Overview of the Immune System and Immunological Assays with Real World Connections
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-
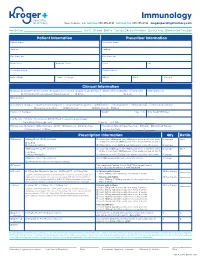
Immunology New Orleans, LA Toll Free 888.355.4191 Toll Free Fax 888.355.4192 Krogerspecialtypharmacy.Com
Immunology New Orleans, LA toll free 888.355.4191 toll free fax 888.355.4192 krogerspecialtypharmacy.com Need By Date: _________________________________________________ Ship To: Patient Office Fax Copy: Rx Card Front/Back Clinical Notes Medical Card Front/Back Patient Information Prescriber Information Patient Name Prescriber Name Address Address City State Zip City State Zip Main Phone Alternate Phone Phone Fax Social Security # Contact Person Date of Birth Male Female DEA # NPI # License # Clinical Information Diagnosis: J45.40 Moderate Asthma J45.50 Severe Asthma L20.9 Atopic Dermatitis L50.1 Chronic Idiopathic Urticaria (CIU) Eosinophil Levels J33 Chronic Rhinosinusitis with Nasal Polyposis Other: ________________________________ Dx Code: ___________ Drug Allergies Concomitant Therapies: Short-acting Beta Agonist Long-acting Beta Agonist Antihistamines Decongestants Immunotherapy Inhaled Corticosteroid Leukotriene Modifiers Oral Steroids Nasal Steroids Other: _____________________________________________________________ Please List Therapies Weight kg lbs Date Weight Obtained Lab Results: History of positive skin OR RAST test to a perennial aeroallergen Pretreatment Serum lgE Level: ______________________________________ IU per mL Test Date: _________ / ________ / ________ MD Specialty: Allergist Dermatologist ENT Pediatrician Primary Care Prescription Type: Naïve/New Start Restart Continued Therapy Pulmonologist Other: _________________________________________ Last Injection Date: _________ / ________ -
IFM Innate Immunity Infographic
UNDERSTANDING INNATE IMMUNITY INTRODUCTION The immune system is comprised of two arms that work together to protect the body – the innate and adaptive immune systems. INNATE ADAPTIVE γδ T Cell Dendritic B Cell Cell Macrophage Antibodies Natural Killer Lymphocites Neutrophil T Cell CD4+ CD8+ T Cell T Cell TIME 6 hours 12 hours 1 week INNATE IMMUNITY ADAPTIVE IMMUNITY Innate immunity is the body’s first The adaptive, or acquired, immune line of immunological response system is activated when the innate and reacts quickly to anything that immune system is not able to fully should not be present. address a threat, but responses are slow, taking up to a week to fully respond. Pathogen evades the innate Dendritic immune system T Cell Cell Through antigen Pathogen presentation, the dendritic cell informs T cells of the pathogen, which informs Macrophage B cells B Cell B cells create antibodies against the pathogen Macrophages engulf and destroy Antibodies label invading pathogens pathogens for destruction Scientists estimate innate immunity comprises approximately: The adaptive immune system develops of the immune memory of pathogen exposures, so that 80% system B and T cells can respond quickly to eliminate repeat invaders. IMMUNE SYSTEM AND DISEASE If the immune system consistently under-responds or over-responds, serious diseases can result. CANCER INFLAMMATION Innate system is TOO ACTIVE Innate system NOT ACTIVE ENOUGH Cancers grow and spread when tumor Certain diseases trigger the innate cells evade detection by the immune immune system to unnecessarily system. The innate immune system is respond and cause excessive inflammation. responsible for detecting cancer cells and This type of chronic inflammation is signaling to the adaptive immune system associated with autoimmune and for the destruction of the cancer cells. -

White Blood Cells and Severe COVID-19: a Mendelian Randomization Study
Journal of Personalized Medicine Article White Blood Cells and Severe COVID-19: A Mendelian Randomization Study Yitang Sun 1 , Jingqi Zhou 1,2 and Kaixiong Ye 1,3,* 1 Department of Genetics, Franklin College of Arts and Sciences, University of Georgia, Athens, GA 30602, USA; [email protected] (Y.S.); [email protected] (J.Z.) 2 School of Public Health, Shanghai Jiao Tong University School of Medicine, Shanghai 200025, China 3 Institute of Bioinformatics, University of Georgia, Athens, GA 30602, USA * Correspondence: [email protected]; Tel.: +1-706-542-5898; Fax: +1-706-542-3910 Abstract: Increasing evidence shows that white blood cells are associated with the risk of coronavirus disease 2019 (COVID-19), but the direction and causality of this association are not clear. To evaluate the causal associations between various white blood cell traits and the COVID-19 susceptibility and severity, we conducted two-sample bidirectional Mendelian Randomization (MR) analyses with summary statistics from the largest and most recent genome-wide association studies. Our MR results indicated causal protective effects of higher basophil count, basophil percentage of white blood cells, and myeloid white blood cell count on severe COVID-19, with odds ratios (OR) per standard deviation increment of 0.75 (95% CI: 0.60–0.95), 0.70 (95% CI: 0.54–0.92), and 0.85 (95% CI: 0.73–0.98), respectively. Neither COVID-19 severity nor susceptibility was associated with white blood cell traits in our reverse MR results. Genetically predicted high basophil count, basophil percentage of white blood cells, and myeloid white blood cell count are associated with a lower risk of developing severe COVID-19. -

"Epitope Mapping: B-Cell Epitopes". In: Encyclopedia of Life Sciences
Epitope Mapping: B-cell Advanced article Epitopes Article Contents . Introduction GE Morris, Wolfson Centre for Inherited Neuromuscular Disease RJAH Orthopaedic Hospital, . What Is a B-cell Epitope? . Epitope Mapping Methods Oswestry, UK and Keele University, Keele, Staffordshire, UK . Applications Immunoglobulin molecules are folded to present a surface structure complementary to doi: 10.1002/9780470015902.a0002624.pub2 a surface feature on the antigen – the epitope is this feature of the antigen. Epitope mapping is the process of locating the antibody-binding site on the antigen, although the term is also applied more broadly to receptor–ligand interactions unrelated to the immune system. Introduction formed of highly convoluted peptide chains, so that resi- dues that lie close together on the protein surface are often Immunoglobulin molecules are folded in a way that as- far apart in the amino acid sequence (Barlow et al., 1986). sembles sequences from the variable regions of both the Consequently, most epitopes on native, globular proteins heavy and light chains into a surface feature (comprised of are conformation-dependent and they disappear if the up to six complementarity-determining regions (CDRs)) protein is denatured or fragmented. Sometimes, by acci- that is complementary in shape to a surface structure on the dent or design, antibodies are produced against linear antigen. These two surface features, the ‘paratope’ on the (sequential) epitopes that survive denaturation, though antibody and the ‘epitope’ on the antigen, may have a cer- such antibodies usually fail to recognize the native protein. tain amount of flexibility to allow an ‘induced fit’ between The simplest way to find out whether an epitope is confor- them. -

We Work at the Intersection of Immunology and Developmental Biology
Development and Homeostasis of Mucosal Tissues U934/UMR3215 – Genetics and Developmental Biology Pedro Hernández Chef d'équipe [email protected] We work at the intersection of immunology and developmental biology. Our primary goal is to understand how immune responses impact the development, integrity and function of mucosal tissue layers, such as the intestinal epithelium, during homeostasis and upon different types of stress, including infections. To study these questions we exploit the advantages of the zebrafish model such as ex utero and rapid development, transparency, large progeny, and simple genetic manipulation. We combine live imaging, flow cytometry, single-cell transcriptomics, and models inducing mucosal stress, including pathogenic challenges. Our research can be subdivided into three main topics: 1) Protection of intestinal epithelial integrity since early development: Epithelial cells are at the core of intestinal organ function. They are in charge of absorbing nutrients and water, and at the same time constitute a barrier for potential pathogens and harmful molecules. Epithelial cells perform all these functions before full development of the immune system, which promotes epithelial barrier function upon injury. We study how robust epithelial integrity is achieved prior and after maturation of the intestinal immune system, with a focus on the function of mucosal cytokines. 2) Epithelial-leukocyte crosstalk throughout development: Intestines become vastly populated by leukocytes after exposure to external cues from diet and colonization by the microbiota. We have recently reported the existence and diversity of zebrafish innate lymphoid cells (ILCs), a key component of the mucosal immune system recently discovered in mice and humans. ILCs mediate immune responses by secreting cytokines such as IL-22 which safeguards gut epithelial integrity. -

Ten Years of Lateral Flow Immunoassay Technique Applications: Trends, Challenges and Future Perspectives
sensors Review Ten Years of Lateral Flow Immunoassay Technique Applications: Trends, Challenges and Future Perspectives Fabio Di Nardo * , Matteo Chiarello , Simone Cavalera , Claudio Baggiani and Laura Anfossi Department of Chemistry, University of Torino, 10125 Torino, Italy; [email protected] (M.C.); [email protected] (S.C.); [email protected] (C.B.); [email protected] (L.A.) * Correspondence: [email protected] Abstract: The Lateral Flow Immunoassay (LFIA) is by far one of the most successful analytical platforms to perform the on-site detection of target substances. LFIA can be considered as a sort of lab-in-a-hand and, together with other point-of-need tests, has represented a paradigm shift from sample-to-lab to lab-to-sample aiming to improve decision making and turnaround time. The features of LFIAs made them a very attractive tool in clinical diagnostic where they can improve patient care by enabling more prompt diagnosis and treatment decisions. The rapidity, simplicity, relative cost-effectiveness, and the possibility to be used by nonskilled personnel contributed to the wide acceptance of LFIAs. As a consequence, from the detection of molecules, organisms, and (bio)markers for clinical purposes, the LFIA application has been rapidly extended to other fields, including food and feed safety, veterinary medicine, environmental control, and many others. This review aims to provide readers with a 10-years overview of applications, outlining the trends for the main application fields and the relative compounded annual growth rates. Moreover, future perspectives and challenges are discussed. Citation: Di Nardo, F.; Chiarello, M.; Cavalera, S.; Baggiani, C.; Anfossi, L. -

Comparison of Immunohistochemistry with Immunoassay (ELISA
British Journal of Cancer (1999) 79(9/10), 1534–1541 © 1999 Cancer Research Campaign Article no. bjoc.1998.0245 Comparison of immunohistochemistry with immunoassay (ELISA) for the detection of components of the plasminogen activation system in human tumour tissue CM Ferrier1, HH de Witte2, H Straatman3, DH van Tienoven2, WL van Geloof1, FJR Rietveld1, CGJ Sweep2, DJ Ruiter1 and GNP van Muijen1 Departments of 1Pathology, 2Chemical Endocrinology and 3Epidemiology, University Hospital Nijmegen, PO Box 9101, 6500 HB Nijmegen, The Netherlands Summary Enzyme-linked immunosorbent assay (ELISA) methods and immunohistochemistry (IHC) are techniques that provide information on protein expression in tissue samples. Both methods have been used to investigate the impact of the plasminogen activation (PA) system in cancer. In the present paper we first compared the expression levels of uPA, tPA, PAI-1 and uPAR in a compound group consisting of 33 cancer lesions of various origin (breast, lung, colon, cervix and melanoma) as quantitated by ELISA and semi-quantitated by IHC. Secondly, the same kind of comparison was performed on a group of 23 melanoma lesions and a group of 28 breast carcinoma lesions. The two techniques were applied to adjacent parts of the same frozen tissue sample, enabling the comparison of results obtained on material of almost identical composition. Spearman correlation coefficients between IHC results and ELISA results for uPA, tPA, PAI-1 and uPAR varied between 0.41 and 0.78, and were higher for the compound group and the breast cancer group than for the melanoma group. Although a higher IHC score category was always associated with an increased median ELISA value, there was an overlap of ELISA values from different scoring classes. -

Immunoassay - Elisa
IMMUNOASSAY - ELISA PHUBETH YA-UMPHAN National Institute of Health, Department of Medical Sciences 0bjective After this presentation, participants will be able to Explain how an ELISA test determines if a person has certain antigens or antibodies . Explain the process of conducting an ELISA test. Explain interactions that take place at the molecular level (inside the microtiter well) during an ELISA test. Outline - Principal of immunoassay - Classification of immunoassay Type of ELISA - ELISA ELISA Reagents General - Applications Principal of ELISA ELISA workflow What is immunoassay? Immunoassays are bioanalytical methods that use the specificity of an antigen-antibody reaction to detect and quantify target molecules in biological samples. Specific antigen-antibody recognition Principal of immunoassay • Immunoassays rely on the inherent ability of an antibody to bind to the specific structure of a molecule. • In addition to the binding of an antibody to its antigen, the other key feature of all immunoassays is a means to produce a measurable signal in response to the binding. Classification of Immunoassays Immunoassays can be classified in various ways. Unlabeled Labeled Competitive Homogeneous Noncompetitive Competitive Heterogeneous Noncompetitive https://www.sciencedirect.com/science/article/pii/S0075753508705618 Classification of Immunoassays • Unlabeled - Immunoprecipitation • Labeled Precipitation of large cross-linked Ag-Ab complexes can be visible to the naked eyes. - Fluoroimmnoassay (FIA) - Radioimmunoassay (RIA) - Enzyme Immunoassays (EIA) - Chemiluminescenceimmunoassay(CLIA) - Colloidal Gold Immunochromatographic Assay (ICA) https://www.creative-diagnostics.com/Immunoassay.htm Classification of Immunoassays • Homogeneous immunoassays Immunoassays that do not require separation of the bound Ag-Ab complex. (Does not require wash steps to separate reactants.) Example: Home pregnancy test. • Heterogeneous immunoassays Immunoassays that require separation of the bound Ag-Ab complex. -

Our Immune System (Children's Book)
OurOur ImmuneImmune SystemSystem A story for children with primary immunodeficiency diseases Written by IMMUNE DEFICIENCY Sara LeBien FOUNDATION A note from the author The purpose of this book is to help young children who are immune deficient to better understand their immune system. What is a “B-cell,” a “T-cell,” an “immunoglobulin” or “IgG”? They hear doctors use these words, but what do they mean? With cheerful illustrations, Our Immune System explains how a normal immune system works and what treatments may be necessary when the system is deficient. In this second edition, a description of a new treatment has been included. I hope this book will enable these children and their families to explore together the immune system, and that it will help alleviate any confusion or fears they may have. Sara LeBien This book contains general medical information which cannot be applied safely to any individual case. Medical knowledge and practice can change rapidly. Therefore, this book should not be used as a substitute for professional medical advice. SECOND EDITION COPYRIGHT 1990, 2007 IMMUNE DEFICIENCY FOUNDATION Copyright 2007 by Immune Deficiency Foundation, USA. Readers may redistribute this article to other individuals for non-commercial use, provided that the text, html codes, and this notice remain intact and unaltered in any way. Our Immune System may not be resold, reprinted or redistributed for compensation of any kind without prior written permission from Immune Deficiency Foundation. If you have any questions about permission, please contact: Immune Deficiency Foundation, 40 West Chesapeake Avenue, Suite 308, Towson, MD 21204, USA; or by telephone at 1-800-296-4433. -

Immunology Stories: How Storytelling Can Help Us to Make Sense of Complex Topics
Immunology Stories: How Storytelling Can Help Us to Make Sense of Complex Topics Jennifer Giuliani, MSc Camosun College, Lansdowne Campus, 3100 Foul Bay Rd, Victoria BC V8P 5J2 [email protected] Abstract The immune response is a wonderfully complex aspect of our physiology that can sometimes confound students and instructors alike. How do we wade through the layers of detail to help our students develop an understanding of immunology? In this article, I will share some of the stories about immunology research that helped me strengthen my own understanding and improve my approach to helping students learn and understand this topic. In addition, we will explore some of the research on the power of storytelling, and how learning through stories might be a defining characteristic of what it means to be human. https://doi.org/10.21692/haps.2020.105 Key words: storytelling, immunology Introduction I have been trying to understand the immune response for a My personal journey to develop a better understanding of long time. Like many Anatomy and Physiology instructors, I the immune system was a compelling reminder to me of the did not have an immunology background beyond what was power of storytelling. Suddenly I saw examples of storytelling covered in my undergraduate physiology courses. When the everywhere that I saw authentic learning. In this article, I will time came for me to teach students about the immune system, share some of what I have learned about learning through I relied heavily on the information presented in our textbooks. stories, some of the fun and fascinating immunology stories I was able to present students with the key pieces of from Davis’ books, and my current approach to helping information and help them to remember a few facts, and the students understand the immune response. -
Laboratory Techniques Used for Immunological Laboratory Methods
Laboratory techniques used for Immunological laboratory methods Dr. Tatiana Jones, MD, PhD NCC How to Make Serial Dilutions? Interpretation can be made differently depending on the nature of test. For example, if we need to figure out in what sample the concentration of the antibody or antigen is higher, we will go by TITER, which is the lowest serial dilution (let’s say that it is 1:32 in the picture on the left) that gives us positive result. This mean that even diluted 32 times sample is still capable of reacting. The other scenario when we are interpreting quantitative assays, such as ELISA. In this case we need to match results of our samples to known concentrations of STANDARD and MULTIPLY be our dilution factor. What is Antibody Titer? An antibody titer is a measurement of how much antibody an organism has produced that recognizes a particular antigen. Titer is expressed as the inverse of the greatest dilution that still gives a positive result. ELISA is a common means of determining antibody titers. How to Determine Antibody Titer? Where we can use Indirect Coombs test detects the presence of anti-Rh antibodies in blood serum. A patient might be reported to have an "indirect Antibody Titer? Coombs titer" of 16. This means that the patient's serum gives a positive indirect Coombs test at any dilution down to 1/16 (1 part serum to 15 parts diluent). At greater dilutions the indirect Coombs test is negative. If a few weeks later the same patient had an indirect Coombs titer of 32 (1/32 dilution which is 1 part serum to 31 parts diluent), this would mean that more anti-Rh antibody was made, since it took a greater dilution to eradicate the positive test. -

Defining Natural Antibodies
PERSPECTIVE published: 26 July 2017 doi: 10.3389/fimmu.2017.00872 Defining Natural Antibodies Nichol E. Holodick1*, Nely Rodríguez-Zhurbenko2 and Ana María Hernández2* 1 Department of Biomedical Sciences, Center for Immunobiology, Western Michigan University Homer Stryker M.D. School of Medicine, Kalamazoo, MI, United States, 2 Natural Antibodies Group, Tumor Immunology Division, Center of Molecular Immunology, Havana, Cuba The traditional definition of natural antibodies (NAbs) states that these antibodies are present prior to the body encountering cognate antigen, providing a first line of defense against infection thereby, allowing time for a specific antibody response to be mounted. The literature has a seemingly common definition of NAbs; however, as our knowledge of antibodies and B cells is refined, re-evaluation of the common definition of NAbs may be required. Defining NAbs becomes important as the function of NAb production is used to define B cell subsets (1) and as these important molecules are shown to play numerous roles in the immune system (Figure 1). Herein, we aim to briefly summarize our current knowledge of NAbs in the context of initiating a discussion within the field of how such an important and multifaceted group of molecules should be defined. Edited by: Keywords: natural antibody, antibodies, natural antibody repertoire, B-1 cells, B cell subsets, B cells Harry W. Schroeder, University of Alabama at Birmingham, United States NATURAL ANTIBODY (NAb) PRODUCING CELLS Reviewed by: Andre M. Vale, Both murine and human NAbs have been discussed in detail since the late 1960s (2, 3); however, Federal University of Rio cells producing NAbs were not identified until 1983 in the murine system (4, 5).