EAU Guidelines on Urolithiasis 2019
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Urinary Stone Disease – Assessment and Management
Urology Urinary stone disease Finlay Macneil Simon Bariol Assessment and management Data from the Australian Institute of Health and Welfare Background showed an annual incidence of 131 cases of upper urinary Urinary stones affect one in 10 Australians. The majority tract stone disease per 100 000 population in 2006–2007.1 of stones pass spontaneously, but some conditions, particularly ongoing pain, renal impairment and infection, An upper urinary tract stone is the usual cause of what is mandate intervention. commonly called ‘renal colic’, although it is more technically correct to call the condition ‘ureteric colic’. Objective This article explores the role of the general practitioner in Importantly, the site of the pain is notoriously inaccurate in predicting the assessment and management of urinary stones. the site of the stone, except in the setting of new onset lower urinary Discussion tract symptoms, which may indicate distal migration of a stone. The The assessment of acute stone disease should determine majority of stones only become clinically apparent when they migrate the location, number and size of the stone(s), which to the ureter, although many are also found on imaging performed for influence its likelihood of spontaneous passage. Conservative other reasons.2,3 The best treatment of a ureteric stone is frequently management, with the addition of alpha blockers to facilitate conservative (nonoperative), because all interventions (even the more passage of lower ureteric stones, should be attempted in modern ones) carry risks. However, intervention may be indicated in cases of uncomplicated renal colic. Septic patients require urgent drainage and antibiotics. Other indications for referral certain situations. -

Urology Services in the ASC
Urology Services in the ASC Brad D. Lerner, MD, FACS, CASC Medical Director Summit ASC President of Chesapeake Urology Associates Chief of Urology Union Memorial Hospital Urologic Consultant NFL Baltimore Ravens Learning Objectives: Describe the numerous basic and advanced urology cases/lines of service that can be provided in an ASC setting Discuss various opportunities regarding clinical, operational and financial aspects of urology lines of service in an ASC setting Why Offer Urology Services in Your ASC? Majority of urologic surgical services are already outpatient Many urologic procedures are high volume, short duration and low cost Increasing emphasis on movement of site of service for surgical cases from hospitals and insurance carriers to ASCs There are still some case types where patients are traditionally admitted or placed in extended recovery status that can be converted to strictly outpatient status and would be suitable for an ASC Potential core of fee-for-service case types (microsurgery, aesthetics, prosthetics, etc.) Increasing Population of Those Aged 65 and Over As of 2018, it was estimated that there were 51 million persons aged 65 and over (15.63% of total population) By 2030, it is expected that there will be 72.1 million persons aged 65 and over National ASC Statistics - 2017 Urology cases represented 6% of total case mix for ASCs Urology cases were 4th in median net revenue per case (approximately $2,400) – behind Orthopedics, ENT and Podiatry Urology comprised 3% of single specialty ASCs (5th behind -

Intravesical Ureterocele Into Childhoods: Report of Two Cases and Review of Literature
Archives of Urology ISSN: 2638-5228 Volume 2, Issue 2, 2019, PP: 1-4 Intravesical Ureterocele into Childhoods: Report of Two Cases and Review of Literature Kouka Scn1*, Diallo Y1, Ali Mahamat M2, Jalloh M3, Yonga D4, Diop C1, Ndiaye Md1, Ly R1, Sylla C1 1 2Departement of Urology, University of N’Djamena, Tchad. Departement3Departement of Urology, of Urology, Faculty University of Health Cheikh Sciences, Anta University Diop of Dakar, of Thies, Senegal. Senegal. 4Service of surgery, County Hospital in Mbour, Senegal. [email protected] *Corresponding Author: Kouka SCN, Department of Urology, Faculty of Health Sciences, University of Thies, Senegal. Abstract Congenital ureterocele may be either ectopic or intravesical. It is a cystic dilatation of the terminal segment of the ureter that can cause urinary tract obstruction in children. The authors report two cases of intravesical ureterocele into two children: a 7 years-old girl and 8 years-old boy. Children were referred for abdominal pain. Ultrasound of the urinary tract and CT-scan showed intravesical ureterocele, hydronephrosis and dilatation of ureter. The girl presented a ureterocele affecting the upper pole in a duplex kidney and in the boy it occurred in a simplex kidney. They underwent a surgical treatment consisting of an ureterocelectomy with ureteral reimplantation according to Cohen procedure. The epidemiology, classification, diagnosis and management aspects are discussed through a review of literature. Keywords: intravesical ureterocele, urinary tract obstruction, surgery. Introduction left distal ureter associated with left hydronephrosis in a duplex kidney. The contralateral kidney was Ureterocele is an abnormal dilatation of the terminal segment of the intravesical ureter [1]. -

Acute Onset Flank Pain-Suspicion of Stone Disease (Urolithiasis)
Date of origin: 1995 Last review date: 2015 American College of Radiology ® ACR Appropriateness Criteria Clinical Condition: Acute Onset Flank Pain—Suspicion of Stone Disease (Urolithiasis) Variant 1: Suspicion of stone disease. Radiologic Procedure Rating Comments RRL* CT abdomen and pelvis without IV 8 Reduced-dose techniques are preferred. contrast ☢☢☢ This procedure is indicated if CT without contrast does not explain pain or reveals CT abdomen and pelvis without and with 6 an abnormality that should be further IV contrast ☢☢☢☢ assessed with contrast (eg, stone versus phleboliths). US color Doppler kidneys and bladder 6 O retroperitoneal Radiography intravenous urography 4 ☢☢☢ MRI abdomen and pelvis without IV 4 MR urography. O contrast MRI abdomen and pelvis without and with 4 MR urography. O IV contrast This procedure can be performed with US X-ray abdomen and pelvis (KUB) 3 as an alternative to NCCT. ☢☢ CT abdomen and pelvis with IV contrast 2 ☢☢☢ *Relative Rating Scale: 1,2,3 Usually not appropriate; 4,5,6 May be appropriate; 7,8,9 Usually appropriate Radiation Level Variant 2: Recurrent symptoms of stone disease. Radiologic Procedure Rating Comments RRL* CT abdomen and pelvis without IV 7 Reduced-dose techniques are preferred. contrast ☢☢☢ This procedure is indicated in an emergent setting for acute management to evaluate for hydronephrosis. For planning and US color Doppler kidneys and bladder 7 intervention, US is generally not adequate O retroperitoneal and CT is complementary as CT more accurately characterizes stone size and location. This procedure is indicated if CT without contrast does not explain pain or reveals CT abdomen and pelvis without and with 6 an abnormality that should be further IV contrast ☢☢☢☢ assessed with contrast (eg, stone versus phleboliths). -
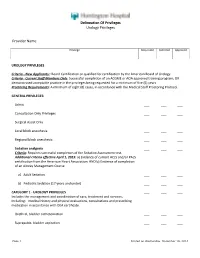
Delineation of Privileges Urology Privileges Provider Name
Delineation Of Privileges Urology Privileges Provider Name: Privilege Requested Deferred Approved UROLOGY PRIVILEGES Criteria - New Applicants:: Board Certification or qualified for certification by the American Board of Urology. Criteria - Current Staff Members Only: Successful completion of an ACGME or AOA approved training program; OR demonstrated acceptable practice in the privileges being requested for a minimum of five (5) years. Proctoring Requirements: A minimum of eight (8) cases, in accordance with the Medical Staff Proctoring Protocol. GENERAL PRIVILEGES: Admit ___ ___ ___ Consultation Only Privileges ___ ___ ___ Surgical Assist Only ___ ___ ___ Local block anesthesia ___ ___ ___ Regional block anesthesia ___ ___ ___ Sedation analgesia ___ ___ ___ Criteria: Requires successful completion of the Sedation Assessment test. Additional criteria effective April 1, 2015: a) Evidence of current ACLS and/or PALS certification from the American Heart Association; AND b) Evidence of completion of an Airway Management Course a) Adult Sedation ___ ___ ___ b) Pediatric Sedation (17 years and under) ___ ___ ___ CATEGORY 1 - UROLOGY PRIVILEGES ___ ___ ___ Includes the management and coordination of care, treatment and services, including: medical history and physical evaluations, consultations and prescribing medication in accordance with DEA certificate. Urethral, bladder catheterization ___ ___ ___ Suprapubic, bladder aspiration ___ ___ ___ Page 1 Printed on Wednesday, December 10, 2014 Delineation Of Privileges Urology Privileges Provider -

Management of Ureteral Stones
Management of Ureteral Stones Ureteral stone disease is among the most painful and prevalent of urologic disorders. As many as 5 percent of Americans will be affected by urinary stones at some point in their lives. Fortunately, most stones pass out of the body without any intervention. If you are not so lucky, the following information should help you and your doctor address the causes, symptoms and possible complications created by your ureteral stone disease. How does the urinary tract work under normal conditions? The urinary tract is similar to a plumbing system, with special pipes that allow water and salts to flow through them. The urinary tract includes two kidneys, two ureters and the urethra. The kidneys act as a filter system for the blood, cleansing it of poisonous materials and retaining valuable glucose, salts and minerals. Urine, the waste product of the filtration, is produced in the kidney and trickles down hours a day through two 10- to 12-inch long tubes called ureters, which connect the kidneys to the bladder. The ureters are about one-fourth inch in diameter and their muscular walls contract to make waves of movement to force the urine into the bladder. The bladder is expandable and stores the urine until it can be conveniently disposed of. It also closes passageways into the ureters so that urine cannot flow back into the kidneys. The tube through which the urine flows out of the body is called the urethra. What is a ureteral stone? A ureteral stone is a kidney stone that has moved down into the ureter. -

Renal Colic, Adult – Emergency V 1.0
Provincial Clinical Knowledge Topic Renal Colic, Adult – Emergency V 1.0 Copyright: © 2018, Alberta Health Services. This work is licensed under the Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License. To view a copy of this license, visit http://creativecommons.org/licenses/by-nc-nd/4.0/. Disclaimer: This material is intended for use by clinicians only and is provided on an "as is", "where is" basis. Although reasonable efforts were made to confirm the accuracy of the information, Alberta Health Services does not make any representation or warranty, express, implied or statutory, as to the accuracy, reliability, completeness, applicability or fitness for a particular purpose of such information. This material is not a substitute for the advice of a qualified health professional. Alberta Health Services expressly disclaims all liability for the use of these materials, and for any claims, actions, demands or suits arising from such use. Revision History Version Date of Revision Description of Revision Revised By 1.0 September 2018 Version 1 of topic completed see Acknowledgments Renal Colic, Adult – Emergency V 1.0 Page 2 of 20 Important Information Before you Begin The recommendations contained in this knowledge topic have been provincially adjudicated and are based on best practice and available evidence. Clinicians applying these recommendations should, in consultation with the patient, use independent medical judgment in the context of individual clinical circumstances to direct care. This knowledge topic will be reviewed periodically and updated as best practice evidence and practice change. The information in this topic strives to adhere to Institute for Safe Medication Practices (ISMP) safety standards and align with Quality and Safety initiatives and accreditation requirements such as the Required Organizational Practices. -

Risks Associated with Drug Treatments for Kidney Stones
View metadata, citation and similar papers at core.ac.uk brought to you by CORE provided by IUPUIScholarWorks Risks Associated with Drug Treatments for Kidney Stones 1Nadya York, M.D., 2Michael S. Borofsky, M.D., and 3James E. Lingeman, M.D. 1Fellow in Endourology and SWL, Indiana University School of Medicine, Dept. of Urology 2Fellow in Endourology and SWL, Indiana University School of Medicine, Dept. of Urology 3Professor of Urology, Indiana University School of Medicine Corresponding Author James E. Lingeman, M.D., FACS 1801 North Senate Blvd., Suite 220 Indianapolis, IN 46202 Phone: 317/962-2485 FAX: 317/962-2893 [email protected] __________________________________________________________________________________________ This is the author's manuscript of the article published in final edited form as: York, N. E., Borofsky, M. S., & Lingeman, J. E. (2015). Risks associated with drug treatments for kidney stones. Expert Opinion on Drug Safety, 14(12), 1865–1877. http://doi.org/10.1517/14740338.2015.1100604 2. Abstract Introduction: Renal stones are one of the most painful medical conditions patients experience. For many they are also a recurrent problem. Fortunately, there are a number of drug therapies available to treat symptoms as well as prevent future stone formation. Areas covered: Herein, we review the most common drugs used in the treatment of renal stones, explaining the mechanism of action and potential side effects. Search of the Medline databases and relevant textbooks was conducted to obtain the relevant information. Further details were sourced from drug prescribing manuals. Recent studies of drug effectiveness are included as appropriate. Expert opinion: Recent controversies include medical expulsive therapy trials and complex role of urinary citrate in stone disease. -

Flexible Ureteroscopic Laser Lithotripsy for Upper Urinary Tract Stone Disease in Patients with Spinal Cord Injury
Urolithiasis DOI 10.1007/s00240-015-0786-0 ORIGINAL PAPER Flexible ureteroscopic laser lithotripsy for upper urinary tract stone disease in patients with spinal cord injury Abdulkadir Tepeler1 · Brian C. Sninsky1 · Stephen Y. Nakada1 Received: 12 January 2015 / Accepted: 12 May 2015 © Springer-Verlag Berlin Heidelberg 2015 Abstract The objective of this study is to present the hyperuricosuria (n: 1) were common abnormalities in 24-h outcomes of flexible ureteroscopic laser lithotripsy (URS) urine analysis. Ureteroscopic laser lithotripsy can be an for upper urinary tract stone disease in spinal cord injury effective treatment modality for SCI patients with upper (SCI) patients performed by a single surgeon. A retrospec- urinary tract calculi. tive analysis was performed for SCI patients treated with flexible URS for proximal ureter and kidney stone disease Keywords Spinal cord injury · Urolithiasis · by a single surgeon between 2003 and 2013. Patient char- Ureteroscopy · Laser lithotripsy acteristics, operative outcomes, metabolic evaluation, and stone analyses were assessed in detail. A total of 27 URS procedures were performed for urolithiasis in 21 renal Introduction units of 19 patients. The mean age was 52.1 15.6 years ± (16–72) and mean BMI was 29.2 7.3 kg/m2 (20–45.7). Spinal cord injury (SCI) causes neurologic problems ± Etiology of SCI was trauma (n: 10), multiple sclerosis (n: including deterioration of sensorial, motor and autonomic 6), cerebrovascular accident (n: 1), or undetermined (n: 2). functions, leading to restricted physical activity, bladder The mean stone size was 15.9 8.6 (6–40) mm. In the and bowel dysfunction, and metabolic alterations. -

Calcium Kidney Stones Are Associated with Increased Risk Of
Journal of Clinical Medicine Article Calcium Kidney Stones are Associated with Increased Risk of Carotid Atherosclerosis: The Link between Urinary Stone Risks, Carotid Intima-Media Thickness, and Oxidative Stress Markers Ho Shiang Huang 1,2, Pao Chi Liao 3 and Chan Jung Liu 1,* 1 Department of Urology, National Cheng Kung University Hospital, College of Medicine, National Cheng Kung University, Tainan 70403, Taiwan; [email protected] 2 Department of Urology, College of Medicine, National Cheng Kung University, Tainan 70403, Taiwan 3 Department of Environmental and Occupational Health, Medical College, National Cheng Kung University, Tainan 70403, Taiwan; [email protected] * Correspondence: [email protected]; Tel.: +886-6-235-3535 (ext. 5251); Fax: +886-6-276-6179 Received: 7 February 2020; Accepted: 6 March 2020; Published: 8 March 2020 Abstract: Previous studies have suggested that kidney stone formers are associated with a higher risk of cardiovascular events. To our knowledge, there have been no previous examinations of the relationship between carotid intima-media thickness (IMT) and urinary stone risk factors. This study was aimed toward an investigation of the association between dyslipidemia, IMT, and 24-hour urinalysis in patients with calcium oxalate (CaOx) or calcium phosphate (CaP) stones. We prospectively enrolled 114 patients with kidney stones and 33 controls between January 2016 and August 2016. All patients were divided into four groups, according to the stone compositions—CaOx 50% group, CaP group, struvite group, and uric acid stones group. Carotid IMT and the carotid ≥ score (CS) were evaluated using extracranial carotid artery doppler ultrasonography. The results of a multivariate analysis indicated that a higher serum total cholesterol (TC) and low-density lipoprotein (LDL) were all associated with lower urinary citrate and higher CS in both the CaOx 50% and CaP ≥ groups. -

Public Use Data File Documentation
Public Use Data File Documentation Part III - Medical Coding Manual and Short Index National Health Interview Survey, 1995 From the CENTERSFOR DISEASECONTROL AND PREVENTION/NationalCenter for Health Statistics U.S. DEPARTMENTOF HEALTHAND HUMAN SERVICES Centers for Disease Control and Prevention National Center for Health Statistics CDCCENTERS FOR DlSEASE CONTROL AND PREVENTlON Public Use Data File Documentation Part Ill - Medical Coding Manual and Short Index National Health Interview Survey, 1995 U.S. DEPARTMENT OF HEALTHAND HUMAN SERVICES Centers for Disease Control and Prevention National Center for Health Statistics Hyattsville, Maryland October 1997 TABLE OF CONTENTS Page SECTION I. INTRODUCTION AND ORIENTATION GUIDES A. Brief Description of the Health Interview Survey ............. .............. 1 B. Importance of the Medical Coding ...................... .............. 1 C. Codes Used (described briefly) ......................... .............. 2 D. Appendix III ...................................... .............. 2 E, The Short Index .................................... .............. 2 F. Abbreviations and References ......................... .............. 3 G. Training Preliminary to Coding ......................... .............. 4 SECTION II. CLASSES OF CHRONIC AND ACUTE CONDITIONS A. General Rules ................................................... 6 B. When to Assign “1” (Chronic) ........................................ 6 C. Selected Conditions Coded ” 1” Regardless of Onset ......................... 7 D. When to Assign -

Ureteroscopic Treatment of Larger Renal Calculi (>2 Cm)
Thomas Jefferson University Jefferson Digital Commons Department of Urology Faculty Papers Department of Urology 9-1-2012 Ureteroscopic treatment of larger renal calculi (>2 cm). Demetrius H. Bagley Thomas Jefferson University Kelly A. Healy Thomas Jefferson University Nir Kleinmann Thomas Jefferson University Follow this and additional works at: https://jdc.jefferson.edu/urologyfp Part of the Urology Commons Let us know how access to this document benefits ouy Recommended Citation Bagley, Demetrius H.; Healy, Kelly A.; and Kleinmann, Nir, "Ureteroscopic treatment of larger renal calculi (>2 cm)." (2012). Department of Urology Faculty Papers. Paper 45. https://jdc.jefferson.edu/urologyfp/45 This Article is brought to you for free and open access by the Jefferson Digital Commons. The Jefferson Digital Commons is a service of Thomas Jefferson University's Center for Teaching and Learning (CTL). The Commons is a showcase for Jefferson books and journals, peer-reviewed scholarly publications, unique historical collections from the University archives, and teaching tools. The Jefferson Digital Commons allows researchers and interested readers anywhere in the world to learn about and keep up to date with Jefferson scholarship. This article has been accepted for inclusion in Department of Urology Faculty Papers by an authorized administrator of the Jefferson Digital Commons. For more information, please contact: [email protected]. Arab Journal of Urology (2012) 10, 296–300 Arab Journal of Urology (Official Journal of the Arab