Analytical Studies on the Kavain Metabolism in Human Specimen and Liver Cell Lines
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Kava (Piper Methysticum) and Its Methysticin Constituents Protect Brain Tissue Against Ischemic Damage in Rodents
5 Refs: Arletti R et al, Stimulating property of Turnera diffusa and Pfaffia paniculata extracts on the sexual-behavior of male rats. Psychopharmacology 143(1), 15-19, 1999. Berger F, Handbuch der drogenkunde . Vol 2, Maudrich, Wien, 1950. Martinez M, Les plantas medicinales de Mexico . Cuarta Edicion Botas Mexico , p119, 1959. Tyler VE et al, Pharmacognosy , 9 th edition, Lea & Febiger, Philadelphia, 1988. KAVA ( Piper methysticum ) - A REVIEW The Kava plant (Piper methysticum) is a robust, well-branching and erect perennial shrub belonging to the pepper family (Piperaceae). The botanical origin remains unknown, although it is likely that early Polynesian explorers brought the plant with them from island to island. Numerous varieties of Kava exist, and today it is widely cultivated in several Pacific Island countries both for local use as well as the rapidly growing demand for pharmaceutical preparations. The dried rhizomes (roots) are normally used. The first description to the western world of the ceremonial use of an intoxicating beverage prepared from Kava was made by Captain James Cook following his Pacific voyage in 1768. The drink, prepared as an infusion in an elaborate manner after first chewing the root, is consumed on formal occasions or meetings of village elders and chiefs, as well as in reconciling with enemies and on a more social basis. It remains an important social custom in many Pacific Island countries today. Most of the islands of the Pacific possessed Kava prior to European contact, particularly those encompassed by Polynesia, Melanesia and Micronesia. After drinking the Kava beverage a pleasantly relaxed and sociable state develops, after which a deep and restful sleep occurs. -

Alternative Treatments for Depression and Anxiety
2019 PCB Conference: Strickland Benzodiazepines (BZDs), Herbal and Alternative Treatments for Anxiety & Depression BZD Learning Objectives • List at least three uses for benzodiazepines • Discuss at least two risk factors associated with benzodiazepine prescriptions Craig Strickland, PhD, Owner Biobehavioral Education and Consultation https://sites.google.com/site/bioedcon 1 2 BZD Pharmacokinetics Clinical Uses of BZDs Generic Name Trade Name Rapidity ½ Life Dose (mg) • Treat a variety of anxiety disorders alprazolam Xanax Intermediate Short 0.75-4 • Hypnotics • Muscle relaxants chlordiaze- Librium Intermediate Long 15-100 poxide • To produce anterograde amnesia clonazepam Klonopin Intermediate Long 0.5-4 • Alcohol & other CNS depressant withdrawal • Anti-convulsant therapy diazepam Valium Rapid Long 4-40 triazolam Halcion Intermediate Very short 0.125-0.5 temazepam Restoril Short Short 7.5-30 3 4 1 2019 PCB Conference: Strickland Issues with BZDs Herbal Medication and Alternative Therapies Used in the Treatment of Depression and Anxiety • Addictive potential • Confusion between “anti-anxiety” effects and the “warm-fuzzy) • Large dose ranges • Comparison of BZDs with medications like Buspar, etc. • They work, they work well and they work quickly 5 6 Alternative Tx. Learning Objectives Background Information on herbals: Natural does not necessarily mean “safe” • List several amino acid treatments for depression • Side-effects and adverse reactions • List at least three of the most common herbal – Herbal medications are “drugs” although -

Could Mycolactone Inspire New Potent Analgesics? Perspectives and Pitfalls
toxins Review Could Mycolactone Inspire New Potent Analgesics? Perspectives and Pitfalls 1 2 3, 4, , Marie-Line Reynaert , Denis Dupoiron , Edouard Yeramian y, Laurent Marsollier * y and 1, , Priscille Brodin * y 1 France Univ. Lille, CNRS, Inserm, CHU Lille, Institut Pasteur de Lille, U1019-UMR8204-CIIL-Center for Infection and Immunity of Lille, F-59000 Lille, France 2 Institut de Cancérologie de l’Ouest Paul Papin, 15 rue André Boquel-49055 Angers, France 3 Unité de Microbiologie Structurale, Institut Pasteur, CNRS, Univ. Paris, F-75015 Paris, France 4 Equipe ATIP AVENIR, CRCINA, INSERM, Univ. Nantes, Univ. Angers, 4 rue Larrey, F-49933 Angers, France * Correspondence: [email protected] (L.M.); [email protected] (P.B.) These three authors contribute equally to this work. y Received: 29 June 2019; Accepted: 3 September 2019; Published: 4 September 2019 Abstract: Pain currently represents the most common symptom for which medical attention is sought by patients. The available treatments have limited effectiveness and significant side-effects. In addition, most often, the duration of analgesia is short. Today, the handling of pain remains a major challenge. One promising alternative for the discovery of novel potent analgesics is to take inspiration from Mother Nature; in this context, the detailed investigation of the intriguing analgesia implemented in Buruli ulcer, an infectious disease caused by the bacterium Mycobacterium ulcerans and characterized by painless ulcerative lesions, seems particularly promising. More precisely, in this disease, the painless skin ulcers are caused by mycolactone, a polyketide lactone exotoxin. In fact, mycolactone exerts a wide range of effects on the host, besides being responsible for analgesia, as it has been shown notably to modulate the immune response or to provoke apoptosis. -

Is Alcohol Use Related to High Cholesterol in Premenopausal
Research iMedPub Journals Journal of Preventive Medicine 2018 http://www.imedpub.com/ Vol.3 No.1:3 ISSN 2572-5483 DOI: 10.21767/2572-5483.100024 Is Alcohol Use Related To High Cholesterol in Premenopausal Women Aged 40-51 Years Old? Sydnee Homeyer, Jessica L Hartos*, Holli Lueg, Jessica Moore and Patricia Stafford Department of Physician Assistant Studies, University of North Texas Health Science Center, USA *Corresponding author: Jessica L. Hartos, Department of Physician Assistant Studies, University of North Texas Health Science Center, USA, Tel: 817-735-2454; Fax: 817-735-2529; E-mail: [email protected] Received date: November 13, 2017; Accepted date: January 8, 2018; Publication date: January 15, 2018 Citation: Homeyer S, Hartos JL, Lueg H, Moore J, Stafford P, et al. (2018) Is Alcohol Use Related To High Cholesterol In Premenopausal Women Aged 40-51 Years Old? J Prev Med Vol.3 No.3: 3. Copyright: © 2018 Homeyer S, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution and reproduction in any medium, provided the original author and source are credited. Introduction Abstract Increased serum cholesterol levels is a major risk factor for coronary heart disease (CHD) [1], and over seventy-one million Purpose: Alcohol use and cholesterol are related in men and American adults have high cholesterol (27%) [2,3]. In American postmenopausal women but relations between alcohol use women, cholesterol levels have been shown to increase with and cholesterol are unclear for premenopausal women. The age, and nearly 1 in 2 American women has high or borderline purpose of this study was to determine whether alcohol use was related to cholesterol in women aged 40-51 years old. -

E the Effect of Topiramate on Weight Loss in Patients with Type 2 Diabetes
E The effect of topiramate on weight loss in patients with type 2 diabetes RTICL Sedighe Moradi, Scott Reza Jafarian Kerman, Mina Mollabashi A Institute of Endocrinology and Metabolism (Hemmat Campus), Firoozgar Hospital, Tehran University of Medical Sciences, Tehran, Iran Background: Obesity has been associated with several co‑morbidities such as diabetes and increased mortality. In general, the use of medication promotes only a modest weight loss in the range of 2 to 10 kg, usually most effective during the first 6 months of therapy; however, studies have shown positive effects on other risk factors such as blood pressure and serum glucose levels, but there are fewer studies in patients with diabetes. The aim of this study was to assess the effect of topiramate on weight reduction patients with type 2 diabetes. Materials and Methods: This was a 32‑week randomized clinical trial study of 69 subjects during 2008‑2010. RIGINAL Patients, in two treatment groups were given topiramate (39 patients) and Placebo (30 patients) and were subjected to participation in a non‑pharmacologic lifestyle intervention program; which were randomly allocated in our two groups. The percentage change in body O weight and Body Mass Index (BMI) at the end of the study was the primary efficacy endpoint and secondary indicators were changes in blood pressure (BP), proportion of subjects who achieved 5% or 10% weight loss, changes in lipid profile (total cholesterol, low‑density lipoprotein cholesterol, high‑density lipoprotein cholesterol, triglycerides); and changes in glycosylated hemoglobin (HgA1c). Paired samples and independent samples t‑test was used for statistical analysis. -

Central Valley Toxicology Drug List
Chloroform ~F~ Lithium ~A~ Chlorpheniramine Loratadine Famotidine Acebutolol Chlorpromazine Lorazepam Fenoprofen Acetaminophen Cimetidine Loxapine Fentanyl Acetone Citalopram LSD (Lysergide) Fexofenadine 6-mono- Clomipramine acetylmorphine Flecainide ~M~ Clonazepam a-Hydroxyalprazolam Fluconazole Maprotiline Clonidine a-Hydroxytriazolam Flunitrazepam MDA Clorazepate Albuterol Fluoxetine MDMA Clozapine Alprazolam Fluphenazine Medazepam Cocaethylene Amantadine Flurazepam Meperidine Cocaine 7-Aminoflunitrazepam Fluvoxamine Mephobarbital Codeine Amiodarone Fosinopril Meprobamate Conine Amitriptyline Furosemide Mesoridazine Cotinine Amlodipine Methadone Cyanide ~G~ Amobarbital Methanol Cyclobenzaprine Gabapentin Amoxapine d-Methamphetamine Cyclosporine GHB d-Amphetamine l-Methamphetamine Glutethamide l-Amphetamine ~D~ Methapyrilene Guaifenesin Aprobarbital Demoxepam Methaqualone Atenolol Desalkylfurazepam ~H~ Methocarbamol Atropine Desipramine Halazepam Methylphenidate ~B~ Desmethyldoxepin Haloperidol Methyprylon Dextromethoraphan Heroin Metoclopramide Baclofen Diazepam Hexobarbital Metoprolol Barbital Digoxin Hydrocodone Mexiletine Benzoylecgonine Dihydrocodein Hydromorphone Midazolam Benzphetamine Dihydrokevain Hydroxychloroquine Mirtazapine Benztropine Diltiazem Hydroxyzine Morphine (Total/Free) Brodificoum Dimenhydrinate Bromazepam ~N~ Diphenhydramine ~I~ Bupivacaine Nafcillin Disopyramide Ibuprofen Buprenorphine Naloxone Doxapram Imipramine Bupropion Naltrexone Doxazosin Indomethacin Buspirone NAPA Doxepin Isoniazid Butabarbital Naproxen -

Diazepam and Kava Combination Article
Journal of Advanced Research (2014) 5, 587–594 Cairo University Journal of Advanced Research ORIGINAL ARTICLE Enhanced efficacy and reduced side effects of diazepam by kava combination Rasha A. Tawfiq a, Noha N. Nassar b,*, Wafaa I. El-Eraky c, Ezzeldein S. El-Denshary b a Egyptian Patent Office, Academy of Scientific Research and Technology, 101 Kasr El-Eini St., Cairo, Egypt b Department of Pharmacology and Toxicology, Faculty of Pharmacy, Cairo University, Kasr El-Eini St., Cairo, Egypt c Department of Pharmacology, National Research Center, El-Tahrir St., Giza, Egypt ARTICLE INFO ABSTRACT Article history: The long term use of antiepileptic drugs possesses many unwanted effects; thus, new safe com- Received 2 April 2013 binations are urgently mandated. Hence, the present study aimed to investigate the anticonvul- Received in revised form 18 July 2013 sant effect of kava alone or in combination with a synthetic anticonvulsant drug, diazepam Accepted 15 August 2013 (DZ). To this end, female Wistar rats were divided into two subsets, each comprising 6 groups Available online 22 August 2013 as follows: group (i) received 1% Tween 80 p.o. and served as control, while groups (ii) and (iii) received kava at two dose levels (100 and 200 mg/kg, p.o.). The remaining three groups received Keywords: (iv) DZ alone (10 mg/kg p.o.) or kava in combination with DZ (v) (5 mg/kg, p.o.) or (vi) (10 mg/ Kava kg, p.o.). Results of the present study revealed that kava increased the maximal electroshock Diazepam seizure threshold (MEST) and enhanced the anticonvulsant effect of diazepam following both Anticonvulsant acute and chronic treatment. -

CAS Number Index
2334 CAS Number Index CAS # Page Name CAS # Page Name CAS # Page Name 50-00-0 905 Formaldehyde 56-81-5 967 Glycerol 61-90-5 1135 Leucine 50-02-2 596 Dexamethasone 56-85-9 963 Glutamine 62-44-2 1640 Phenacetin 50-06-6 1654 Phenobarbital 57-00-1 514 Creatine 62-46-4 1166 α-Lipoic acid 50-11-3 1288 Metharbital 57-22-7 2229 Vincristine 62-53-3 131 Aniline 50-12-4 1245 Mephenytoin 57-24-9 1950 Strychnine 62-73-7 626 Dichlorvos 50-23-7 1017 Hydrocortisone 57-27-2 1428 Morphine 63-05-8 127 Androstenedione 50-24-8 1739 Prednisolone 57-41-0 1672 Phenytoin 63-25-2 335 Carbaryl 50-29-3 569 DDT 57-42-1 1239 Meperidine 63-75-2 142 Arecoline 50-33-9 1666 Phenylbutazone 57-43-2 108 Amobarbital 64-04-0 1648 Phenethylamine 50-34-0 1770 Propantheline bromide 57-44-3 191 Barbital 64-13-1 1308 p-Methoxyamphetamine 50-35-1 2054 Thalidomide 57-47-6 1683 Physostigmine 64-17-5 784 Ethanol 50-36-2 497 Cocaine 57-53-4 1249 Meprobamate 64-18-6 909 Formic acid 50-37-3 1197 Lysergic acid diethylamide 57-55-6 1782 Propylene glycol 64-77-7 2104 Tolbutamide 50-44-2 1253 6-Mercaptopurine 57-66-9 1751 Probenecid 64-86-8 506 Colchicine 50-47-5 589 Desipramine 57-74-9 398 Chlordane 65-23-6 1802 Pyridoxine 50-48-6 103 Amitriptyline 57-92-1 1947 Streptomycin 65-29-2 931 Gallamine 50-49-7 1053 Imipramine 57-94-3 2179 Tubocurarine chloride 65-45-2 1888 Salicylamide 50-52-2 2071 Thioridazine 57-96-5 1966 Sulfinpyrazone 65-49-6 98 p-Aminosalicylic acid 50-53-3 426 Chlorpromazine 58-00-4 138 Apomorphine 66-76-2 632 Dicumarol 50-55-5 1841 Reserpine 58-05-9 1136 Leucovorin 66-79-5 -
Kava - the Unfolding Story: Report on a Work-In-Progress
Article Kava - the unfolding story: Report on a work-in-progress. Denham, Alison, McIntyre, Michael and Whitehouse, Jule Available at http://clok.uclan.ac.uk/9455/ Denham, Alison, McIntyre, Michael and Whitehouse, Jule Kava - the unfolding story: Report on a work-in-progress. Journal of Alternative and Complementary Medicine, 8 (3). pp. 237-263. It is advisable to refer to the publisher’s version if you intend to cite from the work. For more information about UCLan’s research in this area go to http://www.uclan.ac.uk/researchgroups/ and search for <name of research Group>. For information about Research generally at UCLan please go to http://www.uclan.ac.uk/research/ All outputs in CLoK are protected by Intellectual Property Rights law, including Copyright law. Copyright, IPR and Moral Rights for the works on this site are retained by the individual authors and/or other copyright owners. Terms and conditions for use of this material are defined in the policies page. CLoK Central Lancashire online Knowledge www.clok.uclan.ac.uk THE JOURNAL OF ALTERNATIVE AND COMPLEMENTARY MEDICINE Volume 8, Number 3, 2002, pp. 237–263 © Mary Ann Liebert, Inc. SPECIAL REPORT Kava—the Unfolding Story: Report on a Work-in-Progress ALISON DENHAM, B.A. (Soc.), M.N.I.M.H., 1 MICHAEL McINTYRE, M.A., F.N.I.M.H., F.R.C.H.M., M.B.Ac.C., 2 and JULIE WHITEHOUSE, Ph.D., M.N.I.M.H. 3 ABSTRACT This paper, originated as a submission (now updated) to the U.K. Medicines Control Agency and Committee of Safety of Medicines (CSM) on January 11, 2002, in response to a report circu- lated by the German Federal Institute for Drugs and Medical Products (German initials are BfArM), a compilation of which is summarized in Appendix 2. -

Letters to the Editor
Letters to the Editor Internet Pharmacy Prescription complete the medication database. Of course, patients can abuse and Phentermine Overdose any medications, so collaboration between pharmacies and physicians is essential to minimize this risk. Sir: The Internet is now widely used by patients for both Dr. Takeshita reports no financial or other relationship relevant to the health information and prescription services. Yet, a MEDLINE subject matter of this letter. search in January 2002 using the phrase “Internet pharmacy” showed a total of 99 articles; nearly all were geared toward REFERENCES health care management or the general public. There are only a few published reports of bad outcome resulting from medical 1 1. Crocco AG, Villasis-Keever M, Jadad AR. Analysis of cases of information obtained from the Internet. The U.S. Food and harm associated with use of health information on the Internet. Drug Administration noted 326 Internet sites selling pharma- JAMA 2002;287:2867–2871 ceutical products.2 The exact numbers are difficult to quantify 2. Henney JE. Cyberpharmacies and the role of the US Food and Drug as Web sites are constantly changing. I report a case of overdose Administration. J Med Internet Res 2001;3:E3 with phentermine that was obtained through an Internet 3. Gardin JM, Schumacher D, Constantine G, et al. Valvular abnormali- pharmacy. ties and cardiovascular status following exposure to dexfenfluramine or phentermine/fenfluramine. JAMA 2000;283:1703–1709 4. Koury E, Stone CK, Stapczynski JS, et al. Sympathetic overactivity Case report. Ms. A, a 20-year-old woman with a prior from fenfluramine-phentermine overdose. -
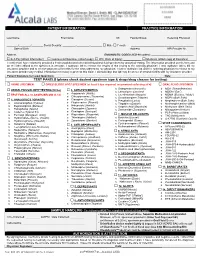
Please Check Desired Specimen Type & Drugs/Drug Classes for Testing
PATIENT INFORMATION PRACTICE INFORMATION ____________________________________ _____________________________________ _______ ________________________ __________________ Last Name First Name MI Facility/Group Referring Physician ________/________/________ Social Security: _________-_________-________ ☐ Male ☐ Female ___________________________________________ Date of Birth Address NPI Provider Nr. __________________________________________________________________ Address DIAGNOSTIC CODES (ICD-10 codes): _____________________________ ☐ Self-Pay (attach Information) ☐ Commercial Insurance (attach copy) ☐ W/C (Date of Injury): ____________ ☐ Medicare (attach copy of Insurance) I certify that I have voluntarily provided a fresh unadulterated urine/dried blood/oral fluid specimen for analytical testing. The information provided on this form and on the label affixed to the specimen is accurate. I authorize lab to release the results of this testing to the ordering physician. I also authorize lab to bill my insurance provider and to receive payment of benefits for the tests ordered by my physician. I further authorize lab and the ordering physician to release to my insurance provider any medical information necessary to process this claim. I acknowledge that lab may be an out-of-network facility with my insurance provider. Patient Signature (or Legal Guardian): ___________________________________________________________________________ Date: _______________ TEST PANELS (please check desired specimen type & drugs/drug classes for testing): ☐ URINE -

Kava Kava Extract Is Available from Ashland Chemical Co., Mini Star International, Inc., and QBI (Quality Botanical Ingredients, Inc.)
SUMMARY OF DATA FOR CHEMICAL SELECTION Kava Kava 9000-38-8; 84696-40-2 November 1998 TABLE OF CONTENTS Basis for Nomination Chemical Identification Production Information Use Pattern Human Exposure Regulatory Status Evidence for Possible Carcinogenic Activity Human Data Animal Data Metabolism Other Biological Effects Structure-Activity Relationships References BASIS OF NOMINATION TO THE CSWG Kava kava is brought to the attention of the CSWG because it is a rapidly growing, highly used dietary supplement introduced into the mainstream U.S. market relatively recently. Through this use, millions of consumers using antianxiety preparations are potentially exposed to kava kava. A traditional beverage of various Pacific Basin countries, kava clearly has psychoactive properties. The effects of its long-term consumption have not been documented adequately; preliminary studies suggest possibly serious organ system effects. The potential carcinogenicity of kava and its principal constituents are unknown. INPUT FROM GOVERNMENT AGENCIES/INDUSTRY The U.S. Pharmacopeia is in the process of reviewing kava kava. No decision on preparation of a monograph has been made. SELECTION STATUS ACTION BY CSWG: 12/14/98 Studies requested: - Toxicological evaluation, to include studies of reproductive toxicity and neurotoxicity - Genotoxicity Priority: High Rationale/Remarks: - Significant human exposure - Leading dietary supplement with rapidly growing use - Concern that kava has been promoted as a substitute for ritilin in children - Test extract standardized to 30 percent kavalactones - NCI is conducting studies in Salmonella typhimurium CHEMICAL IDENTIFICATION CAS Registry Number: 9000-38-8 Kava-kava resin (8CI) Chemical Abstract Service Name: 84696-40-2 CAS Registry Number: Pepper (Piper), P. methysticum, ext. Chemical Abstract Service Name: Extract of kava; kava extract; Piper Synonyms and Trade Names: methisticum extract Description: The tropical shrub Piper methysticum is widely cultivated in the South Pacific.