TROVAN® Tablets(Trovafloxacin Mesylate)
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Fluoroquinolones in the Management of Acute Lower Respiratory Infection
Thorax 2000;55:83–85 83 Occasional review Thorax: first published as 10.1136/thorax.55.1.83 on 1 January 2000. Downloaded from The next generation: fluoroquinolones in the management of acute lower respiratory infection in adults Peter J Moss, Roger G Finch Lower respiratory tract infections (LRTI) are ing for up to 40% of isolates in Spain19 and 33% the leading infectious cause of death in most in the United States.20 In England and Wales developed countries; community acquired the prevalence is lower; in the first quarter of pneumonia (CAP) and acute exacerbations of 1999 6.5% of blood/cerebrospinal fluid isolates chronic bronchitis (AECB) are responsible for were reported to the Public Health Laboratory the bulk of the adult morbidity. Until recently Service as showing intermediate sensitivity or quinolone antibiotics were not recommended resistance (D Livermore, personal communi- for the routine treatment of these infections.1–3 cation). Pneumococcal resistance to penicillin Neither ciprofloxacin nor ofloxacin have ad- is not specifically linked to quinolone resist- equate activity against Streptococcus pneumoniae ance and, in general, penicillin resistant in vitro, and life threatening invasive pneumo- pneumococci are sensitive to the newer coccal disease has been reported in patients fluoroquinolones.11 21 treated for respiratory tract infections with Resistance to ciprofloxacin develops rela- these drugs.4–6 The development of new fluoro- tively easily in both S pneumoniae and H influ- quinolone agents with increased activity enzae, requiring only a single mutation in the against Gram positive organisms, combined parC gene.22 23 Other quinolones such as with concerns about increasing microbial sparfloxacin and clinafloxacin require two resistance to â-lactam agents, has prompted a mutations in the parC and gyrA genes.11 23 re-evaluation of the use of quinolones in LRTI. -
FLUOROQUINOLONES: from Structure to Activity and Toxicity
FLUOROQUINOLONES: from structure to activity and toxicity F. Van Bambeke, Pharm. D. & P. M. Tulkens, MD, PhD Unité de Pharmacologie Cellulaire et Moléculaire Université Catholique de Louvain, Brussels, Belgium SBIMC / BVIKM www.sbimc.org - www.bvikm.org www.md.ucl.ac.be/facm www.isap.org soon... Mechanism of action of fluoroquinolones: the basics... PORIN DNA Topo DNA gyrase isomerase Gram (-) Gram (+) 2 key enzymes in DNA replication: DNA gyrase topoisomerase IV bacterial DNA is supercoiled Ternary complex DNA - enzyme - fluoroquinolone DNA GYRASE catalytic subunits COVALENTLY CLOSED CIRCULAR DNA FLUOROQUINOLONES: DNA GYRASE ATP binding subunits 4 stacked molecules (Shen, in Quinolone Antimicrobial Agents, 1993) Resistance to fluoroquinolones: the basics decreased efflux pump permeability DNA mutation of DNA gyrase Topo isomerase the enzymes Gram (-) Gram (+) Fluoroquinolones are the first entirely man-made antibiotics: do we understand our molecule ? R5 O R COOH 6 R7 X8 N R1 Don’t panic, we will travel together…. Chemistry and Activity This is where all begins... The pharmacophore common to all fluoroquinolones BINDING TO DNA R5 O O R C 6 - BINDING TO O BINDING TO THE ENZYME THE ENZYME R7 X8 N R1 AUTO-ASSEMBLING DOMAIN (for stacking) From chloroquine to nalidixic acid... nalidixic acid N CH3 O O HN CH 3 C - O chloroquine CH N N Cl N 3 C2H5 1939 O O C O- 1962 Cl N 1958 C2H5 7-chloroquinoline (synthesis intermediate found to display antibacterial activity) Nalidixic acid * a • typical chemical features of O O fluoroquinolones (a, b, c) BUT a naphthridone C - O- b (N at position 8: ) H C N N 3 • limited usefulness as drug C H 2 5 • narrow antibacterial spectrum c (Enterobacteriaceae only) • short half-life (1.5h) • high protein binding (90%) * Belg. -

WHO Report on Surveillance of Antibiotic Consumption: 2016-2018 Early Implementation ISBN 978-92-4-151488-0 © World Health Organization 2018 Some Rights Reserved
WHO Report on Surveillance of Antibiotic Consumption 2016-2018 Early implementation WHO Report on Surveillance of Antibiotic Consumption 2016 - 2018 Early implementation WHO report on surveillance of antibiotic consumption: 2016-2018 early implementation ISBN 978-92-4-151488-0 © World Health Organization 2018 Some rights reserved. This work is available under the Creative Commons Attribution- NonCommercial-ShareAlike 3.0 IGO licence (CC BY-NC-SA 3.0 IGO; https://creativecommons. org/licenses/by-nc-sa/3.0/igo). Under the terms of this licence, you may copy, redistribute and adapt the work for non- commercial purposes, provided the work is appropriately cited, as indicated below. In any use of this work, there should be no suggestion that WHO endorses any specific organization, products or services. The use of the WHO logo is not permitted. If you adapt the work, then you must license your work under the same or equivalent Creative Commons licence. If you create a translation of this work, you should add the following disclaimer along with the suggested citation: “This translation was not created by the World Health Organization (WHO). WHO is not responsible for the content or accuracy of this translation. The original English edition shall be the binding and authentic edition”. Any mediation relating to disputes arising under the licence shall be conducted in accordance with the mediation rules of the World Intellectual Property Organization. Suggested citation. WHO report on surveillance of antibiotic consumption: 2016-2018 early implementation. Geneva: World Health Organization; 2018. Licence: CC BY-NC-SA 3.0 IGO. Cataloguing-in-Publication (CIP) data. -

Current Use for Old Antibacterial Agents: Polymyxins, Rifamycins, and Aminoglycosides
Current Use for Old Antibacterial Agents: Polymyxins, Rifamycins, and Aminoglycosides a, b,c Luke F. Chen, MBBS (Hons), MPH, CIC, FRACP *, Donald Kaye, MD KEYWORDS Rifaximin Pharmacokinetics Pharmacodynamics Toxicity Polymyxins Aminoglycoside Rifampin The polymyxins, rifamycins, and the aminoglycosides may be considered special use antibacterial agents. They are all old agents and are rarely considered the drugs of choice for common bacterial infections. The polymyxins are increasingly important because of the continued emergence of multidrug resistant (MDR) gram-negative organisms, such as strains of Pseudomonas aeruginosa or carbapenemase-producing Enterobacteriaceae that are susceptible to few remaining drugs. Rifampin is only considered in the context of nonmycobacterial infections where its role is limited and sometimes controversial. Rifaximin is a new enteric rifamycin that is increasingly used for gastrointestinal infections such as trav- eler’s diarrhea and Clostridium difficile infections (CDIs). This article will also review the current role of aminoglycosides in nonmycobacterial systemic infections, with an emphasis on the use of single daily administration. POLYMYXINS The polymyxins were discovered in 1947. Although there are five known polymyxin molecules, sequentially named polymyxin A through polymyxin E, only two polymyxins are available for therapeutic use: polymyxin B and polymyxin E (colistin) (Table 1). Both polymyxin B and polymyxin E are large cyclic cationic polypeptide detergents A version of this article appeared in the 23:4 issue of the Infectious Disease Clinics of North America. a Division of Infectious Diseases and International Health, Department of Medicine, Duke University Medical Center, Box 102359, Hanes House, Durham, NC 27710, USA b Department of Medicine, Drexel University College of Medicine, Philadelphia, PA 19102, USA c 1535 Sweet Briar Road, Gladwyne, PA 19035, USA * Corresponding author. -

Surveillance of Antimicrobial Consumption in Europe 2013-2014 SURVEILLANCE REPORT
SURVEILLANCE REPORT SURVEILLANCE REPORT Surveillance of antimicrobial consumption in Europe in Europe consumption of antimicrobial Surveillance Surveillance of antimicrobial consumption in Europe 2013-2014 2012 www.ecdc.europa.eu ECDC SURVEILLANCE REPORT Surveillance of antimicrobial consumption in Europe 2013–2014 This report of the European Centre for Disease Prevention and Control (ECDC) was coordinated by Klaus Weist. Contributing authors Klaus Weist, Arno Muller, Ana Hoxha, Vera Vlahović-Palčevski, Christelle Elias, Dominique Monnet and Ole Heuer. Data analysis: Klaus Weist, Arno Muller and Ana Hoxha. Acknowledgements The authors would like to thank the ESAC-Net Disease Network Coordination Committee members (Marcel Bruch, Philippe Cavalié, Herman Goossens, Jenny Hellman, Susan Hopkins, Stephanie Natsch, Anna Olczak-Pienkowska, Ajay Oza, Arjana Tambić Andrasevic, Peter Zarb) and observers (Jane Robertson, Arno Muller, Mike Sharland, Theo Verheij) for providing valuable comments and scientific advice during the production of the report. All ESAC-Net participants and National Coordinators are acknowledged for providing data and valuable comments on this report. The authors also acknowledge Gaetan Guyodo, Catalin Albu and Anna Renau-Rosell for managing the data and providing technical support to the participating countries. Suggested citation: European Centre for Disease Prevention and Control. Surveillance of antimicrobial consumption in Europe, 2013‒2014. Stockholm: ECDC; 2018. Stockholm, May 2018 ISBN 978-92-9498-187-5 ISSN 2315-0955 -
Exploiting the Potential of Transforming Anti-Bacterial Xacins
SCIOL BIOTECHNOLOGY ISSN: 2631-4061 RESEARCH ArtiCLE Exploiting the Potential of Transforming Anti- Bacterial Xacins into Anti-Tumor Hit Compounds Zhi-Gang Sun1,2*, Qing Yuan1 and Yu-Shun Yang1* 1School of Life Sciences, Nanjing University, Nanjing 210023, China 2Central Laboratory, Linyi Central Hospital, Linyi 276400, Shandong, China *Correspondence to: Abstract Zhi-Gang Sun and Yu-Shun Yang Objectives: Exploit the possibility of turning anti-bacterial drugs, xacins, into anti-tumor hit compounds. Citation: Zhi-Gang S, Yuan Q, Yu-Shun Y (2018) Exploiting Materials and methods: Data of xacins were collected. The energy minimization and mo- the Potential of Transform- lecular overlay were conducted to evaluate the consistency in conformation. Docking sim- ulation into topoisomerases was performed to develop possible inhibitors from the usual ing Anti-Bacterial Xacins into anti-bacterial drugs. Anti-Tumor Hit Compounds. SCIOL Biotechnol 2018;1:83- Results: The energy minimization and molecular overlay showed good consistency. The 88 binding situations were available for developing prodrugs for Topo II and Topo III from the xacins. Alatrofloxacin was the top hit into both Topo II and Topo III. Accepted: December 12, 2018 Published: December 14, 2018 Conclusions: The traditional anti-bacterial xacins were potential hit compounds for devel- oping Human Topo II and Topo III inhibitors. Introduction Along with the development of the modern society, the risk of suffering from cancer has become a worldwide and urgent problem with increasing occurrence [1]. Though researchers have achieved tremendous progress on novel agents and therapeutic methods, more and more drugs and techniques in medicinal chemistry are still in emergency 2[ ]. -
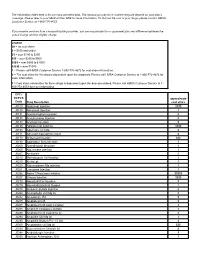
CPT / HCPCS Code Drug Description Approximate Cost Share
The information listed here is for our most prevalent plan. The amount you pay for a covered drug will depend on your plan’s coverage. Please refer to your Medical Plan GTB for more information. To find out the cost of your drugs, please contact HMSA Customer Service at 1-800-776-4672. If you receive services from a nonparticipating provider, you are responsible for a copayment plus any difference between the actual charge and the eligible charge. Legend $0 = no cost share $ = $100 and under $$ = over $100 to $250 $$$ = over $250 to $500 $$$$ = over $500 to $1000 $$$$$ = over $1000 1 = Please call HMSA Customer Service 1-800-776-4672 for cost share information. 2 = The cost share for this drug is dependent upon the diagnosis. Please call HMSA Customer Service at 1-800-772-4672 for more information. 3 = Cost share information for these drugs is dependent upon the dose prescribed. Please call HMSA Customer Service at 1- 800-772-4672 for more information. CPT / HCPCS approximate Code Drug Description cost share J0129 Abatacept Injection $$$$ J0130 Abciximab Injection 3 J0131 Acetaminophen Injection $ J0132 Acetylcysteine Injection $ J0133 Acyclovir Injection $ J0135 Adalimumab Injection $$$$ J0153 Adenosine Inj 1Mg $ J0171 Adrenalin Epinephrine Inject $ J0178 Aflibercept Injection $$$ J0180 Agalsidase Beta Injection 3 J0200 Alatrofloxacin Mesylate 3 J0205 Alglucerase Injection 3 J0207 Amifostine 3 J0210 Methyldopate Hcl Injection 3 J0215 Alefacept 3 J0220 Alglucosidase Alfa Injection 3 J0221 Lumizyme Injection 3 J0256 Alpha 1 Proteinase Inhibitor -
CLOSED PODS Information Sheets
SUMMIT COUNTY PUBLIC HEALTH CLOSED PODS Information Sheets Generic Names of Doxycycline, Ciprofloxacin, and AmoxicillinDOXYCYCLINE / TETRACYCLINE Achromycin Minocin Adoxa Minocycline Arestin Monodox Atridox Myrac Declomycin Oracea Demeclocycline Periodox Doryx Solodyn Doxy Sumycin Doxycycline Tetracycline Dynacin Tigecycline Tygacil Vibramycin Vibra-tabs CIPROFLOXACIN / QUINOLONE / FLUOROQUINOLONE Avelox Maxaquin Cinobac Moxifloxacin HCL Cinoxacin Nalidixic Acid Cipro NegGram Ciprofloxacin Norfloxacin Factive Noroxin Floxin Ofloxacin Gemifloxacin Mesylate Proquin XR Levaquin Sparfloxacin Levofloxacin Trovafloxacin/Alatrofloxacin Mesylate Lomefloxacin HCL Trovan Zagam AMOXICILLIN / PENICILLIN Amoclan Cefotan Keflex Tazicef Amoxicillin Cefotaxime Maxipime Tazidime Amoxicillin/Clavulanate Cefotetan Mefoxin Tazocin Amoxil Cefoxitin Moxatag Ticar Ampicillin Cefpodoxime Nafcil Ticarcillin Ampicillin/Sulbactam Cefprozil Nafcillin Ticarcillin/Clavulanate Augmentin Ceftazidime Omnicef Timentin Bactocill Ceftibuten Oxacillin Trimox Bicillin CR Ceftin Pen VK Unasyn Bicillin LA Ceftizoxime Pencillin G Vantin Carbenicillin Indanyl Sodium Ceftriaxone Penicillin V Veetids Ceclor Cefuroxime Permapen Wycillin Cedax Cefzil PfizerPen Zinacef Cefaclor Cephalexin Piperacillin Zosyn Cefadroxil Cephazolin Piperacillin/Tazobactam Cefazolin Ceptaz Pipracil Cefdinir Claforan Principen Cefditoren Pivoxil Diclox Raniclor Cefepime HCL Dicloxacillin Rocephin Cefixime DisperMox Spectracef Cefizox Duricef Suprax Cefobid Fortaz Cefoperazone Geocillin Sample Information -

Pharmacokinetic Drug Interactions of Antimicrobial Drugs: a Systematic Review on Oxazolidinones, Rifamycines, Macrolides, Fluoroquinolones, and Beta-Lactams
Pharmaceutics 2011, 3, 865-913; doi:10.3390/pharmaceutics3040865 OPEN ACCESS Pharmaceutics ISSN 1999-4923 www.mdpi.com/journal/pharmaceutics Review Pharmacokinetic Drug Interactions of Antimicrobial Drugs: A Systematic Review on Oxazolidinones, Rifamycines, Macrolides, Fluoroquinolones, and Beta-Lactams Mathieu S. Bolhuis *, Prashant N. Panday, Arianna D. Pranger, Jos G. W. Kosterink and Jan-Willem C. Alffenaar Department of Hospital and Clinical Pharmacy, University Medical Center Groningen, University of Groningen, PO Box 30.001, 9700 RB Groningen, The Netherlands; E-Mails: [email protected] (P.N.P.); [email protected] (A.D.P.); [email protected] (J.G.W.K.); [email protected] (J.-W.C.A.) * Author to whom correspondence should be addressed; E-Mail: [email protected]; Tel.: +31-50-361-4071; Fax: +31-50-361-4078 Received: 15 October 2011; in revised form: 26 October 2011 / Accepted: 9 November 2011 / Published: 18 November 2011 Abstract: Like any other drug, antimicrobial drugs are prone to pharmacokinetic drug interactions. These drug interactions are a major concern in clinical practice as they may have an effect on efficacy and toxicity. This article provides an overview of all published pharmacokinetic studies on drug interactions of the commonly prescribed antimicrobial drugs oxazolidinones, rifamycines, macrolides, fluoroquinolones, and beta-lactams, focusing on systematic research. We describe drug-food and drug-drug interaction studies in humans, affecting antimicrobial drugs as well as concomitantly administered drugs. Since knowledge about mechanisms is of paramount importance for adequate management of drug interactions, the most plausible underlying mechanism of the drug interaction is provided when available. -

Standing Order for Tularemia Prophylaxis
OREGON HEALTH AUTHORITY PUBLIC HEALTH DIVISION ACUTE AND COMMUNICABLE DISEASE PREVENTION SECTION Tularemia Prophylaxis I. OREGON MODEL PROTOCOL 1. Follow the nursing assessment of individuals presenting for prophylactic treatment to a known or potentially harmful biological agent. 2. Provide patient information about tularemia and the preventive antibiotics prior to administration, answering any questions 3. Dispense antibiotic prophylaxis in accordance with prophylactic treatment guidelines (Table 1) and within the restrictions of the guidelines of the Strategic National Stockpile program. ________________________________________________________ Signature, Health Officer Date II. Persons for whom prophylaxis may be dispensed The World Health Organization recommends post-exposure prophylaxis in the following settings: 1. Exposure of laboratory personnel to Francisella tularensis in the absence of proper infection control measures; 2. Exposure to an aerosolized release of Francisella tularensis. Tularemia Page 2 of 15 Table 1 Recommendations for Treatment of Patients with Tularemia in a Mass Casualty Setting and for Post-exposure Prophylaxis a Preferred Choices Adults Doxycycline, 100 mg orally twice daily b Ciprofloxacin, 500 mg orally twice daily Preferred Choices Doxycycline; if ≥45 kg, give 100 mg orally twice daily; Children Doxycycline, if <45 kg, give 2.2 mg/kg orally twice daily; Ciprofloxacin, 10–15 mg/kg orally twice daily c Preferred Choices Pregnant women Ciprofloxacin, 500 mg orally twice daily b Doxycycline, 100 mg orally twice daily a One antibiotic, appropriate for patient age, should be chosen from among alternatives. The duration of all recommended therapies in Table 1 is 14 days. b Not a US Food and Drug Administration–approved use. c Ciprofloxacin dosage should not exceed 1g/d in children. -

Inhibitory Effects of Fluoroquinolone Antibiotics on Babesia Divergens and Babesia Microti, Blood Parasites of Veterinary and Zoonotic Importance
Journal name: Infection and Drug Resistance Article Designation: Original Research Year: 2018 Volume: 11 Infection and Drug Resistance Dovepress Running head verso: Rizk et al Running head recto: Effects of fluoroquinolones on Babesia parasites open access to scientific and medical research DOI: http://dx.doi.org/10.2147/IDR.S159519 Open Access Full Text Article ORIGINAL RESEARCH Inhibitory effects of fluoroquinolone antibiotics on Babesia divergens and Babesia microti, blood parasites of veterinary and zoonotic importance Mohamed Abdo Rizk1,2 Aim: This study aimed to evaluate the inhibitory effects of fluoroquinolone antibiotics, includ- Mahmoud AbouLaila3 ing enrofloxacin, enoxacin, trovafloxacin, norfloxacin, and ofloxacin, on the in vitro and in vivo Shimaa Abd El-Salam growth of Babesia divergens and Babesia microti parasites, respectively. El-Sayed1,4 Materials and methods: The in vitro and in vivo inhibitory effects of fluoroquinolone Azirwan Guswanto1,5 antibiotics against B. divergens and B. microti, respectively were evaluated using fluorescence- based assay. Additionally, combination therapies of highly effective fluoroquinolone antibiotics Naoaki Yokoyama1 (enrofloxacin, enoxacin, and trovafloxacin) with diminazene aceturate, luteolin, or pyronaridine Ikuo Igarashi1 tetraphosphate were tested on the in vitro cultures of B. divergens. 1 National Research Center for Results: Enrofloxacin, trovafloxacin, and enoxacin were the most effective fluoroquinolones Protozoan Diseases, Obihiro University of Agriculture and against the in vitro growth of B. divergens, followed by norfloxacin and ofloxacin. Further- Veterinary Medicine, Inada-Cho, more, a combination of enoxacin or trovafloxacin with either diminazene aceturate, luteolin, Obihiro, Hokkaido, Japan; or pyronaridine tetraphosphate significantly enhanced the inhibitory effect on the growth ofB. 2Department of Internal Medicine and Infectious Diseases, Faculty of divergens in in vitro cultures. -

Appendix C Medication Tables
Appendix C Medication Tables Note: The medication tables are not meant to be inclusive lists of all available therapeutic agents. Approved medication tables will be updated regularly. Discrepancies must be reported. See Resource Section of this manual for additional contact information. Release Notes: Aspirin Table Version 1.0 Table 1.1 Aspirin and Aspirin-Containing Medications Acetylsalicylic Acid Acuprin 81 Alka-Seltzer Alka-Seltzer Morning Relief Anacin Arthritis Foundation Aspirin Arthritis Pain Ascriptin Arthritis Pain Formula ASA ASA Baby ASA Baby Chewable ASA Baby Coated ASA Bayer ASA Bayer Children's ASA Buffered ASA Children's ASA EC ASA Enteric Coated ASA/Maalox Ascriptin Aspergum Aspir-10 Aspir-Low Aspir-Lox Aspir-Mox Aspir-Trin Aspirbuf Aspircaf Aspirin Aspirin Baby Aspirin Bayer Aspirin Bayer Children's Aspirin Buffered Aspirin Child Aspirin Child Chewable Aspirin Children's Aspirin EC Aspirin Enteric Coated Specifications Manual for National Appendix C-1 Hospital Quality Measures Table 1.1 Aspirin and Aspirin-Containing Medications (continued) Aspirin Litecoat Aspirin Lo-Dose Aspirin Low Strength Aspirin Tri-Buffered Aspirin, Extended Release Aspirin/butalbital/caffeine Aspirin/caffeine Aspirin/pravachol Aspirin/pravastatin Aspirtab Bayer Aspirin Bayer Aspirin PM Extra Strength Bayer Children’s Bayer EC Bayer Enteric Coated Bayer Low Strength Bayer Plus Buffered ASA Buffered Aspirin Buffered Baby ASA Bufferin Bufferin Arthritis Strength Bufferin Extra Strength Buffex Cama Arthritis Reliever Child’s Aspirin Coated Aspirin