The Large Intestine
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

The Herbivore Digestive System Buffalo Zebra
The Herbivore Digestive System Name__________________________ Buffalo Ruminant: The purpose of the digestion system is to ______________________________ _____________________________. Bacteria help because they can digest __________________, a sugar found in the cell walls of________________. Zebra Non- Ruminant: What is the name for the largest section of Organ Color Key a ruminant’s Mouth stomach? Esophagus __________ Stomach Small Intestine Cecum Large Intestine Background Information for the Teacher Two Strategies of Digestion in Hoofed Mammals Ruminant Non‐ruminant Representative species Buffalo, cows, sheep, goats, antelope, camels, Zebra, pigs, horses, asses, hippopotamus, rhinoceros giraffes, deer Does the animal Yes, regurgitation No regurgitation regurgitate its cud to Grass is better prepared for digestion, as grinding Bacteria can not completely digest cell walls as chew material again? motion forms small particles fit for bacteria. material passes quickly through, so stool is fibrous. Where in the system do At the beginning, in the rumen Near the end, in the cecum you find the bacteria This first chamber of its four‐part stomach is In this sac between the two intestines, bacteria digest that digest cellulose? large, and serves to store food between plant material, the products of which pass to the rumination and as site of digestion by bacteria. bloodstream. How would you Higher Nutrition Lower Nutrition compare the nutrition Reaps benefits of immediately absorbing the The digestive products made by the bacteria are obtained via digestion? products of bacterial digestion, such as sugars produced nearer the end of the line, after the small and vitamins, via the small intestine. intestine, the classic organ of nutrient absorption. -

Mouth Esophagus Stomach Rectum and Anus Large Intestine Small
1 Liver The liver produces bile, which aids in digestion of fats through a dissolving process known as emulsification. In this process, bile secreted into the small intestine 4 combines with large drops of liquid fat to form Healthy tiny molecular-sized spheres. Within these spheres (micelles), pancreatic enzymes can break down fat (triglycerides) into free fatty acids. Pancreas Digestion The pancreas not only regulates blood glucose 2 levels through production of insulin, but it also manufactures enzymes necessary to break complex The digestive system consists of a long tube (alimen- 5 carbohydrates down into simple sugars (sucrases), tary canal) that varies in shape and purpose as it winds proteins into individual amino acids (proteases), and its way through the body from the mouth to the anus fats into free fatty acids (lipase). These enzymes are (see diagram). The size and shape of the digestive tract secreted into the small intestine. varies in each individual (e.g., age, size, gender, and disease state). The upper part of the GI tract includes the mouth, throat (pharynx), esophagus, and stomach. The lower Gallbladder part includes the small intestine, large intestine, The gallbladder stores bile produced in the liver appendix, and rectum. While not part of the alimentary 6 and releases it into the duodenum in varying canal, the liver, pancreas, and gallbladder are all organs concentrations. that are vital to healthy digestion. 3 Small Intestine Mouth Within the small intestine, millions of tiny finger-like When food enters the mouth, chewing breaks it 4 protrusions called villi, which are covered in hair-like down and mixes it with saliva, thus beginning the first 5 protrusions called microvilli, aid in absorption of of many steps in the digestive process. -

Epithelial Control of Gut-Associated Lymphoid Tissue Formation Through P38α-Dependent Restraint of NF-Κb Signaling
Epithelial Control of Gut-Associated Lymphoid Tissue Formation through p38 α -Dependent Restraint of NF-κB Signaling This information is current as Celia Caballero-Franco, Monica Guma, Min-Kyung Choo, of September 27, 2021. Yasuyo Sano, Thomas Enzler, Michael Karin, Atsushi Mizoguchi and Jin Mo Park J Immunol 2016; 196:2368-2376; Prepublished online 20 January 2016; doi: 10.4049/jimmunol.1501724 Downloaded from http://www.jimmunol.org/content/196/5/2368 Supplementary http://www.jimmunol.org/content/suppl/2016/01/19/jimmunol.150172 Material 4.DCSupplemental http://www.jimmunol.org/ References This article cites 53 articles, 20 of which you can access for free at: http://www.jimmunol.org/content/196/5/2368.full#ref-list-1 Why The JI? Submit online. • Rapid Reviews! 30 days* from submission to initial decision by guest on September 27, 2021 • No Triage! Every submission reviewed by practicing scientists • Fast Publication! 4 weeks from acceptance to publication *average Subscription Information about subscribing to The Journal of Immunology is online at: http://jimmunol.org/subscription Permissions Submit copyright permission requests at: http://www.aai.org/About/Publications/JI/copyright.html Email Alerts Receive free email-alerts when new articles cite this article. Sign up at: http://jimmunol.org/alerts The Journal of Immunology is published twice each month by The American Association of Immunologists, Inc., 1451 Rockville Pike, Suite 650, Rockville, MD 20852 Copyright © 2016 by The American Association of Immunologists, Inc. All rights reserved. Print ISSN: 0022-1767 Online ISSN: 1550-6606. The Journal of Immunology Epithelial Control of Gut-Associated Lymphoid Tissue Formation through p38a-Dependent Restraint of NF-kB Signaling Celia Caballero-Franco,* Monica Guma,†,‡ Min-Kyung Choo,* Yasuyo Sano,* Thomas Enzler,*,x Michael Karin,†,{ Atsushi Mizoguchi,‖ and Jin Mo Park* The protein kinase p38a mediates cellular responses to environmental and endogenous cues that direct tissue homeostasis and immune responses. -

6-Physiology of Large Intestine.Pdf
LARGE INTESTINE COLON MOTILITY Color index • Important • Further explanation 1 Contents . Mind map.......................................................3 . Colon Function…………………………………4 . Physiology of Colon Regions……...…………6 . Absorption and Secretion…………………….8 . Types of motility………………………………..9 . Innervation and motility…………………….....11 . Defecation Reflex……………………………..13 . Fecal Incontinence……………………………15 Please check out this link before viewing the file to know if there are any additions/changes or corrections. The same link will be used for all of our work Physiology Edit 2 Mind map 3 COLON FUNCTIONS: Secretions of the Large Intestine: Mucus Secretion. • The mucosa of the large intestine has many crypts of 3 Colon consist of : Lieberkühn. • Absence of villi. • Ascending • Transverse • The epithelial cells contain almost no enzymes. • Descending • Presence of goblet cells that secrete mucus (provides an • Sigmoid adherent medium for holding fecal matter together). • Rectum • Anal canal • Stimulation of the pelvic nerves1 from the spinal cord can cause: Functions of the Large Intestine: o marked increase in mucus secretion. o This occurs along with increase in peristaltic motility 1. Reabsorb water and compact material of the colon. into feces. 2. Absorb vitamins produced by bacteria. • During extreme parasympathetic stimulation, so much 3. Store fecal matter prior to defecation. mucus can be secreted into the large intestine that the person has a bowel movement of ropy2 mucus as often as every 30 minutes; this mucus often contains little or no 1: considered a part of parasympathetic in large intestine . fecal material. 2: resembling a rope in being long, strong, and fibrous 3: anatomical division. 4 ILEOCECAL VALVE It prevents backflow of contents from colon into small intestine. -

6 Physiology of the Colon : Motility
#6 Physiology of the colon : motility Objectives : ● Parts of the Colon ● Functions of the Colon ● The physiology of Different Colon Regions ● Secretion in the Colon ● Nutrient Digestion in the Colon ● Absorption in the Colon ● Bacterial Action in the Colon ● Motility in the Colon ● Defecation Reflex Doctors’ notes Extra Important Resources: 435 Boys’ & Girls’ slides | Guyton and Hall 12th & 13th edition Editing file [email protected] 1 ﺗﻛرار ﻣن اﻟﮭﺳﺗوﻟوﺟﻲ واﻷﻧﺎﺗوﻣﻲ The large intestine ● This is the final digestive structure. ● It does not contain villi. ● By the time the digested food (chyme) reaches the large intestine, most of the nutrients have been absorbed. ● The primary role of the large intestine is to convert chyme into feces for excretion. Parts of the colon ● The colon has a length of about 150 cm. ( 1.5 meters) (one-fifth of the whole length of GIT). ● It consists of the ascending & descending colon, transverse colon, sigmoid colon, rectum and anal canal. 3 ● The transit of radiolabeled chyme through 4 the large intestine occurs in 36-48 hrs. 2 They know this how? By inserting radioactive chyme. 1 6 5 ❖ Mucous membrane of the colon ● Lacks villi and has many crypts of lieberkuhn. ● They consists of simple short glands lined by mucous-secreting goblet cells. Main colonic secretion is mucous, as the colon lacks digestive enzymes. ● The outer longitudinal muscle layer is modified to form three longitudinal bands called taenia coli visible on the outer surface.(Taenia coli: Three thickened bands of muscles.) ● Since the muscle bands are shorter than the length of the colon, the colonic wall is sacculated and forms haustra.(Haustra: Sacculation of the colon between the taenia.) Guyton corner : mucus in the large intestine protects the intestinal wall against excoriation, but in addition, it provides an adherent medium for holding fecal matter together. -

Anatomy of the Digestive System
The Digestive System Anatomy of the Digestive System We need food for cellular utilization: organs of digestive system form essentially a long !nutrients as building blocks for synthesis continuous tube open at both ends !sugars, etc to break down for energy ! alimentary canal (gastrointestinal tract) most food that we eat cannot be directly used by the mouth!pharynx!esophagus!stomach! body small intestine!large intestine !too large and complex to be absorbed attached to this tube are assorted accessory organs and structures that aid in the digestive processes !chemical composition must be modified to be useable by cells salivary glands teeth digestive system functions to altered the chemical and liver physical composition of food so that it can be gall bladder absorbed and used by the body; ie pancreas mesenteries Functions of Digestive System: The GI tract (digestive system) is located mainly in 1. physical and chemical digestion abdominopelvic cavity 2. absorption surrounded by serous membrane = visceral peritoneum 3. collect & eliminate nonuseable components of food this serous membrane is continuous with parietal peritoneum and extends between digestive organs as mesenteries ! hold organs in place, prevent tangling Human Anatomy & Physiology: Digestive System; Ziser Lecture Notes, 2014.4 1 Human Anatomy & Physiology: Digestive System; Ziser Lecture Notes, 2014.4 2 is suspended from rear of soft palate The wall of the alimentary canal consists of 4 layers: blocks nasal passages when swallowing outer serosa: tongue visceral peritoneum, -

Human Body- Digestive System
Previous reading: Human Body Digestive System (Organs, Location and Function) Science, Class-7th, Rishi Valley School Next reading: Cardiovascular system Content Slide #s 1) Overview of human digestive system................................... 3-4 2) Organs of human digestive system....................................... 5-7 3) Mouth, Pharynx and Esophagus.......................................... 10-14 4) Movement of food ................................................................ 15-17 5) The Stomach.......................................................................... 19-21 6) The Small Intestine ............................................................... 22-23 7) The Large Intestine ............................................................... 24-25 8) The Gut Flora ........................................................................ 27 9) Summary of Digestive System............................................... 28 10) Common Digestive Disorders ............................................... 31-34 How to go about this module 1) Have your note book with you. You will be required to guess or answer many questions. Explain your guess with reasoning. You are required to show the work when you return to RV. 2) Move sequentially from 1st slide to last slide. Do it at your pace. 3) Many slides would ask you to sketch the figures. – Draw them neatly in a fresh, unruled page. – Put the title of the page as the slide title. – Read the entire slide and try to understand. – Copy the green shade portions in the note book. 4) -
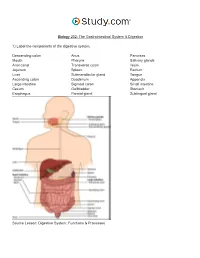
The Gastrointestinal System & Digestion Visual Worksheet
Biology 202: The Gastrointestinal System & Digestion 1) Label the components of the digestive system. Descending colon Anus Pancreas Mouth Pharynx Salivary glands Anal canal Transverse colon Ileum Jejunum Spleen Rectum Liver Submandibular gland Tongue Ascending colon Duodenum Appendix Large intestine Sigmoid colon Small intestine Cecum Gallbladder Stomach Esophagus Parotid gland Sublingual gland Source Lesson: Digestive System: Functions & Processes 2) Label the image below. Serosa Submucous plexus Muscularis externa Submucosa Myenteric plexus Muscular interna Source Lesson: Role of the Enteric Nervous System in Digestion 3) Label the structures of the alimentary canal. Some terms may be used more than once. Vein Mesentery Mucosa Submucosal plexus Epithelium Gland in mucosa Nerve Muscularis Serosa Lymphatic tissue Muscularis mucosae Glands in submucosa Lamina propria Submucosa Duct of gland outside tract Gland in mucosa Lumen Artery Longitudinal muscle Musculararis Areolar connective tissue Circular muscle Myenteric plexus Source Lesson: The Upper Alimentary Canal: Key Structures, Digestive Processes & Food Propulsion 4) Label the image below. Stomach Trachea Lower esophageal sphincter Esophagus Upper esophageal sphincter Source Lesson: The Upper Alimentary Canal: Key Structures, Digestive Processes & Food Propulsion 5) Label the anatomy of the oral cavity. Upper lip Tonsil Inferior labial frenulum Floor of mouth Tongue Superior labial frenulum Lower lip Teeth Retromolar trigone Palatine arch Hard palate Uvula Glossopalatine arch Soft palate Gingiva Source Lesson: The Oral Cavity: Structures & Functions 6) Label the structures of the oral cavity. Some terms may be used more than once. Hard palate Oropharynx Soft palate Pharyngeal tonsil Oral cavity Lingual tonsil Superior lip Teeth Palatine tonsil Tongue Inferior lip Source Lesson: The Oral Cavity: Structures & Functions 7) Label the image below. -

Internal Anal Sphincter
Arch Dis Child: first published as 10.1136/adc.43.231.569 on 1 October 1968. Downloaded from Arch. Dis. Childh., 1968, 43, 569. Internal Anal Sphincter Observations on Development and Mechanism of Inhibitory Responses in Premature Infants and Children with Hirschsprung's Disease E. R. HOWARD and H. H. NIXON From The Hospitalfor Sick Children, Great Ormond Street, London W.C.1 The relative importance of the internal and obstruction to constipation alone. During this external sphincters to the maintenance of tone in study physiological abnormalities were observed in the anal canal has been shown in previous studies of the reflexes of premature infants, which showed anal physiology (Gaston, 1948; Schuster et al., 1965; similarities to those seen in patients with Hirsch- Duthie and Watts, 1965). sprung's disease. On repeated examinations over The external sphincter is a striated muscle, but several days, however, the physiological responses shows continuous activity on electromyography. were found to change until normal reflexes were Inhibition and stimulation is mediated by spinal eventually established. cord reflexes, through the pudendal nerves and In order to help determine the nervous pathway sacral segments of the spinal cord (Floyd and Walls, through which the reflexes of the internal sphincter copyright. 1953; Porter, 1961). Voluntary control is possible are mediated, we have examined normal bowel over this part ofthe anal sphincter. and aganglionic bowel from cases of Hirschsprung's The internal sphincter is made up of smooth disease by pharmacological and histochemical muscle fibres, continuous with the muscle layers of methods. the rectal wall, and under resting conditions pro- vides most of the tone of the anal canal (Duthie and Physiological Study Watts, 1965). -

Aandp2ch25lecture.Pdf
Chapter 25 Lecture Outline See separate PowerPoint slides for all figures and tables pre- inserted into PowerPoint without notes. Copyright © McGraw-Hill Education. Permission required for reproduction or display. 1 Introduction • Most nutrients we eat cannot be used in existing form – Must be broken down into smaller components before body can make use of them • Digestive system—acts as a disassembly line – To break down nutrients into forms that can be used by the body – To absorb them so they can be distributed to the tissues • Gastroenterology—the study of the digestive tract and the diagnosis and treatment of its disorders 25-2 General Anatomy and Digestive Processes • Expected Learning Outcomes – List the functions and major physiological processes of the digestive system. – Distinguish between mechanical and chemical digestion. – Describe the basic chemical process underlying all chemical digestion, and name the major substrates and products of this process. 25-3 General Anatomy and Digestive Processes (Continued) – List the regions of the digestive tract and the accessory organs of the digestive system. – Identify the layers of the digestive tract and describe its relationship to the peritoneum. – Describe the general neural and chemical controls over digestive function. 25-4 Digestive Function • Digestive system—organ system that processes food, extracts nutrients, and eliminates residue • Five stages of digestion – Ingestion: selective intake of food – Digestion: mechanical and chemical breakdown of food into a form usable by -

Electrophysiological Studies the Antrum Muscle Fibers of the Guinea
Electrophysiological Studies of the Antrum Muscle Fibers of the Guinea Pig Stomach H. KURIYAMA, T. OSA, and H. TASAKI Downloaded from http://rupress.org/jgp/article-pdf/55/1/48/1244765/48.pdf by guest on 29 September 2021 From the Department of PhysiologT,Faculty of Medicine and Dentistry, Kyushu University, Fukuoka,Japan AB STRAC T The membrane potentials of single smooth muscle fibers of various regions of the stomach were measured, and do not differ from those measured in intestinal muscle. Spontaneous slow waves with superimposed spikes could be recorded from the longitudinal and circular muscle of the antrum. The develop- ment of tension was preceded by spikes but often tension appeared only when the slow waves were generated. Contracture in high K solution developed at a critical membrane potential of --42 my. MnCI~ blocked the spike generation, then lowered the amplitude of the slow wave. On the other hand, withdrawal of Na +, or addition of atropine and tetrodotoxin inhibited the generation of most of the slow waves but a spike could still be elicited by electrical stimula- tion. Prostigmine enhanced and prolonged the slow wave; acetylcholine de- polarized the membrane without change in the frequency of the slow waves. Chronaxie for the spike generation in the longitudinal muscle of the antrum was 30 msec and conduction velocity was 1.2 cm/sec. The time constant of the foot of the propagated spike was 28 reset. The space constants measured from the longitudinal and circular muscles of the antrum were 1.1 mm and 1.4 into, respectively. INTRODUCTION The early investigations of mammalian stomach muscle suggested that mem- brane activity consisted of spike and slow wave components (Alvarez and Mahoney, 1922; Richter, 1923; Bozler, 1938, 1942; and Ichikawa and Bozler, 1955; Daniel, 1965). -
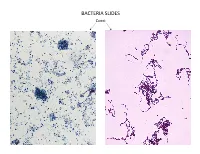
Bacteria Slides
BACTERIA SLIDES Cocci Bacillus BACTERIA SLIDES _______________ __ BACTERIA SLIDES Spirilla BACTERIA SLIDES ___________________ _____ BACTERIA SLIDES Bacillus BACTERIA SLIDES ________________ _ LUNG SLIDE Bronchiole Lumen Alveolar Sac Alveoli Alveolar Duct LUNG SLIDE SAGITTAL SECTION OF HUMAN HEAD MODEL Superior Concha Auditory Tube Middle Concha Opening Inferior Concha Nasal Cavity Internal Nare External Nare Hard Palate Pharyngeal Oral Cavity Tonsils Tongue Nasopharynx Soft Palate Oropharynx Uvula Laryngopharynx Palatine Tonsils Lingual Tonsils Epiglottis False Vocal Cords True Vocal Cords Esophagus Thyroid Cartilage Trachea Cricoid Cartilage SAGITTAL SECTION OF HUMAN HEAD MODEL LARYNX MODEL Side View Anterior View Hyoid Bone Superior Horn Thyroid Cartilage Inferior Horn Thyroid Gland Cricoid Cartilage Trachea Tracheal Rings LARYNX MODEL Posterior View Epiglottis Hyoid Bone Vocal Cords Epiglottis Corniculate Cartilage Arytenoid Cartilage Cricoid Cartilage Thyroid Gland Parathyroid Glands LARYNX MODEL Side View Anterior View ____________ _ ____________ _______ ______________ _____ _____________ ____________________ _____ ______________ _____ _________ _________ ____________ _______ LARYNX MODEL Posterior View HUMAN HEART & LUNGS MODEL Larynx Tracheal Rings Found on the Trachea Left Superior Lobe Left Inferior Lobe Heart Right Superior Lobe Right Middle Lobe Right Inferior Lobe Diaphragm HUMAN HEART & LUNGS MODEL Hilum (curvature where blood vessels enter lungs) Carina Pulmonary Arteries (Blue) Pulmonary Veins (Red) Bronchioles Apex (points