Katherine Public Hearing
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-
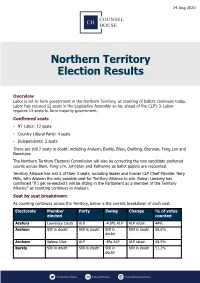
Northern Territory Election Results
24 Aug 2020 Northern Territory Election Results Overview Labor is set to form government in the Northern Territory, as counting of ballots continues today. Labor has secured 12 seats in the Legislative Assembly so far, ahead of the CLP’s 3. Labor requires 13 seats to form majority government. Confirmed seats • NT Labor: 12 seats • Country Liberal Party: 4 seats • Independents: 2 seats There are still 7 seats in doubt, including Araluen, Barkly, Blain, Braitling, Brennan, Fong Lim and Namatjira. The Northern Territory Electoral Commission will also be correcting the two candidate preferred counts across Blain, Fong Lim, Johnston and Katherine as ballot papers are recounted. Territory Alliance has lost 2 of their 3 seats, including leader and former CLP Chief Minister Terry Mills, with Araluen the only possible seat for Territory Alliance to win. Robyn Lambley has confirmed “if I get re-elected I will be sitting in the Parliament as a member of the Territory Alliance” as counting continues in Araluen. Seat by seat breakdown: As counting continues across the Territory, below is the current breakdown of each seat. Electorate Member Party Swing Change % of votes elected counted Arafura Lawrence Costa ALP -4.0% ALP ALP retain 44% Araluen Still in doubt Still in doubt Still in Still in doubt 68.6% doubt Arnhem Selena Uibo ALP -8% ALP ALP retain 48.9% Barkly Still in doubt Still in doubt Still in Still in doubt 51.2% doubt Blain Still in doubt Still in doubt Still in doubt Still in doubt 65% Braitling Still in doubt Still in doubt Still in doubt -

Agenda Item 7.1 REPORT Report No
Agenda Item 7.1 REPORT Report No. 144/17cncl TO: ORDINARY COUNCIL – MONDAY 11 SEPTEMBER 2017 SUBJECT: MAYOR’S REPORT 1. MEETINGS AND APPOINTMENTS 1.1 Lord Mayor of Darwin Katrina Fong Lim 1.2 Kerry Moir and Tony Tapsell, CEO LGANT 1.3 Terry-Ann Maney, Australian Institute of Company Directors 1.4 Stephen Nugent , Advisor to Minister for Tourism and Culture 1.5 Gary Powell, Regional Manager of Central Australia Indigenous Affairs Department, Prime Minister and Cabinet 1.6 Chief Minister Michael Gunner 1.7 Gary Higgins MLA, Leader of the Opposition 1.8 Steve Moore, CEO Barkly Regional Council 1.9 Tony Tapsell, CEO LGANT 1.10 Mayor David O’Loughlin, ALGA President 1.11 Steve Edgington, President Barkly Regional Council 1.12 City of Darwin Lord Mayor Kon Vataskallis 1.13 The Hon. Nicole Manison, NT Treasurer and Richard O’Leary, Advisor 1.14 Alice Springs Town Council – Planning for Great Northern Clean Up 1.15 Ian Coleman, Curator Olive Pink Botanic Garden 1.16 Craig Markham, Paul Tottani, Councillor de Brenni and Dale McIver 1.17 Susan Bradbrook, Governance Institute Australia 1.18 Judith Dixon – Central Australian Development Office 1.19 The Hon. Lauren Moss, Minister for Tourism and Culture 1.20 Chansey Paech MLA, Member for Namatjira 1.21 Litchfield Council Mayor Maree Bredhauer 1.22 Steve Hennessy, Northern Territory Grants Commission 1.23 Boulia Shire Mayor Rick Britton – Outback Way AGM 2. FUNCTIONS ATTENDED 2.1 Red CentreNATS – Volunteers and Officials Welcome, Star of Alice 2.2 Welcome Reception – Red CentreNATS, Alice Springs Convention Centre 2.3 St Philip’s College Musical – Little Women 2.4 Heritage Council Lunch, Mercure Hotel Alice Springs 2.5 Charles Darwin University Campus Industry night 2.6 Reception for Aboriginal Rangers hosted by The Hon. -

Darwin Public Hearing
LEGISLATIVE ASSEMBLY OF THE NORTHERN TERRITORY 11th Assembly Select Committee on Youth Suicides in the NT Public Hearing Transcript 10.30 am, Monday 30 January 2012 Nitmiluk Lounge, Parliament House Members: Ms Marion Scrymgour, MLA Chair, Member for Arafura Mr Michael Gunner, MLA, Member for Fannie Bay Ms Lynne Walker, MLA, Member for Nhulunbuy Ms Kezia Purick, MLA, Member for Goyder Mr Peter Styles, MLA, Member for Sanderson Witnesses: NT CHILDREN’S COMMISSION Dr Howard Bath, NT Children’s Commissioner and Convener of the Child Deaths Review Committee Mr Adam Harwood, Senior Policy Officer CENTRAL AUSTRALIAN YOUTH LINK-UP SERVICE Mr Blair McFarland, Manager WESLEY MISSION LIFE FORCE SUICIDE PREVENTION PROGRAM Mr Tony Cassidy, Program Manager YOUTH MINISTER’S ROUND TABLE OF YOUNG TERRITORIANS Ms Karen Folkers, Project Officer Ms Alpha Capaque, Youth Representative Ms Lauren Moss, Youth Representative Ms Tylee Wirth, Youth Representative NORTHERN TERRITORY COUNCIL OF SOCIAL SERVICES Ms Tess Reinsch, Youth Policy Officer Ms Christa Bartjen-Westermann, Acting Coordinator Central Australia 1 Select Committee - Youth Suicides in the Northern Territory – 30 January 2012 CHILDREN’S COMMISSIONER/CONVENOR OF CHILD DEATHS REVIEW AND PREVENTION COMMITTEE Dr Howard Bath Mr Adam Harwood Madam CHAIR: On behalf of the select committee I welcome the Children’s Commissioner, Dr Howard Bath, to this public hearing into current and emerging issues of youth suicide in the Northern Territory. We have had a couple of attempts and have had to cancel. I thank you for appearing before the committee today. We appreciate you taking the time to speak to the committee and look forward to hearing from you. -

Labor-Ind Seats CLP-Ind Seats % % 53.9
Northern Territory Electoral Pendulum 2020 Labor 14 Independent 1 CLP 8 Independent 2 Total 15 Majority 5 Total 10 Labor-Ind Seats CLP-Ind Seats % % 25 24.3 Nightcliff Nelson (CLP) 22.8 25 20 20 23 19.3 Sanderson 21 17.7 Arnhem 19 17.3 Wanguri 17 16.6 Johnston Spillett (CLP) 15.1 23 SWING TO LABOR PARTY TO SWING 15 16.3 Gwoja SWING TO COUNTRY LIBERAL PARTY COUNTRY TO SWING 13 16.1 Mulka (Ind) 11 16.0 Casuarina 15 15 Goyder (Ind) 14.4 21 Araluen (Ind) 12.7 19 10 10 9 9.8 Karama 7 9.6 Fannie Bay 8 8 5 7.9 Drysdale 4 4 3 3 2 1 1 2 Arafura C Katherine (CLP) L 3.6 P 3 - I n Braitling (CLP) d Brennan (CLP) Fong Lim Namatjira (CLP) M Daly (CLP) a 2.7 Barkly (CLP) jo Port Darwin 2.4 r it y 1 2.1 17 1.3 3 1.3 Blain L 1.2 a b 0.4 15 o 0.1 r - 13 I 0.2 nd M 11 53.9% Labor aj 46.1% CLP o 9 r 7 ity 5 KEY 3.6 Swing required to take seat 3 Majority in seats Result of general election, 22 August 2020 Northern Territory : Two-Party Preferred Votes by Division, 22 August 2020 Division Labor Votes % CLP Votes % %Swing to CLP %Swing Needed Winner Arafura 1,388 53.57 1,203 46.43 3.2 3.6 Lawrence Costa (Labor) Araluen⁽a⁾ 1,630 37.35 2,734 62.65 3.0 12.7 Robyn Lambley (Ind) Arnhem⁽b⁾ 1,977 67.61 947 32.39 -5.2 17.7 Selena Uibo (Labor) Barkly 1,717 49.90 1,724 50.10 16.0 0.1 Steve Edgington (CLP) Blain 2,095 50.16 2,082 49.84 -1.5 0.2 Mark Turner (Labor) Braitling 2,141 48.71 2,254 51.29 4.4 1.3 Joshua Burgoyne (CLP) Brennan 2,138 48.81 2,242 51.19 3.8 1.2 Marie-Clare Boothby (CLP) Casuarina 3,035 65.96 1,566 34.04 -4.6 16.0 Lauren Moss (Labor) Daly 1,890 48.79 -
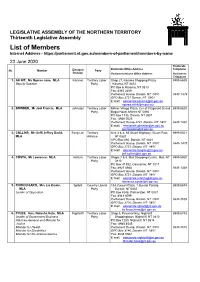
List of Members Internet Address
LEGISLATIVE ASSEMBLY OF THE NORTHERN TERRITORY Thirteenth Legislative Assembly List of Members Internet Address - https://parliament.nt.gov.au/members-of-parliament/members-by-name 23 June 2020 Electorate Electoral Electorate Office Address Telephone No. Member Party Division Parliament House Office Address Parliament Telephone 1. AH KIT, Ms Ngaree Jane, MLA Karama Territory Labor Shop 27, Karama Shopping Plaza, 8999 6659 Deputy Speaker Party Karama, NT 0812 PO Box 6, Karama, NT 0813 Fax: 8945 2090 Parliament House, Darwin, NT 0800 8946 1479 GPO Box 3721 Darwin, NT 0801 E:mail: [email protected] [email protected] 2. BOWDEN, Mr Joel Francis, MLA Johnston Territory Labor Millner Village Plaza, Cnr of Fitzgerald St and 8999 6620 Party Bagot Road, Millner NT 0810 PO Box 1135, Darwin, NT 0801 Fax: 8948 0525 Parliament House 3721, Darwin, NT 0801 8946 1490 E:mail: [email protected] [email protected] 3. COLLINS, Mr (Jeff) Jeffrey David, Fong Lim Territory Unit 3 & 4, 65 Stuart Highway, Stuart Park, 8999 6501 MLA Alliance NT 0820 GPO Box 892, Darwin, NT 0801 Parliament House, Darwin, NT 0800 8946 1475 GPO Box 3721, Darwin, NT 0801 E:mail: [email protected] [email protected] 4. COSTA, Mr Lawrence, MLA Arafura Territory Labor Shops 7 & 8, Moil Shopping Centre, Moil, NT 8999 6950 Party 0810 PO Box 41392, Casuarina, NT 0811 Fax: 8927 0988 8946 1438 Parliament House, Darwin, NT 0800 GPO Box 3721, Darwin, NT 0801 E:mail: [email protected] [email protected] 5. -

Lambley Clinging on to Alliance
MONDAY AUGUST 24 2020 NEWS 05 EVERY vote counts Number every square in NT LEGISLATIVEVoting is compulsory ASSEMBLY ELECTION 2020 the TerritoryHave your say votes this election day the order of your choice VOTE 1 Four seats still hang in the balance MADURA MCCORMACK AND Neither Chief Minister Mi- NATASHA EMECK IN THIS ELECTION THE chael Gunner nor Opposition INTRODUCTION OF A THIRD Leader Lia Finocchiaro made THE political future of Labor MAJOR PARTY MADE THE an appearance yesterday and frontbencher Selena Uibo and it’s understood the CLP leader candidates in three other key ''DETERMINATION OF THE has not yet called Mr Gunner seats could be decided today as TCP FOR ELECTION NIGHT to concede defeat. the NT Electoral Commission MORE DIFFICULT At the moment Labor has shifts into full count mode. comfortably claimed Fannie The NTEC will be correct- Bay, Wanguri, Nightcliff, Cas- NTEC Natasha Fyles enjoys the ing the two candidate pre- uarina, Karama, Gwoja, Sand- Nightcliff markets on Sunday ferred counts across five seats, erson, Johnston, Port Darwin chatting with Anne Kleinitz and four of which remained in NTEC staff able to finish up in and Drysdale. and Arafura has her niece Billie Boyer, 4. doubt yesterday, as ballot pa- less than three hours. more than likely been won by Picture: CHE CHORLEY pers are recounted. Overall, the postal vote flow Labor’s Lawrence Costa. Algorithms in Arnhem will has had minimal impact on the Labor has maybe lost Brait- switch to projected flows be- outcome thus far, though elec- ling’s Dale Wakefield, though tween Ms Uibo, who is ahead tion boffins, including Tas- Charles Darwin University on first preferences, and inde- mania’s Kevin Bonham and Professor Rolf Gerritsen thinks pendent Ian Gumbula while ABC’s Antony Green, have there’s a slim chance she could Katherine, Fong Lim and Blain tipped Labor’s Sid Vashist to pull through on preference. -

Royal Life Saving NT Annual Report 2017-2018
Annual Report 2017/2018 1 ABN 57 939 760 839 Royal Life Saving Society - Australia – NT is an Incorporated Entity (A 1328) and a Public Benevolent Institution. RTO Provider Number 0859 This annual report covers the financial year 1 July 2015 to 30 June 2016. Royal Life Saving Society (Australia) NT Branch is located at: 77 Ross Smith Avenue, Parap, NT 0820 Postal: GPO Box 1229, Darwin NT 0801 Telephone: (08) 8981 5036 Email: [email protected] Web: www.royallifesaving.com.au “Our People, Our Lifestyle, Our Water” 2 MESSAGE FROM OUR PATRONS HER HONOUR VICKI O’HALLORAN AM AND MR CRAIG O’HALLORAN ........................ 3 MESSAGE FROM THE PRESIDENT RANDALL COOK ........................................................................................................ 4 REPORT FROM THE EXECUTIVE DIRECTOR .................................................................................................................... 5 HIGHLIGHTS OF THE YEAR 2017/2018 ........................................................................................................................... 6 OUR ORGANISATION .................................................................................................................................................... 7 HISTORY OF RLSSA NT ........................................................................................................................................................... 7 Our Mission: .................................................................................................................................................................. -

Northern Territory Election Outcome August 2020 on 22 August 2020
Northern Territory election outcome August 2020 On 22 August 2020 Northern Territory Labor was returned to Government, having won a majority of seats in the Northern Territory (NT) Parliament. On Monday 7 September the Chief Minister announced the composition of the new Ministry. Contents Further information................................................................................................................................................ 1 Northern Territory Ministry ................................................................................................................................... 2 Results .................................................................................................................................................................... 3 Key influencing factors: .......................................................................................................................................... 3 Seat by seat results................................................................................................................................................. 4 History of Elections 1997-20126 ............................................................................................................................ 5 Chief Minister– The Hon Michael Gunner MP ....................................................................................................... 5 Further information For more information, please contact your Hawker Britton consultant, Queensland and Northern Territory Director, -

2016 NORTHERN TERRITORY ELECTION 27 August 2016
2016 NORTHERN TERRITORY ELECTION 27 August 2016 CONTENTS Page Introduction ............................................................................................................................. Summary of Legislative Assembly Election ........................................................................... 3 Legislative Assembly Results by Electoral Division ............................................................... 6 By-elections 2012-2016 ...................................................................................................... 11 Summary of Two-Party and Tw-Candidate Preferred Results ............................................. 12 Regional Summaries ........................................................................................................... 16 Elected and Defeated Members .......................................................................................... 18 Summary of Redistribution .................................................................................................. 19 List of Candidate ................................................................................................................. 20 Prepared by Antony Green – ABC Election Unit1 Symbols .. Nil or rounded to zero * Sitting MPs .… ‘Ghost’ candidate, where a party contesting the previous election did not nominate for the current election (n.a.) Not available Party Abbreviations - Non-affiliated candidates 1TP 1 Territory Party ALP Australian Labor Party ASX Australian Sex Party (contested 2012 election) -

August 2020 Election
August 2020 Election WHO & WHERE GUIDE This guide will tell you: - What are the different Electorates in the NT - Which electorate your community, town, homeland or suburb falls into - Who is the current politician for your area, called Member of Parliament (MLA) - Who are some of the other people running to be elected for your area What Letters stand for: If a politican has an Aboriginal flag - MLA - member of Parliament next to their name, that means they ALP - Australian Labor Party identify as Aboriginal or Torres Strait CLP- Country Liberal Party Islander Territory Alliance There are three big parties running in the NT election, NT Labor, Country Liberal Party and Territory Alliance. There are also people who run as Independents, and people who run in smaller parties. If an electorate page is yellow, that means an Independent is the representative in Parliament for that area If the electorate page is red, that means Labor are the representatives for that area If an electorate page is organge, that means Country Liberal party are the representatives for that area And if it is dark blue, that means Territory Alliance are the representaives for that area. Authorised by A.Telford of the Australian Youth Climate Coalition, Queen St Brisbane, Printed and funded by Seed Indigenous Climate Network MULKA Where: Nhulunbuy, Galiwinku, Yirrkala, Ramingining, Galinwinku Current MLA: Mr Yingiya (Mark) Guyula (Independent) ALP candidate: Lynne Walker Authorised by A.Telford of the Australian Youth Climate Coalition, Queen St Brisbane, Printed and funded by Seed Indigenous Climate Network Barkly Where: Barkly Tableland, the regional centre of Tennant Creek and the communities of Ali Curung, Alpurrurulam, Ampilatwatja, Arlparra, Borroloola, Daly Waters, Elliott, Larrimah, and Ti Tree. -

LEGISLATIVE ASSEMBLY of the NORTHERN TERRITORY Thirteenth Legislative Assembly
LEGISLATIVE ASSEMBLY OF THE NORTHERN TERRITORY Thirteenth Legislative Assembly List of Members – Internet Address - http://www.nt.gov.au/lant 9 January 2017 Electorate Electoral Electorate Office Address Telephone No. Member Party Division Parliament House Office Address Parliament Telephone 1. AH KIT, Ngaree Jane, MLA Karama A.L.P Shop 27, Karama Shopping Plaza, 8999 6659 Karama, NT 0812 PO Box 6, Karama, NT 0813 Fax: 8945 2090 Parliament House, Darwin, NT 0800 8946 1411 GPO Box 3721 Darwin, NT 0801 E:mail: [email protected] [email protected] 2. COLLINS, (Jeff) Jeff rey David , MLA Fong Lim A.L.P Unit 4 & 5, 65 Stuart Highway, Stuart Park, 8999 6501 NT 0820 GPO Box 892, Darwin, NT 0801 Parliament House, Darwin, NT 0800 8946 1475 GPO Box 3721, Darwin, NT 0801 E:mail: [email protected] [email protected] 3. COSTA, Lawrence, MLA Arafura A.L.P Shop 7 & 8, Moil Shopping Centre, Moil, NT 8999 6950 0810 PO Box 41392, Casuarina, NT 0811 Parliament House, Darwin, NT 0800 8946 1438 GPO Box 3721, Darwin, NT 0801 E:mail: [email protected] [email protected] 4. FINOCCHIARO, Lia Emele, MLA Spillett C.L. Shop 20, Winnellie Shopping Centre, 8999 6667 Deputy Leader of Opposition Winnellie, NT 0820 Opposition Whip PO Box 4248, Palmerston, NT 0831 Fax: 8941 8099 Parliament House, Darwin, NT 0800 8946 1471 GPO Box 3700, Darwin, NT 0801 E:mail: [email protected] [email protected] 5. FYLES, Hon. Natasha Kate, MLA Nightcliff A.L.P Shop 5, Pavonia Way, Nightcliff 8999 6743 Leader of Government Business Shoppingtown, Nightcliff, NT 0810 Attorney-General and Minister for Justice PO Box 1283, Nightcliff, NT 0814 Minister for Health Fax: 8985 4545 Parliament House, Darwin, NT 0800 8936 5610 GPO Box 3146, Darwin, NT 0801 Fax: 8936 5562 E:mail: [email protected] [email protected] 6. -
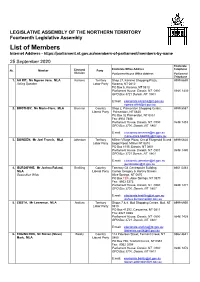
List of Members Internet Address
LEGISLATIVE ASSEMBLY OF THE NORTHERN TERRITORY Fourteenth Legislative Assembly List of Members Internet Address - https://parliament.nt.gov.au/members-of-parliament/members-by-name 25 September 2020 Electorate Electoral Electorate Office Address Telephone No. Member Party Division Parliament House Office Address Parliament Telephone 1. AH KIT, Ms Ngaree Jane, MLA Karama Territory Shop 27, Karama Shopping Plaza, 8999 6659 Acting Speaker Labor Party Karama, NT 0812 PO Box 6, Karama, NT 0813 Parliament House, Darwin, NT 0800 8946 1433 GPO Box 3721 Darwin, NT 0801 E:mail: [email protected] [email protected] 2. BOOTHBY, Ms Marie-Clare, MLA Brennan Country Shop 2, Palmerston Shopping Centre, 8999 5587 Liberal Party Palmerston, NT 0830 PO Box 32 Palmerston, NT 0831 Fax: 8932 7488 Parliament House, Darwin, NT 0800 8946 1453 GPO Box 3700, Darwin, NT 0801 E:mail: [email protected] [email protected] 3. BOWDEN, Mr Joel Francis, MLA Johnston Territory Millner Village Plaza, Cnr of Fitzgerald St and 8999 6620 Labor Party Bagot Road, Millner NT 0810 PO Box 1135, Darwin, NT 0801 Parliament House, Darwin, NT 0801 8946 1446 GPO Box 3721 Darwin, NT 0801 E:mail: [email protected] [email protected] 4. BURGOYNE, Mr Joshua Roland, Braitling Country Tenancy G4 Centrepoint Building 8951 5463 MLA Liberal Party Corner Gregory & Hartley Streets Opposition Whip Alice Springs, NT 0870 PO Box TBA, Alice Springs, NT 0871 Fax: 8952 5373 Parliament House, Darwin, NT 0800 8946 1471 GPO Box 3700, Darwin, NT 0801 E:mail: [email protected] [email protected] 5.