2018 [Pdf, 1.9
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

COMMUNITY HEALTH NEEDS ASSESSMENT, Monmouth Medical
COMMUNITY HEALTH NEEDS ASSESSMENT 2016-2018 DECEMBER 7, 2016 ACKNOWLEDGEMENTS The following partners led the Monmouth Medical Center Southern Campus Community Health Needs Assessment: BARNABAS HEALTH COMMUNITY HEALTH NEEDS ASSESSMENT STEERING COMMITTEE The Barnabas Health CHNA Steering Committee oversees the 2016 CHNA process to update the 2013 CHNAs and create new Implementation Plans. The key tasks of the Steering Committee include: Review 2013 facility implementation plan updates and results Review 2015 community and public health surveys Review of suggested priorities for facility implementation planning Oversight and guidance of CHNA implementation plan development Review and sign-off of 2016 CHNA and implementation plans Members of the Barnabas Health CHNA Steering Committee include: Jen Velez, SVP, Community and Behavioral Health, Committee Chair Michellene Davis, EVP, Corporate Affairs Robert Braun, Oncology leadership Connie Greene, Behavioral Health/Preventive Care Joseph Jaeger, DrPH, Chief Academic Officer Barbara Mintz, VP, Health and Wellness Michael Knecht, Corporate Vice President, Strategic Messaging and Marketing Ernani Sadural, M.D., Director of Global Health for Barnabas Health Shari Beirne, Barnabas Health Behavioral Health Center, Designate Teri Kubiel, Ph.D., CMC Designate Frank Mazzarella, MD, CMMC Designate Brenda Hall, JCMC, Designate Anna Burian, MMC, Designate Judy Colorado, MMCSC, Designate Darrell Terry, NBIMC, President and CEO Ceu Cirne Neves, SBMC, Designate Charlene Harding, Planning -

Regional Chief Medical Informatics Officers (Central & Southern Regions) Organization Overview
Position Profile Regional Chief Medical Informatics Officers (Central & Southern Regions) Organization Overview Hackensack Meridian Health is New Jersey’s Largest, Most Comprehensive and Most Integrated Health Network Hackensack Meridian Health (HMH) is a leading not-for-profit health care organization that is the largest, most comprehensive and truly integrated health care network in New Jersey, offering a complete range of medical services, innovative research and life-enhancing care. Hackensack Meridian Health includes 17 hospitals and 500 patient care locations throughout the state which include ambulatory care centers, surgery centers, home health services, long-term care and assisted living communities, ambulance services, lifesaving air medical transportation, fitness and ellnessw centers, rehabilitation centers, urgent care centers and physician practice locations. Mission “Transform health care and be recognized as the leader of positive change.” Vision “Innovation is in our DNA, compelling us to create a world where: the highest quality care is human-centered, accessible and affordable; we deliver outcomes that matter most; and excellence is the standard.” Key Network Indicators • 6,500 physicians • 175,647 admissions • 17 hospitals • 18,063 births • 500 locations • 1,916,065 outpatient visits • 34,100 employees • $6.5 billion net revenue • 4,303 licensed beds • $271 million operating gain Source: 2017 Annual Report Organization Overview Recognition • America’s 50 Best Hospitals award for five or more consecutive years, Hackensack University Medical Center, (One of only five U.S. major academic medical centers receive this award), Healthgrades • Top 10 Hospitals in New Jersey: Hackensack University Medical Center at #2, Jersey Shore University Medical Center at #4, Riverview Medical Centers #8, Raritan Bay Medical Center - Perth Amboy #10, U.S. -

A Surgical Solution Riverview Medical Center a Middletown Father and Musician Receives Expert Surgical Care
Enjoying Life After The Right Treatment 6 Tips for Life as a Lung Cancer p15 at the Right Time p22 Cancer Survivor p30 SEPTEMBER/ OCTOBER 2016 A Surgical Solution Riverview Medical Center A Middletown father and musician receives expert surgical care. page 10 MORE ONLINE AT HACKENSACKMERIDIANHEALTH.ORG ConnectWITH US A MESSAGE TO THE COMMUNITY We are excited to announce that Meridian Health and Hackensack POST YOUR PET’S University Health Network have joined HALLOWEEN COSTUME! together to become Hackensack Meridian Does your pet wear a Health, creating a whole new state of Halloween costume? health care in New Jersey and beyond. We want to see! Share a As a result, Meridian HealthViews is now photo on Instagram using Hackensack Meridian HealthViews! #HowlHackensackMeridian. Hackensack Meridian Health L to R: Robert C. Garrett and John K. Lloyd translates into 13 hospitals, including Moving forward, you’ll see more two academic medical centers, two patient stories from Hackensack children’s hospitals, and nine community University Medical Center, which is RANKED AMONG THE BEST...AGAIN! hospitals. We believe that the effective ranked by U.S. News & World Report as Our hospitals have once again earned high and compassionate care you have come the number one hospital in New recognition in U.S. News & World Report’s to expect from our hospitals will only Jersey, as well as other features that Best Regional Hospitals 2016–17 annual strengthen, as you now have access to show the depth and breadth of rankings. In New Jersey, Hackensack the unmatched depth of expert care our new health network. -

Center for Integrated Palliative Medicine Is an Outpatient Program for Patients Dealing with a Serious Illness
Center for Integrated Palliative Hackensack Meridian Health Care Journey is a comprehensive palliative care Medicine program offered to patients in Monmouth and Ocean counties. This program has four components to address the needs of patients, no matter where they are receiving care within the Hackensack Brick Meridian Health network: hospital, nursing Ocean Medical Center Cancer Center 425 Jack Martin Boulevard and rehabilitation centers, home or at a Brick, NJ 08724 physician practice. Manahawkin Inpatient Palliative Care Consultation: Southern Ocean Medical Center 1140 Route 72 West, Suite 306A Our inpatient palliative care Manahawkin, NJ 08050 consultation program is offered at our network hospitals. Neptune HOPE Tower at Outpatient Palliative Care Consultation: Jersey Shore University Medical Center 19 Davis Avenue, 2nd Floor At our Hackensack Meridian Health Neptune, NJ 07753 Nursing & Rehabilitation facilities, a palliative care referral-based outpatient Red Bank Riverview Medical Center consultation program is offered. Jane Booker Building, 2nd Floor 1 Riverview Plaza Home-based Palliative Care Program Red Bank, NJ 07701 A home-based service that offers Phone: 732-268-8470 nursing, social work and spiritual visits Fax: 732-268-8459 for support of patients and their families. For more information about any of our other Palliative Care Programs, call 732-202-8071 Outpatient Practices or visit HMHCareJourney.org. Center for Integrated Palliative Medicine is an outpatient program for patients dealing with a serious illness. HMMG-0660-CIMP-bro_9.18-1M SPS About the Program Our Professional Staff We welcome you to our practice and look forward to accompanying you on your journey Our mission at the Center for Integrated Palliative We have a multidisciplinary team of experienced to a better quality of life. -

Riverview Medical Center Foundation Brings Fireworks Back to the Navesink River on July 3
NEWS Riverview Medical Center Foundation Brings Fireworks Back to the Navesink River on July 3 Family Fireworks on the Navesink Generously Hosted by the DiPiero Family Red Bank, NJ – June 13, 2019 – The Hackensack Meridian Health Riverview Medical Center Foundation Board of Trustees is pleased to announce the Seventh Annual Family Fireworks on the Navesink to support Riverview Medical Center Foundation. This annual event will again be held at the DiPiero home on the picturesque Navesink River, on Wednesday, July 3 at 6:30 p.m. “Riverview Medical Center is one of the best hospitals in the area, delivering top-notch care for our community, as affirmed by its recent achievement of a sixth consecutive ‘A’ rating from The Leapfrog Group for patient safety,” says Joseph Stampe, president and chief development officer, Hackensack Meridian Health Meridian Health Foundation. “Philanthropy plays a pivotal role in the medical center’s success. It helps to create new spaces for care, provide cutting-edge technology, train team members and enhance the patient experience. By attending this event, guests will ensure that our community continues to have access to the best care, close to home, while getting to learn more about the medical center and enjoy a fabulous fireworks display. We cannot thank the DiPieros enough for their continued support and commitment to philanthropy.” A variety of food options, including food trucks, will be available at the event, and guests will enjoy inflatable rides and games, as well as a front row seat to the fireworks show, which kicks off at 9:30 p.m. -

Safe Syringe Disposal Guide for Home Generated Medical Waste
SAFE SYRINGE DISPOSAL GUIDE FOR HOME GENERATED MEDICAL WASTE If you produce any medical waste at home, this Guide may apply to you. 2008 INTRODUCTION Home generators of medical waste may account for the use of up to 700,000 sharps daily in New Jersey. The most common disease that requires self- injection of insulin and lancets to monitor blood sugar levels at home is diabetes. Data for 2000-2002 indicates that there are approximately 24,000 individuals over the age of 18 who have been diagnosed as diabetic in the State of New Jersey. (NJDHSS Center for Health Statistics) Further, it is estimated that an additional 134,000 individuals in the same age group have diabetes but have yet to be diagnosed. (NJDHSS Family Health Services) The proper disposal of home generated medical waste is an important step that all home generators of medical waste can take to help ensure the health and safety of all New Jerseyans. WHAT HEALTH EFFECTS ARE ASSOCIATED WITH IMPROPER DISPOSAL OF HOME GENERATED MEDICAL WASTE? The improper disposal of home generated medical waste poses a potential health hazard to many, including family members, sanitation workers, people in the community, hotel housekeeping staffs and school personnel. Although rare, diseases as serious as Hepatitis B and AIDS can also result from accidental needle sticks. In addition, loose syringes thrown into your household trash can also be misused if they fall into the wrong hands. Moreover, these items can injure small children, pets and wildlife. DOES THIS GUIDE APPLY TO YOU? The Safe Syringe Disposal Guide (Guide) applies to New Jerseyans generating medical waste at home. -

2019 Bayshore Medical Center CHNA Report
2019 Community Health Needs Assessment Summary Report Bayshore Medical Center Service Area Prepared for: Bayshore Medical Center By: PRC, Inc. 11326 P Street Omaha, NE 68137-2316 www.PRCCustomResearch.com 2019-0258-02 © September 2019 PRC, Inc. COMMUNITY HEALTH NEEDS ASSESSMENT Table of Contents Introduction 4 About This Assessment 5 Methodology 5 PRC Community Health Survey 5 Online Key Informant Survey 8 Public Health, Vital Statistics & Other Data 10 Determining Significance 12 Information Gaps 12 IRS Form 990, Schedule H Compliance 13 Summary of Findings 14 Significant Health Needs: BMC Service Area 14 Summary Tables: Comparisons With Benchmark Data 16 Summary of Key Informant Perceptions 29 Data Charts & Key Informant Input 30 Community Characteristics 31 Population Characteristics 31 Social Determinants of Health 33 General Health Status 41 Overall Health Status 41 Mental Health 43 Death, Disease & Chronic Conditions 53 Leading Causes of Death 53 Cardiovascular Disease 55 Cancer 63 Respiratory Disease 70 Injury & Violence 75 Diabetes 81 Kidney Disease 87 Potentially Disabling Conditions 90 Infectious Disease 101 Births 103 Prenatal Care 103 Birth Outcomes & Risks 104 Family Planning 107 PRC, Inc. 2 2 COMMUNITY HEALTH NEEDS ASSESSMENT Modifiable Health Risks 109 Nutrition, Physical Activity & Weight 109 Substance Abuse 121 Tobacco Use 129 Sexual Health 134 Access to Health Services 140 Lack of Health Insurance Coverage (Age 18 to 64) 140 Difficulties Accessing Healthcare 142 Primary Care Services 148 Oral Health 150 Local Resources 153 Appendix 161 Evaluation of Past Activities 162 PRC, Inc. 3 3 Introduction COMMUNITY HEALTH NEEDS ASSESSMENT About This Assessment This Community Health Needs Assessment is a systematic, data-driven approach to determining the health status, behaviors and needs of residents in the service area of Bayshore Medical Center. -
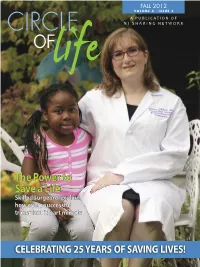
The Power to Save a Life Skilled Surgeons Explain How Every Successful Transplant Is Part Miracle
FALL 2012 VOLUME 3 • ISSUE 2 A PUBLICATION OF NJ SHARING NETWORK The Power to Save a Life Skilled surgeons explain how every successful transplant is part miracle CELEBRATING 25 YEARS OF SAVING LIVES! WHO WE ARE NJ Sharing Network is a non-profit, federally-designated, organ procurement organization responsible for the recovery of organs and tissue for the nearly 5,000 New Jersey residents currently awaiting transplantation, and is part of the national recovery system, which is in place for the more than 115,000 people on waiting lists. WHAT A SPECIAL AND REWARDING BOARD OF TRUSTEES YEAR 2012 IS PROVING TO BE John J. Halperin, MD Chair While we spent a great deal of time in 2012 celebrating the 25th Anniversary of NJ Sharing Bruce I. Goldstein, Esq. Network, we never took our focus off what we celebrate every day: the lives saved through the Vice Chair selfless act of organ and tissue donation. Vito A. Pulito In this issue of Circle of Life , you can learn more about the great work that has been accom - Treasurer plished over the past year as well as how the process of organ and tissue donation connects people Marc H. Lory for life. Secretary This issue’s cover story reveals what it’s like to be a transplant surgeon, both a demanding and Patrick M. Buddle, MD emotional job, but one that is extremely rewarding (see page 8). Other articles discuss how lives Margaret Dreker can be intertwined forever after letter exchanges occur between a donor family and an organ recip - Edward J. -

Extending a Surgeon's Reach
Extending a Surgeon’s Reach Ocean Medical Center Brian Flaherty is a prostate cancer survivor, thanks to his longtime urologist’s vigilance and skill. WHEN BRIAN FLAHERTY WAS DIAGNOSED WITH EARLY-STAGE PROSTATE “The da Vinci System allows surgeons cancer at age 49, he knew he had to thoroughly research his treatment to maneuver, cut, staple, and sew with options. Robot-assisted minimally invasive surgery offered him the best great dexterity in small spaces without chance for a fast and complete recovery. Some friends and damaging surrounding tissues, blood family urged Brian to go to New York City or Philadelphia vessels, and nerves,” says Dr. Mendoza. for the procedure. But after careful consideration, he decided “This results in less blood loss, less pain, that his best move was to stay local. and a faster recovery.” For three years, he’d been seeing Pierre Mendoza, M.D., medical director of Urologic Robotic Surgery at Ocean Medical Center and part of Meridian Cancer Care, for Pierre Mendoza, M.D. regular checkups and biopsies, ever since a benign Board certified in enlargement of his prostate had revealed some Urology Brick precancerous cells that warranted close monitoring. 1-800-560-9990 And Brian knew that in addition to being an excellent diagnostician, Dr. Mendoza was a robotic surgery expert who had completed fellowship training in robot-assisted surgery and had been involved in more than 1,000 cases. “I felt very comfortable with Dr. Mendoza’s experience, and to me, the logical choice was to stay under his care,” Brian says. A Powerful Tool Makes Great Surgeons Even Better At Ocean, Dr. -

CANCER CARE of Monmouth and Ocean Counties
CANCER CARE of Monmouth and Ocean Counties A member of the Memorial Sloan Kettering – Hackensack Meridian Health Partnership 2 Hackensack Meridian Health CANCER CARE OF MONMOUTH AND OCEAN COUNTIES Hackensack Meridian Health Cancer Care of Monmouth and Ocean Counties Dear Friends, When someone is diagnosed with cancer, nothing is more important than knowing they have access to the best physicians, the most compassionate care, and the latest technology and therapies. Hackensack Meridian Health Cancer Care of Monmouth and Ocean counties has made an unyielding commitment to provide the highest level of care and the most advanced treatment options close to home. Our team continues to grow and lead the charge in cancer and innovation through our $128M investment in five brand new state-of-the-art cancer centers throughout Monmouth and Ocean counties. We operate at the highest levels recognized by the American College of Surgeons Commission on Cancer (CoC) as the only network accredited program in New Jersey. Our clinical experts and support teams are in constant communication to make sure each patient’s treatment, progress, and plans for life beyond discharge are seamless. Thomas L. Bauer II, M.D. Through our integrated network comprised of 13 hospitals, including John Theurer Clinical Medical Director of Oncology, Cancer Center at Hackensack University Medical Center, patients have more access Hackensack Meridian Health to clinical trials, support services and resources throughout Hackensack Meridian Health. Looking back on 2017, we have a lot to be proud of and we look forward to Medical Director of Thoracic Oncology, Hackensack Meridian Health even more advancements to take on cancer in 2018. -

2019 Nursing Annual Report 3 from the Chief Nurse Executive
Nursing2019 ANNUAL REPORT Contents 5 11 21 34 Professional Practice Model 3 First Cohort of Hackensack Meridian Health Our mission, vision and philosophy. Nurses Earn DNP from Monmouth University 15 Enhancing the Magnet® Journey 16 Nursing by the Numbers 3 Nurses Stay on Top of Their Game The numbers don’t lie: Hackensack Meridian Health nurses are the best in their field. with Professional Organizations 18 2019 Academic Achievements From the Chief Nursing Executive 4 and National Certifications 20 A message from Theresa M. Brodrick, Ph.D., RN, NE-BC, executive vice president and chief nurse executive, Hackensack Meridian Health SECTION 3 New Knowledge, SECTION 1 Innovations & Improvements 21 Transformational Leadership 5 Research and learning are the keys to delivering improved patient care. How nurses are initiating and leading positive change throughout the network. Nursing Research Studies 22 Theresa Brodrick Recognized as One of Four-year HRSA Award Will Enhance Crain’s Notable Women in Health Care 6 Nurse Practitioner Residency Program 23 Thank You, Denise Occhiuzzo 6 Quality Improvement Initiative 23 Nurses Honored with DAISY Awards 7 Publications and Presentations 24 New Jersey League for Nurses Recognizes Dr. Amanda Hessels Four Hackensack Meridian Health Nurses 8 Secures Prestigious Grant 24 Welcome to Carrier Clinic and Shaun Sweeney 9 Congratulations, Michelle Wilder, SECTION 4 NJBIZ Nurse of the Year 9 Structural Empowerment 25 Chief Nurse Officer Rebecca Graboso Accomplishments of nurses across the network. Wins 2019 Divas & Dons Award 9 Saluting Ellen Angelo, Donna Ciufo Take Vape Away Campaign 26 and Marie Foley-Danecker 10 Community and Military Service 27 Combating Human Trafficking 28 SECTION 2 Foundation Awards and Scholarships 30 Exemplary Professional Practice 11 New Pilot Program with Red Cross 31 A look at noteworthy improvements to processes and practices. -

Tier 1 Advantage Outpatient Surgery and Rehabilitation Center Tier Placements for 2014*
Tier 1 Advantage Outpatient Surgery and Rehabilitation Center Tier Placements for 2014* Tier 1 Atlantic County Center for Endoscopy Fellowship Surgical Center Ocean Surgery Center & Surgical Specialties Florham Park Endoscopy Center Ocean Surgical Pavilion Advanced Endo & Surgical Center Freehold Surgical Center Princeton Endoscopy Center Advantage Therapy Centers Gastro, LLC Rehabilitation Hospital of Tinton Falls Ambulatory Care Center Hamilton Endoscopy and Surgery Ridgedale Surgery Center Atlantic Coastal Surgery Center Hamilton Surgery Center River Drive Surgery Center Atlantic Surgery Center Hand Surgery and Rehabilitation Seashore Ambulatory Surgery Bacharach Institute for Rehabilitation Hanover Endoscopy Center Shore Outpatient Surgicenter Bergen-Passaic Cataract Surgery and Laser HealthSouth – HealthSouth Rehabilitation Shore Rehabilitation Institute Burlington County Endoscopy Center Hospital of Tinton Falls Somerset Eye Institute Campus Eye Group Surgical Center HealthSouth – HealthSouth Rehabilitation South Jersey Endoscopy Center Cape Cataract Center Hospital of Toms River South Jersey Surgicenter CARES Surgicenter Horizon Laser and Eye Surgery St. Lawrence Rehabilitation Hospital Cataract & Laser Institute Hughes Center for Aesthetic Medicine Surgery Center of Central NJ Centennial Surgery Center Kessler Institute for Rehabilitation Surgery Center of Cherry Hill Central Jersey Surgery Center Lakewood Surgery Center Surgi Center of Vineland Cherry Hill Women’s Center Marlton Rehabilitation Hospital Surgical Center of South