciprofloxacin) • Bactrim (trimethoprim-sulfamethoxazole) • Vibramycin (doxycycline) OR Minocin (minocycline) OR Tetracycline • Flagyl (metronidazole) • Keflex (Cephalexin) Reauthorization. Approve for 3 months upon documentation of Positive clinical responses to therapy (e.g., resolution of symptoms or Relapse with Xifaxan discontinuation). -

1 TITLE PAGE CLINICAL STUDY PROTOCOL a Randomized, Double
1 TITLE PAGE CLINICAL STUDY PROTOCOL A randomized, double-blind, parallel group, placebo-controlled, multi-center, therapeutic equivalence study to compare Rifaximin 200 mg tablets (Sandoz GmbH) to Xifaxan® 200 mg tablets (Salix Pharmaceuticals, Inc.) and placebo in patients with travelers’ diarrhea Protocol No.: 1526 RIF_2 / NCT02920242 Test Product: rifaximin Indication: Travelers’ diarrhea Development Phase: Phase III Sponsor: Sandoz GmbH Biochemiestrasse 10 6250 Kundl Austria Sponsor Representative Signatory: Clinical Research Organization Date of the Protocol: October 29, 2015 Version of the Protocol: 2.0 The confidential information in this document is provided to you as an Investigator, potential Investigator or consultant for review by you, your staff and applicable Ethics Committee. It is understood that the information will not be disclosed to others without written authorization from Sandoz GmbH except to the extent necessary to obtain informed consent from those persons to whom the drug may be administered. Protocol No. 1526 RIF_2 Sandoz GmbH CONFIDENTIAL rifaximin 200 mg Version History Version Date Summary of Changes Final Version 1.0 02 October 2015 -- Final Version 2.0 28 October 2015 Appendix II Visual Scale for Patient Assessment of Stools deleted; reference to most recent version of Declaration of Helsinki updated; text edits for clarification of dosing; formatting Changes made prior to submission to any regulatory agencies Version 2.0, October 29, 2015 Page 2 of 90 Protocol No. 1526 RIF_2 Sandoz GmbH CONFIDENTIAL rifaximin 200 mg 2 SIGNATURE PAGES SPONSOR REPRESENTATIVE SIGNATURE PAGE PROTOCOL TITLE: A randomized, double-blind, parallel group, placebo-controlled, multi-center, therapeutic equivalence study to compare Rifaximin 200 mg tablets (Sandoz GmbH) to Xifaxan® 200 mg tablets (Salix Pharmaceuticals, Inc.) and placebo in patients with travelers’ diarrhea PROTOCOL NUMBER: 1526 RIF_2 SPONSOR REPRESENTATIVE Date (day/month/year) Date (day/month/year) Version 2.0, October 29, 2015 Page 3 of 90 Protocol No. -

Rifaximin Preserves Intestinal Microbiota Balance in Patients Undergoing Allogeneic Stem Cell Transplantation
Bone Marrow Transplantation (2016) 51, 1087–1092 © 2016 Macmillan Publishers Limited, part of Springer Nature. All rights reserved 0268-3369/16 www.nature.com/bmt ORIGINAL ARTICLE Rifaximin preserves intestinal microbiota balance in patients undergoing allogeneic stem cell transplantation D Weber1, PJ Oefner2, K Dettmer2, A Hiergeist3, J Koestler3, A Gessner3, M Weber4, F Stämmler5, J Hahn1, D Wolff1, W Herr1 and E Holler1 Intestinal dysbiosis has been associated with acute gastrointestinal GvHD and poor outcome following allogeneic stem cell transplantation (ASCT). To assess the effect of a switch in 2012 from ciprofloxacin/metronidazole to rifaximin for gut decontamination on intestinal microbiota composition and ASCT outcome, we retrospectively analyzed 394 patients receiving ASCT from September 2008 through June 2015. In 131 and 90 patients, respectively, urinary 3-indoxyl sulfate levels and intestinal enterococcal load were measured before conditioning and weekly within the first 28 days after ASCT. The use of rifaximin correlated with lower enterococcal positivity (6.9 vs 21.9%, P=0.05) and higher urinary 3-indoxyl sulfate concentrations (10.5 vs 4.6 μmoL/mmoL crea, Po0.001) after ASCT. Patients on rifaximin showed lower 1-year transplant-related mortality (P=0.04) and higher overall survival (P=0.008). Treatment of infectious complications with systemic antibiotics did not abrogate the beneficial effects of rifaximin on intestinal microbiota composition in the early course of ASCT and outcome. The data underscore the importance of -
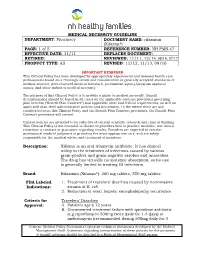
Rifaximin (Xifaxan®) PAGE: 1 of 5 REFERENCE NUMBER
MEDICAL NECESSITY GUIDELINE DEPARTMENT: Pharmacy DOCUMENT NAME: rifaximin (Xifaxan®) PAGE: 1 of 5 REFERENCE NUMBER: NH.PMN.47 EFFECTIVE DATE: 11/11 REPLACES DOCUMENT: RETIRED: REVIEWED: 11/11, 12/14, 08/16, 07/17 PRODUCT TYPE: All REVISED: 11/12, 11/13, 09/16 IMPORTANT REMINDER This Clinical Policy has been developed by appropriately experienced and licensed health care professionals based on a thorough review and consideration of generally accepted standards of medical practice, peer-reviewed medical literature, government agency/program approval status, and other indicia of medical necessity. The purpose of this Clinical Policy is to provide a guide to medical necessity. Benefit determinations should be based in all cases on the applicable contract provisions governing plan benefits (“Benefit Plan Contract”) and applicable state and federal requirements, as well as applicable plan-level administrative policies and procedures. To the extent there are any conflicts between this Clinical Policy and the Benefit Plan Contract provisions, the Benefit Plan Contract provisions will control. Clinical policies are intended to be reflective of current scientific research and clinical thinking. This Clinical Policy is not intended to dictate to providers how to practice medicine, nor does it constitute a contract or guarantee regarding results. Providers are expected to exercise professional medical judgment in providing the most appropriate care, and are solely responsible for the medical advice and treatment of members. Description: Xifaxan is an oral rifamycin antibiotic. It has clinical utility in the treatment of infections caused by various gram-positive and gram-negative aerobes and anaerobes. The drug has virtually no systemic absorption, so its use is generally limited to treating GI infections.