Heterogeneity of Patients in Clinical Trials Subgroup Analysis and Covariate Adjustment in Cardiovascular and Neurosurgical Trials
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

A Century of Scholarship 1881 – 2004
A Century of Scholarship 1881 – 2004 Distinguished Scholars Reception Program (Date – TBD) Preface A HUNDRED YEARS OF SCHOLARSHIP AND RESEARCH AT MARQUETTE UNIVERSITY DISTINGUISHED SCHOLARS’ RECEPTION (DATE – TBD) At today’s reception we celebrate the outstanding accomplishments, excluding scholarship and creativity of Marquette remarkable records in many non-scholarly faculty, staff and alumni throughout the pursuits. It is noted that the careers of last century, and we eagerly anticipate the some alumni have been recognized more coming century. From what you read in fully over the years through various this booklet, who can imagine the scope Alumni Association awards. and importance of the work Marquette people will do during the coming hundred Given limitations, it is likely that some years? deserving individuals have been omitted and others have incomplete or incorrect In addition, this gathering honors the citations in the program listing. Apologies recipient of the Lawrence G. Haggerty are extended to anyone whose work has Faculty Award for Research Excellence, not been properly recognized; just as as well as recognizing the prestigious prize scholarship is a work always in progress, and the man for whom it is named. so is the compilation of a list like the one Presented for the first time in the year that follows. To improve the 2000, the award has come to be regarded completeness and correctness of the as a distinguishing mark of faculty listing, you are invited to submit to the excellence in research and scholarship. Graduate School the names of individuals and titles of works and honors that have This program lists much of the published been omitted or wrongly cited so that scholarship, grant awards, and major additions and changes can be made to the honors and distinctions among database. -

HAGAMOS MEMORIA La Evolución Del Sector Cultural En Guatemala, 1996-2016 ÍNDICE
HAGAMOS MEMORIA La evolución del sector cultural en Guatemala, 1996-2016 ÍNDICE EJERCITAR LA MEMORIA CULTURAL, Primera edición: Presentación 5 Ciudad de Guatemala Diciembre, 2017 HAGAMOS MEMORIA Introducción 9 Relatorías iniciales: José Fernández, Lisandro Guevara y Roxana Orantes Córdova EL ANDAMIAJE DE UNA GUERRA Época anterior: durante el conflicto armado interno 15 Versión final de los textos: Carmen Lucía Alvarado y Luis Méndez Salinas CREAREMOS, PESE A TODO Iconografía y elementos gráficos: Época de transición desde la firma de la paz, Julio Cúmez y renacimiento de los movimientos artísticos 29 Diseño y diagramación: Luis Méndez Salinas EL PENTAGRAMA DE NUESTRA MEMORIA Mesa de Música 41 Esta es una publicación conjunta del Centro Cultural de España en Guatemala, Fundación Paiz, Caja Lúdica, Fundación YAXS. UN PUENTE ENTRE LA COMUNIDAD Y SUS SÍMBOLOS y Ministerio de Cultura y Deportes, producida por Catafixia Mesa de Gestión Cultural 55 Editorial. Está protegida por una licencia Creative Commons Reco- nocimiento-No Comercial 4.0. Puede compartirse, distribuirse y co- municarse públicamente esta obra, siempre y cuando se reconozca VAMOS A CONTAR LO QUE VIMOS la fuente de manera adecuada y el material no se utilice para fines Mesa de Artes Visuales 67 comerciales. ¿CÓMO RECUPERAR EL CUERPO EN GUATEMALA? Mesa de Danza 81 CONOCERNOS A TRAVÉS DE UNA PANTALLA Mesa de cine 93 EL NECESARIO REGISTRO DE LO QUE SOMOS Mesa de Periodismo 107 EL ARTE QUE CAMINA ENTRE LA GENTE Mesa de Arte Urbano 121 UNA HISTORIA Y UNA HISTERIA QUE RECORREN LAS -

148759034.Pdf
LOS DESAPARECIDOS/ Horror Vacui GUATEMALA/2008 EMBAJADA de EspaÑA EN Guatemala Carmen Díez Orejas Embajadora Diego Nuño Consejero Cultural CENtro de FormaciÓN de la CooperaciÓN EspaÑola Mercedes Florez Directora Maria Luisa Aumesquet Responsable Formación David Ruiz López-Prisuelos Cristina Rodríguez Alonzo Rebeca Lozar López Espacioce! Miriam Legarreta Biblioce! Mariola Alvarez Laura Fernández Comunicación y Prensa Asesores Rosina Cazali Curadora Asociada Luisa Cabrera Coordinadora Componente Reflexivo Mercedes Blanco Coordinadora Componente Educativo Ximena Chapero Diseño y diagramación Valia Garzón. Consultores de Arte, S.A Cuidado de la edición Carlos Sebastian Luis Pedro Cabarrús Fotografías Alejo Crisostomo Video y Documentación © Los autores por sus textos © Los artistas por sus imágenes ISBN 978-99922-940-3-1 OrgaNIZacioNes DONANtes: ColaBoradores: ÍNDICE CARTA DE PRESENTacIÓN Mercedes Florez 7 COMPONENTE artístico LOS DEsaparECIDOS. Radiografía de una exposición / Rosina Cazali 11 HORROR VACUI VACIO NON PLENITUD. Primera muestra de performance, acciones e intervenciones artísticas / Rosina Cazali 15 A-1 53167 / Horror Vacui 16 STEFAN BENCHOAM / Nunca ha estado tan presente como cuando no está 17 BENVENUTO CHAVAJAY / Caso Francés 18 JORGE DE LEÓN / Recuerdo 19 MARÍA ADELA DÍAZ / Resistencia 20 AUDREY HOUBEN / Historia revelada 21 JESSICA KAIRÉ / Transicionalidades 22 DAVID KARMA PÉREZ / Forma truncada 23 JESSICA LAGUNAS / 120 minutos de silencio 24 JORGE LINARES / Variaciones de Horror Vacui 25 ENRIQUE LÓPEZ–CAMPANG / Sin título -

A Comparative Analysis of Punk in Spain and Mexico
Brigham Young University BYU ScholarsArchive Theses and Dissertations 2018-07-01 El futuro ya está aquí: A Comparative Analysis of Punk in Spain and Mexico Rex Richard Wilkins Brigham Young University Follow this and additional works at: https://scholarsarchive.byu.edu/etd Part of the Spanish and Portuguese Language and Literature Commons BYU ScholarsArchive Citation Wilkins, Rex Richard, "El futuro ya está aquí: A Comparative Analysis of Punk in Spain and Mexico" (2018). Theses and Dissertations. 6997. https://scholarsarchive.byu.edu/etd/6997 This Thesis is brought to you for free and open access by BYU ScholarsArchive. It has been accepted for inclusion in Theses and Dissertations by an authorized administrator of BYU ScholarsArchive. For more information, please contact [email protected], [email protected]. El futuro ya está aquí: A Comparative Analysis of Punk Culture in Spain and Mexico Rex Richard Wilkins A thesis submitted to the faculty of Brigham Young University in partial fulfillment of the requirements for the degree of Master of Arts Brian Price, Chair Erik Larson Alvin Sherman Department of Spanish and Portuguese Brigham Young University Copyright © 2018 Rex Richard Wilkins All Rights Reserved ABSTRACT El futuro ya está aquí: A Comparative Analysis of Punk Culture in Spain and Mexico Rex Richard Wilkins Department of Spanish and Portuguese, BYU Master of Arts This thesis examines the punk genre’s evolution into commercial mainstream music in Spain and Mexico. It looks at how this evolution altered both the aesthetic and gesture of the genre. This evolution can be seen by examining four bands that followed similar musical and commercial trajectories. -
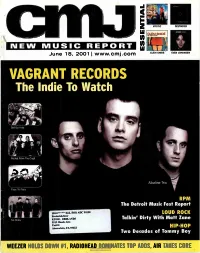
VAGRANT RECORDS the Lndie to Watch
VAGRANT RECORDS The lndie To Watch ,Get Up Kids Rocket From The Crypt Alkaline Trio Face To Face RPM The Detroit Music Fest Report 130.0******ALL FOR ADC 90198 LOUD ROCK Frederick Gier KUOR -REDLANDS Talkin' Dirty With Matt Zane No Motiv 5319 Honda Ave. Unit G Atascadero, CA 93422 HIP-HOP Two Decades of Tommy Boy WEEZER HOLDS DOWN el, RADIOHEAD DOMINATES TOP ADDS AIR TAKES CORE "Tommy's one of the most creative and versatile multi-instrumentalists of our generation." _BEN HARPER HINTO THE "Geggy Tah has a sleek, pointy groove, hitching the melody to one's psyche with the keen handiness of a hat pin." _BILLBOARD AT RADIO NOW RADIO: TYSON HALLER RETAIL: ON FEDDOR BILLY ZARRO 212-253-3154 310-288-2711 201-801-9267 www.virginrecords.com [email protected] [email protected] [email protected] 2001 VIrg. Records Amence. Inc. FEATURING "LAPDFINCE" PARENTAL ADVISORY IN SEARCH OF... EXPLICIT CONTENT %sr* Jeitetyr Co owe Eve« uuwEL. oles 6/18/2001 Issue 719 • Vol 68 • No 1 FEATURES 8 Vagrant Records: become one of the preeminent punk labels The Little Inclie That Could of the new decade. But thanks to a new dis- Boasting a roster that includes the likes of tribution deal with TVT, the label's sales are the Get Up Kids, Alkaline Trio and Rocket proving it to be the indie, punk or otherwise, From The Crypt, Vagrant Records has to watch in 2001. DEPARTMENTS 4 Essential 24 New World Our picks for the best new music of the week: An obit on Cameroonian music legend Mystic, Clem Snide, Destroyer, and Even Francis Bebay, the return of the Free Reed Johansen. -

Crinew Music Re Uoft
CRINew Music Re u oft SEPTEMBER 11, 2000 ISSUE 682 VOL. 63 NO. 12 WWW.CMJ.COM MUST HEAR Universal/NIP3.com Trial Begins With its lawsuit against MP3.com set to go inent on the case. to trial on August 28, Universal Music Group, On August 22, MP3.com settled with Sony the only major label that has not reached aset- Music Entertainment. This left the Seagram- tlement with MP3.com, appears to be dragging owned UMG as the last holdout of the major its feet in trying to reach a settlement, accord- labels to settle with the online company, which ing to MP3.com's lead attorney. currently has on hold its My.MP3.com service "Universal has adifferent agenda. They fig- — the source for all the litigation. ure that since they are the last to settle, they can Like earlier settlements with Warner Music squeeze us," said Michael Rhodes of the firm Group, BMG and EMI, the Sony settlement cov- Cooley Godward LLP, the lead attorney for ers copyright infringements, as well as alicens- MP3.com. Universal officials declined to corn- ing agreement allowing (Continued on page 10) SHELLAC Soundbreak.com, RIAA Agree Jurassic-5, Dilated LOS AMIGOS INVIWITI3LES- On Webcasting Royalty Peoples Go By Soundbreak.com made a fast break, leaving the pack behind and making an agreement with the Recording Word Of Mouth Industry Association of America (RIAA) on aroyalty rate for After hitting the number one a [digital compulsory Webcast license]. No details of the spot on the CMJ Radio 200 and actual rate were released. -

08/10/18 “Outside Lands Music & Arts Festival” the Weeknd
Artist TicketsTickets SoldSold Date Facility/Promoter Support Capacity Capacity GrossGross 08/10/18 “Outside Lands Music & Arts Festival” The Weeknd 201,477 $27,743,508 08/11-12 Golden Gate Park Florence + The Machine / Janet Jackson 67,159 San Francisco, CA Future / Beck / Odesza / Bon Iver 100% 3 shows Another Planet Entertainment / Superfly Presents DJ Snake / N*E*R*D 149.50 - 795.00 1 03/23/18 “Lollapalooza Brazil” Red Hot Chili Peppers / Pearl Jam 300,000 $23,384,475 03/24-25 Autodromo de Interlagos Arctic Monkeys / The Killers 100,000 Sao Paulo, BRAZIL Kendrick Lamar / Lenny Kravitz 100% Reals 3 shows T4F - Time For Fun Kings Of Leon / Chance The Rapper 297.50 - 2,000.00 (75,2985,298) 06/15/18 “Pinkpop” Pearl Jam / Foo Fighters 133,350 $19,567,672 06/16-17 Megaland Bruno Mars / A Perfect Circle 44,450 Landgraaf, NETHERLANDS The Offspring / The Script 100% Euro 3 shows Buro Pinkpop / Live Nation Snow Patrol / Editors / The Kooks 100.00 - 220.00 (16,3753,000) 09/21/18 “Life Is Beautiful Festival” The Weeknd / N*E*R*D 158,282 $19,528,148 09/22-23 Downtown Las Vegas Odesza / Death Cab For Cutie 52,761 Las Vegas, NV Justice / Florence + The Machine 100% 3 shows Another Planet Entertainment Chvrches / RL Grime / Travis Scott 135.00 - 2,495.00 4 06/22/18 “Southside Festival” Arctic Monkeys / The Prodigy 57,236 $11,255,727 06/23-24 Take Off Park The Offspring / Arcade Fire 60,000 Neuhausen ob Eck, GERMANY Billy Talent / The Kooks 95% Euro FKP Scorpio Konzertproduktionen Justice / Franz Ferdinand / NOFX 137.58 - 577.58 5(9,636,670) 08/03/18 -

Análisis Discursivo De Las Líricas Del Rock Argentino En La “Primavera Democrática” (1983 - 1986)
Si tienes voz, Análisis discursivo de las líricas del r oc k ar g entino tienes palabras Federico Rodríguez Lemos en la “primavera democr ática” Cristian Secul Giusti (1983 - 1986) Universidad Nacional de La Plata Facultad de Periodismo y Comunicación Social Licenciatura en Comunicación Social Tesis de Grado Si tienes voz, tienes palabras Análisis discursivo de las líricas del rock argentino en la “primavera democrática” (1983 - 1986) Autores: Federico Rodríguez Lemos Cristian Secul Giusti Directora: Susana Souilla Agosto, 2011 Facultad de Periodismo y Comunicación Social Universidad Nacional de La Plata La Plata, Agosto de 2011 Estimados miembros del Consejo Académico S / D Tengo el agrado de dirigirme a ustedes a los efectos de dejar constancia de que los alumnos Cristian Secul Giusti y Federico Rodríguez Lemos han concluido su tesis de licenciatura bajo mi dirección. En el trabajo “Si tienes voz, tienes palabras: análisis discursivo de las líricas del rock argentino en la “primavera democrática” (1983-1986)”, los tesistas han elaborado un cuidadoso análisis de letras de rock a partir de las herramientas teórico metodológicas del análisis del discurso y han consultado una extensa bibliografía no sólo de análisis discursivo sino también de las ciencias sociales en general. Considero pertinente destacar que durante todo el proceso de investigación y escritura de la tesis, los alumnos Secul Giusti y Rodríguez Lemos han demostrado responsabilidad, entusiasmo, curiosidad y una gran disposición para revisar su producción, corregir diversos aspectos formales y de contenido y proponer ideas creativas e interesantes. Estas cualidades y actitudes les han permitido experimentar un proceso de crecimiento en sus habilidades analíticas y reflexivas. -

Obama Le Dijo a Maduro Que Apoya El Diálogo Pacífico
PREMIO NACIONAL DE PERIODISMO 1982 / 1989 / 1990 3 5° El Tigre - Anaco, D o m i n go 1 2 de abril de 201 5 Año LV Edición 3.277 w w w.e l t i e m p o.co m .ve EL PERIÓDICO DEL PUEBLO ORIENTAL PV Justo Bs 30,00 Fecha de Marcaje 03/15 La tercerización vence Precios en clínicas aumenta Trueque contra la reventa en mayo, pero poco se sabe control de embarazos El intercambio, a través de las redes sociales, de productos escasos se ha vuelto una práctica cada vez más común como una medida cómo va ese proceso +10, 11 en hospital tigrense +8 para evitar la especulación de los bachaqueros +3 PREGUNTA DE LA SEMANA: ¿Cree que el sistema de compras por número de cédula ha frenado el “b a c h a q u e o”? Vote en w w w.eltiempo.com.ve POLÍTIC A GOBIERNO // ARREAZA: QUEREMOS BUENAS RELACIONES CON ESTADOS UNIDOS PORQUE ES UN SOCIO IM P O RTA N T E Sólo 10 de 28 toldas postularon candidatos para Obama le dijo a Maduro internas de MUD +5 que apoya el diálogo pacífico Los presidentes de EE UU y de Venezuela sostuvieron un breve encuentro cuando el líder norteamericano estaba retirándose de la Cumbre de las Américas en Panamá. La reunión fue confirmada por un vocero de la Casa Blanca y por el jefe de Estado bolivariano. Barack Obama le reiteró a su homólogo que el interés de su gobierno no es amenazar a Venezuela. Nicolás Maduro aseguró que fue una conversación seria, franca y hasta “co rd i a l ”, donde “nos dijimos las verdades”+14, 16 N AC I O N A L E S Usuarios llevarán al TSJ recorte y restricción en cupo de divisas +9 DEL DÍA En etiquetas está la clave para prevenir acc i d e nt e s +20, 21 CINE A Sarah Jessica el “s exo” en la ciudad le brindó fama Como “h i s t ó r i c a”calificó el presidente de Estados Unidos, Barack Obama, la primera reunión que sostuvo con el mandatario cubano Raúl Castro. -

Piedras Color
eSTELAR Domingo 19 de Febrero de 2006 EXPRESO 7D FOBIA, SIN MIEDO A LOS STONES Piedras color El grupo mexicano El hecho es abrirá el concierto de “que nos eligieron los Rolling Stones el entre varias próximo 26 de febrero bandas, y nos en la Ciudad de México toca llevar en alto el prestigio GUADALAJARA.- Nada más de tocar el tema, el gesto les del rock nacional cambia. Para los integrantes del y decir: ‘Hay grupo Fobia, abrir el concierto de los Rolling Stones en México bandas de el próximo 26 de febrero en elROSA Foro Sol es un sueño, pero más calidad que le que nada “un honor”, asegura pueden abrir Iñaki, tecladista de la banda, con una sonrisa que casi le des- a bandas a la borda el rostro. banda más A su lado, Cha se tira del ca- bello y expresa: “Es que son ‘sus antigua y más satánicas majestades”. Iñaki acepta que esta oportu- antigua del nidad es de esos sueños que no planeta’” se esperan cumplir y se enfren- tan sin miedo. Fobia “¿Pero sí lo sueñas?”, le in- Grupo de rock quiere el bajista. Iñaki recuerda que desde los 14 años que se inició en la música, pensaba conocer a “los Stones”, pero no se imaginaba VENUS poder tocar en el mismo lugar. “No creí, incluso, que por generación me fuera a tocar. Lo increíble es que estén tan bien a su edad, con tanta energía, más que nosotros; con tanta energía como para seguir girando por el mundo”. (SUN)1 5NUEVO DISCO 9INTEGRANTES AÑOS JUNTOS ¿Cómo se dice? ¿Cómo se dice disparo en árabe? José Luis Ramírez / Agencia Reforma / EXPRESO Reforma Agencia / Luis Ramírez José alla va la bala Los integrantes de Fobia serán teloneros de “Las piedras rodantes” (The Rolling Stones). -

Re-Interpreting Mexican Rock Music: Contemporary Youth
RE-INTERPRETING MEXICAN ROCK MUSIC: CONTEMPORARY YOUTH, POLITICS, AND THE MEXICAN STATE by MAGDELANA RED B.A., University of San Francisco, 2000 M.A., University of Texas at Austin, 2003 A thesis submitted to the Faculty of the Graduate School of the University of Colorado in partial fulfillment of the requirement for the degree of Doctor of Philosophy School of Journalism and Mass Communication 2012 This thesis entitled: Re-Interpreting Mexican Rock Music: Contemporary Youth, Politics, and the Mexican State written by Magdelana Red has been approved for the School of Journalism and Mass Communication _________________________________________ Dr. Robert Trager, Chair _________________________________________ Dr. Shu-Ling Berggreen _________________________________________ Dr. Robert Buffington _________________________________________ Dr. Isaac Reed _________________________________________ Dr. Nabil Echchaibi Date ____________________ The final copy of this thesis has been examined by the signatories, and we find that both the content and the form meet acceptable presentation standards of scholarly work in the above mentioned discipline. IRB protocol # 0410.26 Copyright 2012, Magdelana Red Red, Magdelana Mae (Ph.D., Communication) Re-Interpreting Mexican Rock Music: Contemporary Youth, Politics, and the Mexican State Thesis directed by Professor Robert Trager This dissertation elaborates a theoretical intervention challenging accepted interpretations of the role of rock music in youth political expression and identity formation during the period following the Mexican government’s apertura, or opening, from the 1980s through the 2000s, a period that followed decades of censorship and tight government control of youth expression, popular culture, and national identity. In spite of the fact that youth under the age of twenty-four make up approximately forty-five percent of Mexico’s population, young people and their engagement with and creation of popular culture have been severely understudied. -

****10 Tag'' a BILLBOARD SPOTLIGHT: PAGE 51
$5.95 (U.S.), $6.95 (CAN.), £4.95 (U.K.), Y2,500 (JAPAN) Z04£-L0906 V3 H3V39 91101 V t 3AV W13 04LE 0911 9Zi Z (,jnjrjrjnntjjjnjnjjnjnrjnrjjrjnjnrjjnjtjj005Z£Ó33TTÓOA1tJOW 959 0919 tZ00W34L2339L0906t 906 1I9I0-£ ******* TA3J11X9t THE INTERNATIONAL NEWSWIEEKLY OF MUSIC, VIDEO, AND HOME ENTERTAINMENT REACHING 110 COUNTRIES NOVEMBER 21, 1998 THERE'S A NEW SOUND FOR THE SEASON... "Unigram' Takes Shape, But Details Unresolved V:Awn/.l-CJGf/Ief,;/I2 A Billboard staff report. The broad strokes may have been The switch has not been finalized, through" in December (Billboard, painted, but none of the lines has says a senior PolyGram executive, Nov 14). l%')Gr2P/.lIeß'i NEW YORK -While the proposed been filled in yet, says one executive but "it has essentially been agreed." "No final decisions have been involved in the consolidation process. Paul McGuinness of Dublin -based made," says Universal Music "Strikingly original." master plan to consolidate PolyGram Management says, "We do spokesman Bob Bernstein, who -- People and the Universal Music Group In fact, some of the senior label exec- Principle (UMG) into one company has been utives who are upset by how not know as of now where declines further comment. "...the best selling album of the season." revealed via press reports in advance their new roles are being certain players are going to Rank and file employees, who have --NT Times of official word, the thousands of defined in the consolidated end up. This is by no means been anxious since the deal was first details needed to make the scheme company are said to be lob- RSAL done and dusted." announced in mid -May to see how the "Amazing...powerful..." work are still being sorted out, accord- bying to overturn some of The relationship between two companies will be fitted togeth- --Scott Shannon/WPLJ ing to executives at both companies.