Allergen Components Tests and What They Mean
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Recurrent Angioedema Due to Lysozyme Allergy R Pérez-Calderón, MA Gonzalo-Garijo, a Lamilla-Yerga, R Mangas-Santos, I Moreno-Gastón
R Pérez-Calderón, et al CASE REPORT Recurrent Angioedema Due to Lysozyme Allergy R Pérez-Calderón, MA Gonzalo-Garijo, A Lamilla-Yerga, R Mangas-Santos, I Moreno-Gastón Department of Allergology, Infanta Cristina University Hospital, Badajoz, Spain ■ Abstract A 54-year-old woman suffered an episode of dyspnea and edema affecting her eyelids, tongue, and lips a few minutes after intake of Lizipaina (bacitracin, papain, and lysozyme). She was treated with intravenous drugs and her symptoms improved within 2 hours. She had experienced 3 to 4 bouts of similar symptoms related to the ingestion of cured cheeses or raw egg. Specifi c serum immunoglobulin (Ig) E against lysozyme was present at a concentration of 0.45 kU/L, and no specifi c IgE was found against egg white and yolk, ovalbumin, or ovomucoid. Skin prick tests were positive with commercial extracts of egg white and lysozyme but doubtful with yolk, ovalbumin, and ovomucoid. Prick-to-prick tests with raw egg white and yolk gave positive results, but negative results were obtained with cooked egg white and yolk and 5 brands of cheese (3 of them containing lysozyme and the other 2 without lysozyme). Controlled oral administration of papain, bacitracin, and cheeses without lysozyme was well tolerated. We suggest that the presence of lysozyme in a pharmaceutical preparation, cured cheese, and raw egg was responsible for the symptoms suffered by our patient, probably through an IgE-mediated mechanism. Key words: Additives. Drug allergy. Food allergy. Hypersensitivity. Lysozyme. ■ Resumen Mujer de 54 años de edad, que presentó un cuadro de disnea y edema de párpados, lengua y labios a los pocos minutos de tomar un comprimido de Lizipaina (bacitracina, papaína y lisozima). -
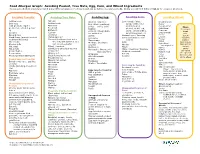
Avoiding Peanut, Tree Nuts, Egg, Corn, and Wheat Ingredients Common Food Allergens May Be Listed Many Different Ways on Food Labels and Can Be Hidden in Common Foods
Food Allergen Graph: Avoiding Peanut, Tree Nuts, Egg, Corn, and Wheat Ingredients Common food allergens may be listed many different ways on food labels and can be hidden in common foods. Below you will find different labels for common allergens. Avoiding Peanuts: Avoiding Tree Nuts: Avoiding Egg: Avoiding Corn: Avoiding Wheat: Artificial nuts Almond Albumin / albumen Corn - meal, flakes, Bread Crumbs Beer nuts Artificial nuts Egg (dried, powdered, syrup, solids, flour, Bulgur Cold pressed, expeller Brazil nut solids, white, yolk) niblets, kernel, Cereal extract Flour: pressed or extruded peanut Beechnut Eggnog alcohol, on the cob, Club Wheat all-purpose Butternut oil Globulin / Ovoglobulin starch, bread,muffins Conscous bread Goobers Cashew Fat subtitutes sugar/sweetener, oil, Cracker meal cake Durum Ground nuts Chestnut Livetin Caramel corn / flavoring durum Einkorn Mandelonas (peanuts soaked Chinquapin nut Lysozyme Citric acid (may be corn enriched Emmer in almond flavoring) Coconut (really is a fruit not a based) graham Mayonnaise Farina Mixed nuts tree nut, but classified as a Grits high gluten Meringue (meringue Hydrolyzed Monkey nuts nut on some charts) high protein powder) Hominy wheat protein Nut meat Filbert / hazelnut instant Ovalbumin Maize Kamut Gianduja -a chocolate-nut mix pastry Nut pieces Ovomucin / Ovomucoid / Malto / Dextrose / Dextrate Matzoh Peanut butter Ginkgo nut Modified cornstarch self-rising Ovotransferrin Matzoh meal steel ground Peanut flour Hickory nut Polenta Simplesse Pasta stone ground Peanut protein hydrolysate -

Investigating the Chemical Basis of Functionality Differences Between Beet and Cane Sugar Sources in Model Egg White Foams and Other Products
INVESTIGATING THE CHEMICAL BASIS OF FUNCTIONALITY DIFFERENCES BETWEEN BEET AND CANE SUGAR SOURCES IN MODEL EGG WHITE FOAMS AND OTHER PRODUCTS BY NICHOLAS REITZ THESIS Submitted in partial fulfillment of the requirements for the degree of Master of Science in Food Science and Human Nutrition with a concentration in Food Science in the Graduate College of the University of Illinois at Urbana-Champaign, 2016 Urbana, Illinois Adviser: Professor Shelly J. Schmidt ABSTRACT Though often used interchangeably, researchers have identified differences in functionality between beet and cane sugar sources in some food products. For example, previous research reported sensory differences between meringue cookies made with beet and cane sugar. Beet sugar meringue cookies were more marshmallow-like than cane meringue cookies. However, these sensory differences have not been instrumentally quantified and the underlying cause has not been determined. Thus, the objective of this research was to instrumentally quantify and investigate the chemical basis for the sensory differences between beet and cane meringue cookies. To instrumentally quantify differences between beet and cane meringue cookies, moisture content and water activity was obtained for unbaked meringues and meringue cookies. Additionally, texture profile analysis, three point break analysis, and differential scanning calorimetry was carried out on beet and cane meringue cookies. To gain insight into factors causing differences between beet and cane meringue cookies, heat denatured sugar-egg gel texture, unbaked foam stability, and water loss during simulated baking were obtained. No meaningful difference was found between beet and cane meringues in moisture content, water activity, and foam stability prior to baking. After baking, however, beet meringue cookies where shown to have higher moisture content, water activity, and cohesiveness values, and lower hardness and force to break values. -

Functional Proteins and Peptides of Hen's Egg Origin
Chapter 5 Functional Proteins and Peptides of Hen’s Egg Origin Adham M. Abdou, Mujo Kim and Kenji Sato Additional information is available at the end of the chapter http://dx.doi.org/10.5772/54003 1. Introduction Hen’s egg has long history as a food. It contains a great variety of nutrients to sustain both life and growth. Egg provides an excellent, inexpensive and low calorie source of high- quality proteins. Moreover, Eggs are a good source of several important nutrients including protein, total fat, monounsaturated fatty acids, polyunsaturated fatty acids, cholesterol, choline, folate, iron, calcium, phosphorus, selenium, zinc and vitamins A, B2, B6, B12, D, E and K [1]. Eggs are also a good source of the antioxidant carotenoids, lutein and zeaxanthin [2]. The high nutritional properties of eggs make them ideal for many people with special dietary requirements. Egg proteins are nutritionally complete with a good balance of essential amino acids which are needed for building and repairing the cells in muscles and other body tissues [3]. Egg proteins are distributed in all parts of the egg, but most of them are present in the egg white and egg yolk amounting to 50% and 40%, respectively. The remaining amount of protein is in the egg shell and egg shell membranes. In addition to excellent nutritional value, egg proteins have unique biological activities. Hyperimmunized hens could provide a convenient and economic source of specific immunoglobulin in their yolks (IgY) that have been found to be effective in preventing many bacteria and viruses infections [4]. Proteins in the egg white as lysozyme, ovotransferrin, and avidin have proven to exert numerous biological activities. -

Test Instruction Allergenic
General Information Hen’s egg (Gallus gallus) is very rich of proteins and represents an important food source for humans. While proteins of egg yolk only have minor aller- genicity, many proteins of egg white are known to be Test Instruction allergenic. In addition to ovalbumin, ovotransferrin, lysozyme and livetin, ovomucoid represents the Egg White most important allergen. Unlike the other allergens ovomucoid is heat stable and can resist common 96/48 Tests production processes like baking. For allergic per- sons the consumption of egg white represents a critical problem. Already very low amounts of the Enzyme Immunoassay allergen can cause allergic reactions, which may for the Quantitative lead to anaphylactic shock in severe cases. Because Determination of of this, egg allergic persons must strictly avoid the Egg White Proteins in Food consumption of eggs or egg containing food. Non- declared addition of egg in food is hazardous for allergic people. Crosscontamination, mostly in con- Cat.-No.: HU0030007 sequence of the production process is often noticed. The chocolate production process is a repre- Version: September 25th, 2017 sentative example. For the detection of egg white protein residues, sensitive detection systems are This document represents a combined test required. instruction for the products HU0030007 The SENSISpec Egg White ELISA represents a (96 well) and HU0030031 (48 well). highly sensitive detection system for egg white pro- tein based on ovomucoid and is particularly capable of the quantification of egg white residues in pasta, bakery products, sausage and chocolate. Tecna cod. AL557-AL457 Principle of the Test The SENSISpec Egg White quantitative test is based on the principle of the enzyme linked immu- nosorbent assay. -

Egg Allergy Avoidance Hidden Names for Eggs
Egg Allergy Avoidance List Hidden Names for Egg Compiled by Debra A. Indorato RD, LDN, member of KFA’s Medical Advisory Team Foods covered by the FDA labeling laws that contain eggs must be labeled in plain English to declare that it “contains eggs.” However, there are many foods and products that are not covered by FDA allergen labeling laws, so it is still important to know how to read a label for egg ingredients. Products exempt from plain English labeling rules: foods that are not regulated by the FDA (tinyurl.com/KFA-FALCPA), cosmetics and personal care products, prescription and over-the-counter medications or supplements, pet food, toys and crafts. contain egg The following ingredients found on a label indicate the presence of egg protein. All labels should be read carefully before consuming a product, even if it has been used safely in the past. Albumin Ovalbumin may contain egg Apovitellin Ovoglobulin Artificial flavoring Cholesterol free egg substitute Ovomucin Baked goods (e.g. Eggbeaters®) Ovomucoid Lecithin Dried egg solids, dried egg Ovotransferrin Natural flavoring Egg, egg white, egg yolk Ovovitelia Nougat Egg wash Ovovitellin Pasta Eggnog Powdered eggs Fat substitutes Silici albuminate Globulin Simplesse Livetin Surimi Lysozyme Trailblazer Mayonnaise Vitellin Meringue, meringue powder Whole egg PROUDLY BROUGHT TO YOU BY For more detailed information and a list of resources, please visit KidsWithFoodAllergies.org. Rev. March 2015 Copyright ©2014, Kids With Food Allergies, a division of the Asthma and Allergy Foundation of America (AAFA), all rights reserved. TRAVEL-SIZE CARDS Egg Allergy Avoidance List Hidden Names for Egg Compiled by Debra A. -

Egg Protein Residue ELISA Kit
Egg Protein Residue ELISA Kit Catalog Number: KA3877 96 assays Version: 02 Intended for research use only www.abnova.com Table of Contents Introduction ................................................................................................... 3 Intended Use ................................................................................................................. 3 Background ................................................................................................................... 3 Principle of the Assay .................................................................................................... 3 General Information ...................................................................................... 4 Materials Supplied ......................................................................................................... 4 Storage Instruction ........................................................................................................ 4 Materials Required but Not Supplied ............................................................................. 4 Precautions for Use ....................................................................................................... 5 Assay Protocol .............................................................................................. 6 Reagent Preparation ..................................................................................................... 6 Sample Preparation ...................................................................................................... -

Egg White Proteins and Their Potential Use in Food Processing Or As Nutraceutical and Pharmaceutical Agents—A Review
Animal Science Publications Animal Science 12-1-2013 Egg white proteins and their potential use in food processing or as nutraceutical and pharmaceutical agents—A review E. D. N. S. Abeyrathne Seoul National University H. Y. Lee Seoul National University Dong U. Ahn Iowa State University, [email protected] Follow this and additional works at: https://lib.dr.iastate.edu/ans_pubs Part of the Agriculture Commons, and the Poultry or Avian Science Commons The complete bibliographic information for this item can be found at https://lib.dr.iastate.edu/ ans_pubs/885. For information on how to cite this item, please visit http://lib.dr.iastate.edu/ howtocite.html. This Article is brought to you for free and open access by the Animal Science at Iowa State University Digital Repository. It has been accepted for inclusion in Animal Science Publications by an authorized administrator of Iowa State University Digital Repository. For more information, please contact [email protected]. Egg white proteins and their potential use in food processing or as nutraceutical and pharmaceutical agents—A review Abstract Egg white contains many functionally important proteins. Ovalbumin (54%), ovotransferrin (12%), ovomucoid (11%), ovomucin (3.5%), and lysozyme (3.5%) are among the major proteins that have high potentials for industrial applications if separated. The separation methods for these proteins from egg white have been developed since early 1900, but preparation methods of these proteins for commercial applications are still under development. Simplicity and scalability of the methods, use of nontoxic chemicals for the separation, and sequential separation for multiple proteins are very important criteria for the commercial production and application of these proteins. -

INFLUENCE of LYSOZYME on EGG WHITE QUALITY DISSERTATION Presented in Partial Fulfillment of the Requirements for the Degree Doct
INFLUENCE OF LYSOZYME ON EGG WHITE QUALITY DISSERTATION Presented in Partial Fulfillment of the Requirements for the Degree Doctor of Philosophy in the Graduate School of The Ohio State University by OWEN JAY COTTERILL, B. S., M. S. The Ohio State University 19SU Approved by* Adviser i TABLE OF CONTENTS INTRODUCTION ................................................ 1 REVIEW OF LITERATURE........................................ h .Composition of Egg W h i t e ............. 5 Gross structure ............... 5 Chemical composition ............ 6 W a t e r ................................... • . • 6 Proteins • .................... ....... 7 Minerals ....... .......... ...... 10 Carbohydrates •••..•• • 10 L i p i d ........................................ 10 Vitamins . ........ 11 froperties of Egg White Proteins •••••••••••* 12 Physical ••••.«••• 12 Biological ............... lii Conalbumin ............. Ill Ovomucoid lU Avidin . .................................. 1$ Ovomucin .................................. 15 Lysozyme ............. 16 Factors Affecting Egg Whits Quality • • 19 Temperature .................................. 19 Humidity.......................................... 19 ii pH .... ...................................... 20 Disease 25 Breeding 26 Nutrition •••••... .............. ••••• 26 Season of year and age of b i r d ................... .. 27 Thermostabilization . .............. 27 Mechanism of Egg White Thinning...................... .. 30 Tiyptic digestion ..................... 30 Fibrous structure 32 Sulfhydryl groups . -

Albumen Protein and Functional Properties of Gelation and Foaming
Proteins of albumen functional properties 291 Review ALBUMEN PROTEIN AND FUNCTIONAL PROPERTIES OF GELATION AND FOAMING Ana Cláudia Carraro Alleoni R. Athaualpa Vaz de Melo, 179 - 13405-216 - Piracicaba, SP - Brasil. e-mail <[email protected]> ABSTRACT: Hen eggwhite proteins have been extensively utilized as ingredients in food processing because of their unique functional properties, such as gelling and foaming. This work reviews the molecular basis of the eggwhite proteins targeting the development of these functional properties during processing. Key words: ovalbumin, coagulation, gel, denaturation PROTEÍNAS DO ALBUME E PROPRIEDADES FUCIONAIS DE GELATINIZAÇÃO E FORMAÇÃO DE ESPUMA RESUMO: As proteínas da clara do ovo de galinha têm sido extensivamente usadas como ingredientes em alimentos processados, devido às suas propriedades funcionais, tais como gelatinização e formação de espuma. Essa revisão aborda as bases moleculares das proteínas da clara do ovo para o desenvolvimento dessas propriedades funcionais durante o processamento. Palavras-chave: ovalbumina, coagulação, gel, desnaturação INTRODUTION ALBUMEN PROTEINS The eggwhite has 9.7 to 12% protein (Vadehra Hen eggwhite have been extensively used as & Nath, 1973; Mine, 1995) and can be considered a sys- processed food ingredients, because of their functional tem built out of numerous globular proteins in an aque- properties of gelation and foam formation, ovalbumin ous solution. The seven largest fractions are ovalbumins proteins of chicken eggs have been used as processed A1 and A2, ovoglobulins G1, G2 and G3, ovomucoid and food ingredients (Mine, 1995). Gelation has evident conalbumin. Table 1 presents amounts of several pro- importance given the amount of available products to teins of eggwhite and some of their properties. -

Rabbit Anti Ovomucoid Polyclonal Antibody Application: ELISA, WB Alternate Names: Ovomucoid, OVM, OM, Trypsin Inhibitor Reactivity: Chicken
Order Information Description: Rabbit anti-Ovomucoid Catalogue#: 601-770 Lot#: See the label Size: 100 ug/200 ul Host: Rabbit Clone: N/A Rabbit anti Ovomucoid Polyclonal Antibody Application: ELISA, WB Alternate Names: Ovomucoid, OVM, OM, Trypsin inhibitor Reactivity: Chicken ANTIGEN PREPARATION A synthetic peptide corresponding to the C-terminus of chicken egg white Ovomucoid protein. BACKGROUND Ovomucoid is isolated from chicken egg white. The precursor is a 210 aa secreted protein which consists of three homologous, tandem Kazal family inhibitory domains each homologous to pancreatic secretory trypsin inhibitor (Kazal) and each with an actual or putative reactive site for inhibition of serine proteinases. The major reactive site for bovine beta-trypsin is the Arg89-Ala peptide bond in the second domain. It causes an allergic reaction in human. Allergy to chicken egg or proteins is one of the most frequent causes of food hypersensitivity in infants and young children. Both IgG and IgA class antibodies may be detected. Ovalbumin intolerance has been implicated in a number of conditions affecting children. In particular, children with cystic fibrosis show elevated anti-Ovalbumin antibodies. Ovalbumin antibodies have also been noted in some forms of kidney disease. A relationship between food allergy and infantile autism has also been observed. Children with insulin-dependent diabetes mellitus show an enhanced immune response to both β- actoglobulin and ovalbumin, a phenomenon that may be related to the development of the disease. Conditions related to ovalbumin intolerance usually resolve once egg and egg based foods have been withdrawn from the patient's diet. Intolerance to egg proteins could be due not only to the ovalbumin protein found in egg white but also to other major proteins present in the yolk.