High-Resolution CISS MR Imaging with and Without Contrast for Evaluation of the Upper Cranial Nerves
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Cranial Nerve Palsy
Cranial Nerve Palsy What is a cranial nerve? Cranial nerves are nerves that lead directly from the brain to parts of our head, face, and trunk. There are 12 pairs of cranial nerves and some are involved in special senses (sight, smell, hearing, taste, feeling) while others control muscles and glands. Which cranial nerves pertain to the eyes? The second cranial nerve is called the optic nerve. It sends visual information from the eye to the brain. The third cranial nerve is called the oculomotor nerve. It is involved with eye movement, eyelid movement, and the function of the pupil and lens inside the eye. The fourth cranial nerve is called the trochlear nerve and the sixth cranial nerve is called the abducens nerve. They each innervate an eye muscle involved in eye movement. The fifth cranial nerve is called the trigeminal nerve. It provides facial touch sensation (including sensation on the eye). What is a cranial nerve palsy? A palsy is a lack of function of a nerve. A cranial nerve palsy may cause a complete or partial weakness or paralysis of the areas served by the affected nerve. In the case of a cranial nerve that has multiple functions (such as the oculomotor nerve), it is possible for a palsy to affect all of the various functions or only some of the functions of that nerve. What are some causes of a cranial nerve palsy? A cranial nerve palsy can occur due to a variety of causes. It can be congenital (present at birth), traumatic, or due to blood vessel disease (hypertension, diabetes, strokes, aneurysms, etc). -

MR Imaging of Primary Trochlear Nerve Neoplasms
707 MR Imaging of Primary Trochlear Nerve Neoplasms Lindell R. Gentry 1 We present the clinical, anatomic, and MR imaging findings in six patients with seven Rahul C. Mehta 1 primary trochlear nerve neoplasms, as well as the MR and clinical criteria that serve to Richard E. Appen2 establish the diagnosis of these rare cranial nerve neoplasms. Three patients had a Joel M. Weinstein2 history of neurofibromatosis and five patients had clinical evidence of a trochlear nerve palsy. Six of seven neoplasms produced localized, fusiform enlargement of the proximal cisternal segments of the trochlear nerves. The lesions that were visible on noncontrast MR scans (T1-, T2-, and proton density-weighted) had signal intensities that were virtually identical to normal brain parenchyma. All lesions showed intense, homogeneous enhancement on contrast-enhanced scans. Contrast-enhanced imaging was necessary for the detection of five of seven lesions and greatly increased the value of the MR study in all six patients. AJNR 12:707-713, July/August 1991; AJR 157: September 1991 Primary neoplasms arising from pure motor cranial nerves such as the trochlear nerve are rare. To our knowledge just nine primary trochlear nerve neoplasms have been reported in the literature [1-7), only one of which was imaged with MR [1). Over the last 6 years, since we began to use MR as the primary imaging method for evaluating patients with cranial nerve palsies , we have noticed a striking increase in the number of primary trochlear nerve neoplasms over those encountered during the CT era. We believe this is due to a much greater sensitivity of MR in detecting these typically small lesions. -

Cranial Nerve Disorders: Clinical Manifestations and Topographyଝ
Radiología. 2019;61(2):99---123 www.elsevier.es/rx UPDATE IN RADIOLOGY Cranial nerve disorders: Clinical manifestations and topographyଝ a,∗ a b c M. Jorquera Moya , S. Merino Menéndez , J. Porta Etessam , J. Escribano Vera , a M. Yus Fuertes a Sección de Neurorradiología, Hospital Clínico San Carlos, Madrid, Spain b Servicio de Neurología, Hospital Clínico San Carlos, Madrid, Spain c Neurorradiología, Hospital Ruber Internacional, Madrid, Spain Received 17 November 2017; accepted 27 September 2018 KEYWORDS Abstract The detection of pathological conditions related to the twelve cranial pairs rep- Cranial pairs; resents a significant challenge for both clinicians and radiologists; imaging techniques are Cranial nerves; fundamental for the management of many patients with these conditions. In addition to knowl- Cranial neuropathies; edge about the anatomy and pathological entities that can potentially affect the cranial pairs, Neuralgia; the imaging evaluation of patients with possible cranial pair disorders requires specific exami- Cranial nerve palsy nation protocols, acquisition techniques, and image processing. This article provides a review of the most common symptoms and syndromes related with the cranial pairs that might require imaging tests, together with a brief overview of the anatomy, the most common underlying processes, and the most appropriate imaging tests for different indications. © 2018 SERAM. Published by Elsevier Espana,˜ S.L.U. All rights reserved. PALABRAS CLAVE Sintomatología derivada de los pares craneales: Clínica y topografía Pares craneales; Resumen La detección de la patología relacionada con los doce pares craneales representa Nervios craneales; un importante desafío, tanto para los clínicos como para los radiólogos. Las técnicas de imagen Neuropatía de pares craneales; son fundamentales para el manejo de muchos de los pacientes. -

Clinical Anatomy of the Cranial Nerves Clinical Anatomy of the Cranial Nerves
Clinical Anatomy of the Cranial Nerves Clinical Anatomy of the Cranial Nerves Paul Rea AMSTERDAM • BOSTON • HEIDELBERG • LONDON NEW YORK • OXFORD • PARIS • SAN DIEGO SAN FRANCISCO • SINGAPORE • SYDNEY • TOKYO Academic Press is an imprint of Elsevier Academic Press is an imprint of Elsevier 32 Jamestown Road, London NW1 7BY, UK The Boulevard, Langford Lane, Kidlington, Oxford OX5 1GB, UK Radarweg 29, PO Box 211, 1000 AE Amsterdam, The Netherlands 225 Wyman Street, Waltham, MA 02451, USA 525 B Street, Suite 1800, San Diego, CA 92101-4495, USA First published 2014 Copyright r 2014 Elsevier Inc. All rights reserved. No part of this publication may be reproduced or transmitted in any form or by any means, electronic or mechanical, including photocopying, recording, or any information storage and retrieval system, without permission in writing from the publisher. Details on how to seek permission, further information about the Publisher’s permissions policies and our arrangement with organizations such as the Copyright Clearance Center and the Copyright Licensing Agency, can be found at our website: www.elsevier.com/permissions. This book and the individual contributions contained in it are protected under copyright by the Publisher (other than as may be noted herein). Notices Knowledge and best practice in this field are constantly changing. As new research and experience broaden our understanding, changes in research methods, professional practices, or medical treatment may become necessary. Practitioners and researchers must always rely on their own experience and knowledge in evaluating and using any information, methods, compounds, or experiments described herein. In using such information or methods they should be mindful of their own safety and the safety of others, including parties for whom they have a professional responsibility. -

Cranial Nerves
Cranial Nerves Cranial nerve evaluation is an important part of a neurologic exam. There are some differences in the assessment of cranial nerves with different species, but the general principles are the same. You should know the names and basic functions of the 12 pairs of cranial nerves. This PowerPage reviews the cranial nerves and basic brain anatomy which may be seen on the VTNE. The 12 Cranial Nerves: CN I – Olfactory Nerve • Mediates the sense of smell, observed when the pet sniffs around its environment CN II – Optic Nerve Carries visual signals from retina to occipital lobe of brain, observed as the pet tracks an object with its eyes. It also causes pupil constriction. The Menace response is the waving of the hand at the dog’s eye to see if it blinks (this nerve provides the vision; the blink is due to cranial nerve VII) CN III – Oculomotor Nerve • Provides motor to most of the extraocular muscles (dorsal, ventral, and medial rectus) and for pupil constriction o Observing pupillary constriction in PLR CN IV – Trochlear Nerve • Provides motor function to the dorsal oblique extraocular muscle and rolls globe medially © 2018 VetTechPrep.com • All rights reserved. 1 Cranial Nerves CN V – Trigeminal Nerve – Maxillary, Mandibular, and Ophthalmic Branches • Provides motor to muscles of mastication (chewing muscles) and sensory to eyelids, cornea, tongue, nasal mucosa and mouth. CN VI- Abducens Nerve • Provides motor function to the lateral rectus extraocular muscle and retractor bulbi • Examined by touching the globe and observing for retraction (also tests V for sensory) Responsible for physiologic nystagmus when turning head (also involves III, IV, and VIII) CN VII – Facial Nerve • Provides motor to muscles of facial expression (eyelids, ears, lips) and sensory to medial pinna (ear flap). -

Central Fourth Nerve Palsies Mitchell S.V
RESIDENT &FELLOW SECTION Pearls and Oy-sters: Section Editor Central fourth nerve palsies Mitchell S.V. Elkind, MD, MS Daniel R. Gold, DO CLINICAL PEARLS Lesions of the fourth (trochlear) Clinical features suggestive of bilateral fourth nerve Robert K. Shin, MD cranial nerve cause vertical or oblique diplopia by impair- palsies include right hypertropia in left gaze, left hyper- Steven Galetta, MD ing the ability of the superior oblique muscle to intort tropia in right gaze, and alternating hypertropia with and depress the eye. This binocular diplopia worsens in head tilt to either side (i.e., right hypertropia with right downgaze and lateral gaze away from the affected eye. tilt and left hypertropia with left head tilt).8 Correspondence & reprint Because intorsion is necessary to maintain fusion in ocu- requests to Dr. Gold: [email protected] lar counter-roll, this diplopia also worsens with head tilt CASE REPORTS Case 1. A20-year-oldmanpresented 1,2 toward the affected eye. to the emergency department complaining of 6 days of Diagnosis of a superior oblique palsy can be made binocular vertical diplopia and a left eyelid droop. He using the Parks-Bielschowsky 3-step test: 1) determine had noted fatigue, bilateral eye pain, and flu-like symp- which eye is hypertropic, 2) determine if the hypertro- toms 2 to 4 weeks prior to presentation. pia worsens in left or right gaze, and 3) determine if the Left-sided ptosis and miosis were present on exam- hypertropia worsens in right or left head tilt. In a supe- ination, along with a left adduction deficit. -
Cranial Nerves. Sensory Organs
Kharkiv National Medical University, Department of Human Anatomy CRANIAL NERVES. SENSORY ORGANS. The cranial nerves are: CN I - Olfactory Nerve CN II - Optic Nerve CN III - Oculomotor Nerve CN IV - Trochlear Nerve CN V - Trigeminal Nerve CN VI - Abducens Nerve CN VII - Facial Nerve CN VIII - Vestibulocochlear Nerve CN IX - Glossopharyngeal Nerve CN X - Vagus Nerve CN XI - Accessory Nerve CN XII - Hypoglossal Nerve Classification of the Cranial Nerves It is possible to describe a cranial nerve in terms of its function and embryological origin, initially cranial nerves can be subdivided into being either: Motor (efferent) Sensory (afferent) And from there further categorization can occur. Motor (efferent) Cranial nerves -Somatic motor (general somatic efferent) (III, IV, VI, XII) These cranial nerves are so called because they innervate muscles derived from the occipital somites, such as the extra ocular and extrinsic tongue muscles. Sensory (afferent) cranial nerves -Visceral sensory special visceral afferent- (VII, IX, X) general visceral afferent- (IX, X) The name is related to the fact that it detects sensation from visceral organs. They are divided into special visceral, referring to the rostral portion of the nucleus which contributes to the special sensation of taste. Whilst the general visceral portion is named as such due to this caudal portion receiving general sensory impulses such as cardiac, respiratory . - General somatic sensory (general somatic afferent) (V, VII, IX, X) These nuclei detect general sensation, such as touch, pain, vibration from the face, sinuses and meninges - Special somatic sensory (special somatic) (VIII) This carries information from the special sensation of hearing and balance. -
Peripheral Nervous System Peripheral Nervous System Comprises: A) Cranial Nerves: 12 in Number, Arise Mainly from Brain Stem
Peripheral nervous system Peripheral nervous system comprises: A) Cranial nerves: 12 in number, arise mainly from brain stem. B) Spinal nerves: arise from spinal cord, varies in number according to species. C) Autonomic nervous system : 1-Sympathetic (thoracolumbar) division. 2-Parasympathetic (craniosacral) division. Cranial nerves They are 12 pairs General features: – They are known by roman numbers from (rostral to caudal) . – Some nerves take their names according to: * Function as olfactory and abducent * Distribution as facial and hypoglossal * Shape as trigeminal. - All cranial nerves have superficial origins on ventral aspect of brain except trochlear nerve originates from dorsal aspect of brain. -All cranial nerves except first one originate from brain stem. - Each nerve emerges from cranial cavity through a foramen. - All cranial nerves except vagus distributed generally in head region. - 3,7,9,10 cranial nerves carry parasympathetic fibers. - Classification of cranial nerves: - They are classified according to the function into: 1-Sensory nerves: 1,2,8. 2-Motor nerves: 3,4,6,11,12. 3-Mixed nerves: 5,7,9,10. I- Olfactory nerves Type: • Sensory for smell. • Represented by bundles of nerve fibers, not form trunk. Origin: • Central processes of olfactory cells of olfactory region of nasal cavity. Course: • They pass though cribriform plate to join olfactory bulb. Vomeronasal nerve: • It arises from vomeronasal organ ,passes through medial border of cribriform plate to terminate in olfactory bulb. II- Optic nerve Type: • Sensory for vision. Origin: • Central processes of ganglion cells of retina. Course: • Fibers converge toward optic papilla forming optic nerve, emerges from eyeball. • Then passes through optic foramen and decussates with its fellow to form optic chiasma. -

Anatomical Note the Superficial Origin of the Trochlear Nerve with Special
J. Anat. (1990), 170, pp. 199-201 199 With 4 figures Printed in Great Britain Anatomical Note The superficial origin of the trochlear nerve with special reference to its vascular relations K. K. BISARIA*, I. C. PREMSAGARt, P. K. LAKHTAKIAt, R. C. SAXENA* AND S. D. BISARIA§ * Department of Anatomy, t Department of Neurosurgery, $ Department of Orthopaedic Surgery, K. G. Medical College, Lucknow, U.P. and § Department Of Ophthalmology, Vivekananda Polyclinic, Lucknow, U.P. India (Accepted 14 November 1989) INTRODUCTION A full description of the roots of the trochlear nerve is not commonly found in the literature. Gardner, Gray & O'Rahilly (1960), Hamilton (1976), Romanes (1964), Snell (1981), Hollinshead & Rosse (1985) and Williams, Warwick, Dyson & Bannister (1989) do not mention the possibility of two roots of origin of this nerve. Crosby, Humphrey & Lauer (1962) and Truex & Carpenter (1969) have mentioned that the nerve may emerge as a single root while Paturet (1964) and Nathan & Goldhammer (1973) have mentioned the possibility that more than one root may be present. The relations of the trochlear nerve to the adjoining blood vessels have not been described. MATERIALS AND METHODS For the present work 162 trochlear nerves of 90 formalin-fixed brains were studied (in 18 brains only one of the two nerves could be studied as the other was torn during the removal of the brain from the cranial cavity). The origin of the nerve and its relationships with neighbouring blood vessels was noted. RESULTS In all the 90 brains, the trochlear nerves arose in the usual situation. In 111 nerves out of 162, the nerve had a single root; in 51, double rootlets were present, the rootlets being up to 4 mm apart (Fig. -

Acquired Palsy of the Oculomotor, Trochlear and Abducens Nerves
ACQUIRED PALSY OF THE OCULOMOTOR, TROCHLEAR AND ABDUCENS NERVES l 2 P. A. C. TIFFIN\ C. J. MacEWEN\ E. A. CRAIG and G. CLAYTON Dundee SUMMARY commonly than trochlear nerve palsy. In addition, There have been few studies primarily concerned with although the major cause of ocular palsy was the relative frequencies, aetiologies and prognoses of consistently classified as undetermined (25%), a ocular motor palsies. Those published have emanated relatively high proportion of cases were recorded as largely from neurological tertiary referral centres rather secondary to sinister pathology: neoplasia (18%) and than primary ophthalmology departments. We have aneurysm (7%). performed a retrospective study of all patients with There have been several studies relating to series acquired III, IV or VI cranial nerve palsy who were of patients seen in the more general setting of both s 9 seen in the orthoptic department at Ninewells Hospital, orthoptic and ophthalmic clinics. - However, these Dundee, over the 9 year period from 1984 to 1992. A have concentrated on groups of patients presenting total of 165 cases were identified. VI nerve palsies with the somewhat broader diagnosis of diplopia accounted for the majority of patients (57%), with IV rather than only those with acquired nerve palsies nerve palsies (21%) occurring more frequently than III per se. Acquired ocular motor nerve palsy accounted nerve palsies (17%) and multiple palsies (5%). Thirty for 40-60% of patients presenting with binocular five per cent of cases were of unknown aetiology and diplopia. Although abducens nerve palsy occurred 6 8 9 32% of vascular aetiology. The incidence of sinister most frequently in most of these reports, , , oculo s pathology - neoplasia (2%) and aneurysm (1%) - was motor nerve palsy was found most often in one and surprisingly low. -
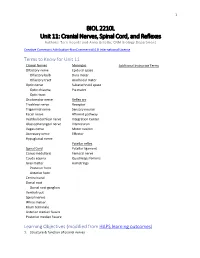
Unit 11 Cranial Nerves, Spinal Cord, and Reflexes
1 BIOL 2210L Unit 11: Cranial Nerves, Spinal Cord, and Reflexes Authors: Terri Koontz and Anna Gilletly, CNM Biology Department Creative Commons Attribution-NonCommercial 4.0 International License Terms to Know for Unit 11 Cranial Nerves Meninges Additional Instructor Terms Olfactory nerve Epidural space Olfactory bulb Dura mater Olfactory tract Arachnoid mater Optic nerve Subarachnoid space Optic chiasma Pia mater Optic tract Oculomotor nerve Reflex arc Trochlear nerve Receptor Trigeminal nerve Sensory neuron Facial nerve Afferent pathway Vestibulocochlear nerve Integration Center Glossopharyngeal nerve Interneuron Vagus nerve Motor neuron Accessory nerve Effector Hypoglossal nerve Patellar reflex Spinal Cord Patellar ligament Conus medullaris Femoral nerve Cauda equina Quadriceps femoris Gray matter Hamstrings Posterior horn Anterior horn Central canal Dorsal root Dorsal root ganglion Ventral root Spinal nerves White matter Filum terminale Anterior median fissure Posterior median fissure Learning Objectives (modified from HAPS learning outcomes) 1. Structure & function of cranial nerves 2 a. List and identify the cranial nerves by name and number. b. Describe the specific functions of each of the cranial nerves and classify each as sensory, motor or mixed. c. Identify the foramina that the cranial nerves pass through within the skull. 2. Anatomy of the spinal cord a. Describe the gross anatomy of the spinal cord. b. Identify the anatomical features seen in a cross sectional view of the spinal cord c. Identify the dorsal root ganglia, dorsal and ventral roots, and spinal nerves. 3. Reflexes & their roles in nervous system function a. Define the term reflex. b. Describe reflex responses in terms of the major structural and functional components of a reflex arc. -

Human Anatomy Lab - Examination of the Cranial Nerves
Utah State University DigitalCommons@USU Undergraduate Honors Capstone Projects Honors Program 5-1993 Human Anatomy Lab - Examination of the Cranial Nerves Jeanne Falk Utah State University Follow this and additional works at: https://digitalcommons.usu.edu/honors Part of the Nervous System Commons Recommended Citation Falk, Jeanne, "Human Anatomy Lab - Examination of the Cranial Nerves" (1993). Undergraduate Honors Capstone Projects. 296. https://digitalcommons.usu.edu/honors/296 This Thesis is brought to you for free and open access by the Honors Program at DigitalCommons@USU. It has been accepted for inclusion in Undergraduate Honors Capstone Projects by an authorized administrator of DigitalCommons@USU. For more information, please contact [email protected]. JEANNE FALK SENIOR PROJECT HUMANANATOMY LAB - EXAMINATIONOF THE CRANIALNERVES The peripheral nervous system consists of twelve pairs of cranial nerves, 31 pairs of spinal nerves, and the nerves of the autonomic nervous system. The cranial nerves are the nerves that leave the brain directly. These nerves control various actions and sensations such as sight, smell, .chewing, and swallowing, and will be the focus of this week's lab. Of the twelve pairs of cranial nerves, two pairs arise from the forebrain, ten pairs arise from the midbrain and brain stem, and all but the Vagus nerve innervates the structures in the head and neck. Each cranial nerve pair is designated with a Roman nwneral in reference to the order in which the nerves are positioned from the front to the back of the brain. The names given to the nerves indicate the structures innervated or the principle functions of the nerves.