Collaborating to Bring SAFE Together
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

ETHIOPIA - National Hot Spot Map 31 May 2010
ETHIOPIA - National Hot Spot Map 31 May 2010 R Legend Eritrea E Tigray R egion !ª D 450 ho uses burned do wn d ue to th e re ce nt International Boundary !ª !ª Ahferom Sudan Tahtay Erob fire incid ent in Keft a hum era woreda. I nhabitan ts Laelay Ahferom !ª Regional Boundary > Mereb Leke " !ª S are repo rted to be lef t out o f sh elter; UNI CEF !ª Adiyabo Adiyabo Gulomekeda W W W 7 Dalul E !Ò Laelay togethe r w ith the regiona l g ove rnm ent is Zonal Boundary North Western A Kafta Humera Maychew Eastern !ª sup portin g the victim s with provision o f wate r Measle Cas es Woreda Boundary Central and oth er imm ediate n eeds Measles co ntinues to b e re ported > Western Berahle with new four cases in Arada Zone 2 Lakes WBN BN Tsel emt !A !ª A! Sub-city,Ad dis Ababa ; and one Addi Arekay> W b Afa r Region N b Afdera Military Operation BeyedaB Ab Ala ! case in Ahfe rom woreda, Tig ray > > bb The re a re d isplaced pe ople from fo ur A Debark > > b o N W b B N Abergele Erebtoi B N W Southern keb eles of Mille and also five kebeles B N Janam ora Moegale Bidu Dabat Wag HiomraW B of Da llol woreda s (400 0 persons) a ff ected Hot Spot Areas AWD C ases N N N > N > B B W Sahl a B W > B N W Raya A zebo due to flo oding from Awash rive r an d ru n Since t he beg in nin g of th e year, Wegera B N No Data/No Humanitarian Concern > Ziquala Sekota B a total of 967 cases of AWD w ith East bb BN > Teru > off fro m Tigray highlands, respective ly. -

Final Report1
PROJECT REPORT To: Austrian Development Agency NGO Cooperation and Humanitarian Aid Zelinkagasse 2, 1010 Vienna E-mail: [email protected] Project progress reports are to be presented by e-mail as contractually agreed. Originals of additional documents can be sent to the NGO Cooperation desk. Final Report1 Contract number: 2679-00/2016 Contract partner in Austria Local project partner Name: Name: CARE Österreich CARE Ethiopia Address: Address: Lange Gasse 30/4, 1080 Vienna, Austria Telephone, e-mail: Telephone, e-mail: +43 1 715 0 715 +251 911 237 582 [email protected] +251911819687 Project officer/contact: Project officer/contact: Stéphanie Bouriel Teyent Taddesse [email protected] [email protected] Worku Abebaw [email protected] Project title: Emergency Seed Support to Smallholder Drought- Affected Farmers in South Gondar Ethiopia Country: Ethiopia Region/place: Amhara /South Gondar Duration from: 29 Feb 2016 to: 30 November 2016 Report as at (date):November 30, 2016 submitted on: March 7, 2017 Invoicing as at (date) in euros Submitted for Total project costs Invoiced to date Outstanding verification as at (date) 430,000 EURO 424,598.14 EURO 424.598,14 EURO 5.401,86 Date, report written by CARE Ethiopia, February 2017 1 Delete as applicable NGO individual projects– version: January 2009 | 1 PROJECT REPORT 1. Brief description of project progress2 (German, max. 1 page) A drought due to the effect of El Niño phenomenon had impacted 10.2 million people in various regions of Ethiopia. South Gonder administrative zone located in Amhara region and comprising seven livelihood zones, was amongst the areas most affected. -
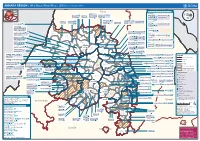
AMHARA REGION : Who Does What Where (3W) (As of 13 February 2013)
AMHARA REGION : Who Does What Where (3W) (as of 13 February 2013) Tigray Tigray Interventions/Projects at Woreda Level Afar Amhara ERCS: Lay Gayint: Beneshangul Gumu / Dire Dawa Plan Int.: Addis Ababa Hareri Save the fk Save the Save the df d/k/ CARE:f k Save the Children:f Gambela Save the Oromia Children: Children:f Children: Somali FHI: Welthungerhilfe: SNNPR j j Children:l lf/k / Oxfam GB:af ACF: ACF: Save the Save the af/k af/k Save the df Save the Save the Tach Gayint: Children:f Children: Children:fj Children:l Children: l FHI:l/k MSF Holand:f/ ! kj CARE: k Save the Children:f ! FHI:lf/k Oxfam GB: a Tselemt Save the Childrenf: j Addi Dessie Zuria: WVE: Arekay dlfk Tsegede ! Beyeda Concern:î l/ Mirab ! Concern:/ Welthungerhilfe:k Save the Children: Armacho f/k Debark Save the Children:fj Kelela: Welthungerhilfe: ! / Tach Abergele CRS: ak Save the Children:fj ! Armacho ! FHI: Save the l/k Save thef Dabat Janamora Legambo: Children:dfkj Children: ! Plan Int.:d/ j WVE: Concern: GOAL: Save the Children: dlfk Sahla k/ a / f ! ! Save the ! Lay Metema North Ziquala Children:fkj Armacho Wegera ACF: Save the Children: Tenta: ! k f Gonder ! Wag WVE: Plan Int.: / Concern: Save the dlfk Himra d k/ a WVE: ! Children: f Sekota GOAL: dlf Save the Children: Concern: Save the / ! Save: f/k Chilga ! a/ j East Children:f West ! Belesa FHI:l Save the Children:/ /k ! Gonder Belesa Dehana ! CRS: Welthungerhilfe:/ Dembia Zuria ! î Save thedf Gaz GOAL: Children: Quara ! / j CARE: WVE: Gibla ! l ! Save the Children: Welthungerhilfe: k d k/ Takusa dlfj k -

English-Full (0.5
Enhancing the Role of Forestry in Building Climate Resilient Green Economy in Ethiopia Strategy for scaling up effective forest management practices in Amhara National Regional State with particular emphasis on smallholder plantations Wubalem Tadesse Alemu Gezahegne Teshome Tesema Bitew Shibabaw Berihun Tefera Habtemariam Kassa Center for International Forestry Research Ethiopia Office Addis Ababa October 2015 Copyright © Center for International Forestry Research, 2015 Cover photo by authors FOREWORD This regional strategy document for scaling up effective forest management practices in Amhara National Regional State, with particular emphasis on smallholder plantations, was produced as one of the outputs of a project entitled “Enhancing the Role of Forestry in Ethiopia’s Climate Resilient Green Economy”, and implemented between September 2013 and August 2015. CIFOR and our ministry actively collaborated in the planning and implementation of the project, which involved over 25 senior experts drawn from Federal ministries, regional bureaus, Federal and regional research institutes, and from Wondo Genet College of Forestry and Natural Resources and other universities. The senior experts were organised into five teams, which set out to identify effective forest management practices, and enabling conditions for scaling them up, with the aim of significantly enhancing the role of forests in building a climate resilient green economy in Ethiopia. The five forest management practices studied were: the establishment and management of area exclosures; the management of plantation forests; Participatory Forest Management (PFM); agroforestry (AF); and the management of dry forests and woodlands. Each team focused on only one of the five forest management practices, and concentrated its study in one regional state. -

Ethiopia: Amhara Region Administrative Map (As of 05 Jan 2015)
Ethiopia: Amhara region administrative map (as of 05 Jan 2015) ! ! ! ! ! ! ! ! ! ! Abrha jara ! Tselemt !Adi Arikay Town ! Addi Arekay ! Zarima Town !Kerakr ! ! T!IGRAY Tsegede ! ! Mirab Armacho Beyeda ! Debark ! Debarq Town ! Dil Yibza Town ! ! Weken Town Abergele Tach Armacho ! Sanja Town Mekane Berhan Town ! Dabat DabatTown ! Metema Town ! Janamora ! Masero Denb Town ! Sahla ! Kokit Town Gedebge Town SUDAN ! ! Wegera ! Genda Wuha Town Ziquala ! Amba Giorges Town Tsitsika Town ! ! ! ! Metema Lay ArmachoTikil Dingay Town ! Wag Himra North Gonder ! Sekota Sekota ! Shinfa Tomn Negade Bahr ! ! Gondar Chilga Aukel Ketema ! ! Ayimba Town East Belesa Seraba ! Hamusit ! ! West Belesa ! ! ARIBAYA TOWN Gonder Zuria ! Koladiba Town AMED WERK TOWN ! Dehana ! Dagoma ! Dembia Maksegnit ! Gwehala ! ! Chuahit Town ! ! ! Salya Town Gaz Gibla ! Infranz Gorgora Town ! ! Quara Gelegu Town Takusa Dalga Town ! ! Ebenat Kobo Town Adis Zemen Town Bugna ! ! ! Ambo Meda TownEbinat ! ! Yafiga Town Kobo ! Gidan Libo Kemkem ! Esey Debr Lake Tana Lalibela Town Gomenge ! Lasta ! Muja Town Robit ! ! ! Dengel Ber Gobye Town Shahura ! ! ! Wereta Town Kulmesk Town Alfa ! Amedber Town ! ! KUNIZILA TOWN ! Debre Tabor North Wollo ! Hara Town Fogera Lay Gayint Weldiya ! Farta ! Gasay! Town Meket ! Hamusit Ketrma ! ! Filahit Town Guba Lafto ! AFAR South Gonder Sal!i Town Nefas mewicha Town ! ! Fendiqa Town Zege Town Anibesema Jawi ! ! ! MersaTown Semen Achefer ! Arib Gebeya YISMALA TOWN ! Este Town Arb Gegeya Town Kon Town ! ! ! ! Wegel tena Town Habru ! Fendka Town Dera -

July 31, 2018
Food for the Hungry Ethiopia Development Food Security Activity Targeted Response for Agriculture, Income and Nutrition Project Year II Third Quarter Report April 1 to June 30, 2018 Submission Date: July 31, 2018 [Contract/Agreement] Number: [AID-FFP-A-16-00007] Activity Start Date and End Date: Sep 30, 2016 – Sep 29, 2021 [COR/AOR] Name: Cliff Davison Submitted by: Anthony E. Koomson Senior Director for Public Resources 1001 Connecticut Ave NW Suite 1115, Washington, DC 20036 Tel: 202-480-2540 Email: [email protected] 1. PROJECT OVERVIEW/SUMMARY Targeted Response for Agriculture, Income and Nutrition Program Name: Activity Start Date And End Date: Sep 30, 2016 – Sep 29, 2021 Name of Prime Implementing Partner: Food for the Hungry [Contract/Agreement] Number: AID-FFP-A-16-00007 Name of Subcontractors/Sub- Amhara Credit and Saving Institution, Amhara Development awardees: Association, and Search For Common Ground Major Counterpart Organizations Regional, Zonal and District level Government Line Offices Ethiopia, Amhara Regional State, Seven Districts [Lay Gayint, Geographic Coverage Tach Gayint, Sedi-Muja, Simada, Abergele, Sahila and Ziquala. Reporting Period: April 1 to June 30, 2018 ii Table of Contents 1. PROJECT OVERVIEW/SUMMARY .............................................................................................................. II LIST OF TABLES AND FIGURES ............................................................................................................................ III ACRONYMS AND ABBREVIATIONS ................................................................................................................... -

Fh-Ethiopia Development Food Security Activity- Targeted Response for Agriculture, Income and Nutrition
MOBILE CASH TRANSFER PILOT FOR PSNP CLIENTS IN LAY GAYINT AND TACH GAYINT WOREDAS OF AMHARA REGION, ETHIOPIA FH ETHIOPIA DEVELOPMENT FOOD SECURITY ACTIVITY FH-ETHIOPIA DEVELOPMENT FOOD SECURITY ACTIVITY- TARGETED RESPONSE FOR AGRICULTURE, INCOME AND NUTRITION SEPTEMBER, 2018 ADDIS ABABA 0 ACKNOWLEDGEMENT Thanks to the June 2018 Amhara Region PSNP Joint Review and Implementation Support (JRIS) meeting participants who raised critical questions on the overall cash transfer with special emphasis on e- payment which contributed to the scope of this study. We are grateful for Woreda and Zonal Food Security (FS) and Amhara Credit and Saving Institute (ACSI) branch offices for providing data on list of unpaid clients and the unpaid amount of cash in Lay Gayint Woreda. Lay Gayint Woreda FS has also provided assessment result on why clients didn’t collect their entitlements. Special thanks to FH field staff in the two Woredas for their unreserved effort to interview clients and conduct Focus Group Discussions (FGDs) with Kebele administration and e-payment steering committee members. We are highly indebted to Productive Safety Net Program (PSNP) clients who participated in the survey interview and made this study possible. Cover page picture: Cash transfer transaction between ACSI cashier and a PW participant in Tach Gayint Woreda Agat Kebele. 1 ACRONYMS ACSI Amhara Credit and Saving Institute ADA Amhara Development Association BCC Behavioral Change Communication DA Development Agent FDRE Federal Democratic Republic of Ethiopia FGD Focus Group -

Impacts of Smallholder Tree Plantation in Amhara Region of Ethiopia: the Case of Lay Gayint and Fagta Locuma Districts1
Impacts of Smallholder Tree Plantation in Amhara Region of Ethiopia: The Case of Lay Gayint and Fagta Locuma Districts1 Fentahun Addis2, Surafel Melak3, Berihun Tefera4 and Habtemariam Kassa5 Abstract This study analyzes the impacts of smallholder plantation on the households’ total cash income, modern agricultural input use, education and health care spending of 300 sampled households in Lay Gayint and Fagta Locuma district’s of the Amhara Region, Ethiopia. A propensity score matching (PSM) analytical model has been used to examine the impacts of smallholder plantation on total cash income, improved agricultural input use, educational and health care expenditure. The PSM tool confirmed that, participation in to tree plantation had a significant impact on farm households total cash income, education and health expenditure outcome. However, it does not have a significant impact on the use of modern agricultural inputs. The findings of this study calls for the scale up of best practices of smallholder plantation in Amhara region and in Ethiopia at large. In addition, concerns have to be given in improving land productivity, educational level of farm households, and increasing market access and linkages, value addition of plantation products, expansion of infrastructures especially road and telecommunication networks in the rural parts to raise participation in plantation. Key words: plantation, propensity score matching, planter, non-planter, impact analysis JEL Classification: Q23, C99, DO2, C91, C18 1 We thank the Center for International Forestry Research (CIFOR) for financing this research project. The helpful comments and suggestions of two anonymous referees are gratefully acknowledged. Any remaining errors are ours. 2 Lecturer, Department of Economics, Bahir Dar University; Corresponding Author. -

Ethiopia Humanitarian Fund 2016 Annual Report
2016 Annual Report Ethiopia Humanitarian Fund Ethiopia Humanitarian Fund 2016 Annual Report TABLE of CONTENTS Forward by the Humanitarian Coordinator 04 Dashboard – Visual Overview 05 Humanitarian Context 06 Allocation Overview 07 Fund Performance 09 Donor Contributions 12 Annexes: Summary of results by Cluster Map of allocations Ethiopia Humanitarian Fund projects funded in 2016 Acronyms Useful Links 1 REFERENCE MAP N i l e SAUDI ARABIA R e d ERITREA S e a YEMEN TIGRAY SUDAN Mekele e z e k e T Lake Tana AFAR DJIBOUTI Bahir Dar Gulf of Aden Asayita AMHARA BENESHANGUL Abay GUMU Asosa Dire Dawa Addis Ababa Awash Hareri Ji Jiga Gambela Nazret (Adama) GAMBELA A EETHIOPIAT H I O P I A k o b o OROMIA Awasa Omo SOMALI SOUTH S SNNPR heb SUDAN ele le Gena Ilemi Triangle SOMALIA UGANDA KENYA INDIAN OCEAN 100 km National capital Regional capital The boundaries and names shown and the designations International boundary used on this map do not imply official endorsement or Region boundary acceptance by the United Nations. Final boundary River between the Republic of Sudan and the Republic of Lake South Sudan has not yet been determined. 2 I FOREWORD DASHBOARD 3 FOREWORD FOREWORD BY THE HUMANITARIAN COORDINATOR In 2016, Ethiopia continued to battle the 2015/2016 El Niño-induced drought; the worst drought to hit the country in fifty years. More than 10.2 million people required relief food assistance at the peak of the drought in April. To meet people’s needs, the Government of Ethiopia and humanitar- ian partners issued an initial appeal for 2016 of US$1.4 billion, which increased to $1.6 billion in August. -

Intestinal Parasite Prevalence in an Area of Ethiopia After Implementing the SAFE Strategy, Enhanced Outreach Services, and Health Extension Program
Intestinal Parasite Prevalence in an Area of Ethiopia after Implementing the SAFE Strategy, Enhanced Outreach Services, and Health Extension Program Jonathan D. King1,2,3*, Tekola Endeshaw4, Elisabeth Escher3,5, Genetu Alemtaye6, Sileabatt Melaku6, Woyneshet Gelaye6, Abebe Worku7, Mitku Adugna4, Berhanu Melak4, Tesfaye Teferi4, Mulat Zerihun4, Demelash Gesese4, Zerihun Tadesse4, Aryc W. Mosher1, Peter Odermatt2,3,Ju¨ rg Utzinger2,3, Hanspeter Marti3,5, Jeremiah Ngondi1,8, Donald R. Hopkins1, Paul M. Emerson1 1 The Carter Center, Atlanta, Georgia, United States of America, 2 Department of Epidemiology and Public Health, Swiss Tropical and Public Health Institute, Basel, Switzerland, 3 University of Basel, Basel, Switzerland, 4 The Carter Center, Addis Ababa, Ethiopia, 5 Department of Medical Services and Diagnostic, Swiss Tropical and Public Health Institute, Basel, Switzerland, 6 Amhara Regional Research Laboratory, Amhara National Regional State Health Bureau, Bahir Dar, Ethiopia, 7 South Gondar Zonal Health Department, Amhara National Regional State Health Bureau, Debre Tabor, Ethiopia, 8 Department of Public Health and Primary Care, Institute of Public Health, University of Cambridge, Cambridge, United Kingdom Abstract Background: The SAFE strategy aims to reduce transmission of Chlamydia trachomatis through antibiotics, improved hygiene, and sanitation. We integrated assessment of intestinal parasites into large-scale trachoma impact surveys to determine whether documented environmental improvements promoted by a trachoma program had collateral impact on intestinal parasites. Methodology: We surveyed 99 communities for both trachoma and intestinal parasites (soil-transmitted helminths, Schistosoma mansoni, and intestinal protozoa) in South Gondar, Ethiopia. One child aged 2–15 years per household was randomly selected to provide a stool sample of which about 1 g was fixed in sodium acetate-acetic acid-formalin, concentrated with ether, and examined under a microscope by experienced laboratory technicians. -

Bahir Dar University College of Agriculture and Environmental Sciences
BAHIR DAR UNIVERSITY COLLEGE OF AGRICULTURE AND ENVIRONMENTAL SCIENCES GRADUATE PROGRAM PHENOTYPIC CHARACTERIZATION OF INDIGENOUS SHEEP AND FARMERS’ BREEDING OBJECTIVES IN THREE SELECTED DISTRICTS OF SOUTH WOLLO ZONE, ETHIOPIA M.Sc. Thesis By Moges Takele Teshale Department: Animal Production and Technology, Program: MSc. in Animal Genetics and Breeding Major Advisor: Yeshambel Mekuriaw (PhD) Co-advisor: Solomon Gizaw (PhD) June, 2016 Bahir Dar BAHIR DAR UNIVERSITY COLLEGE OF AGRICULTURE AND ENVIRONMENTAL SCIENCES GRADUATE PROGRAM PHENOTYPIC CHARACTERIZATION OF INDIGENOUS SHEEP AND FARMERS' BREEDING OBJECTIVES IN THREE SELECTED DISTRICTS OF SOUTH WOLLO ZONE, ETHIOPIA M.sc. Thesis By Moges Takele Teshale SUBMITTED IN PARTIAL FULFILLMENT OF THE REQUIREMENTS FOR THE DEGREE OF MASTER OF SCIENCE (M.Sc.) IN ANIMAL GENETICS AND BREEDING June, 2016 Bahir Dar University THESIS APPROVAL SHEET As member of the Board of Examiners of the Master of Sciences (M.Sc.) thesis open defense examination, we have read and evaluated this thesis prepared by Moges Takele Teshale entitled ‘phenotypic characterization of indigenous sheep and farmers’ breeding objectives in three selected districts of south Wollo Zone, Ethiopia’. We hereby certify that, the thesis is accepted for fulfilling the requirements for the award of the degree of Master of Sciences (M.Sc.) in Animal Genetics and Breeding. Board of Examiners Name of External Examiner Signature Date ------------------------------ ________________----------------_________ _ ------------ _________________ ______________ -

1. Summary COMPILED by DISASTER RISK REDUCTION PROGRAM DEPARTMENT
Quarter FS Situation & Early Warning Report (July - September 2015) FH – ETHIOPIA, DISASTER RISK REDUCTION PROGRAM (DRRP) DEPARTMENT In the Quarter: Impact of El Nino has resulted in water stress in a substantial scale in the lowlands of South Gondar and Wag Humra zones, causing a number of water sources to dry earlier than normal times According to the Central Statistics Agency of Ethiopia; Ethiopian inflation rate had peaked to 11.9 percent as compared to last year in 1. SummarySeptember from 11.6 percent, because of a rise in food items. Food price inflation had peaked from 1.114.7 General percent Overview a month ago to 16.1 percent, Theaccording early warning to the Agency.report of Oct the 7, quarter 2015 (July - September 2015) is summarized based on reports from currently ongoing FHE project areas of Amhara, SNNP, Oromia, and Benishangul Gumuz Regional States; and from the articles and bulletins of FEWS NET, Food Security updates, etc… The aim of preparing this report is to update partners on the prevailing food security situation at FHE intervention areas and give alert for preparedness and possible responses required. The report briefly includes the weather condition, market performances, health and nutrition and food security situation within the quarter (July - September 2015). COMPILED BY DISASTER RISK 1.2 Major Highlights towardsREDUCTION the end of July 2015,PROGRAM which forced In normal crop production years, the meher farmers to plant crops beyond the planting DEPARTMENT rain usually starts at the beginning of June season. Accordingly, the amount and that enables farmers to start planting meher distribution of rainfall had been much below crops timely and it continues up to the normal within most of the project area month of October for the normal maturity of woredas in the reporting period except Belo, crops.