Kava - the Unfolding Story: Report on a Work-In-Progress
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Anti-Inflammatory Activity of Compounds from Kaempferia Marginata Rhizomes
Songklanakarin J. Sci. Technol. 39 (1), 91-99, Jan. - Feb. 2017 http://www.sjst.psu.ac.th Original Article Anti-inflammatory activity of compounds from Kaempferia marginata rhizomes Kanidta Kaewkroek1, Chatchai Wattanapiromsakul1, 2, Hisashi Matsuda3, Seikou Nakamura3, and Supinya Tewtrakul1, 2* 1 Department of Pharmacognosy and Pharmaceutical Botany, Faculty of Pharmaceutical Sciences, Prince of Songkla University, Hat Yai, Songkhla, 90112 Thailand 2 Excellent Research Laboratory, Phytomedicine and Phamaceutical Biotechnology Excellence Center, Faculty of Pharmaceutical Sciences, Prince of Songkla University, Hat Yai, Songkhla, 90112 Thailand 3 Kyoto Pharmaceutical University, Misasagi, Yamashina-ku, Kyoto, 607-8412 Japan Received: 12 January 2016; Revised: 12 April 2016; Accepted: 19 April 2016 Abstract Two new pimarane diterpenes were obtained from Kaempferia marginata rhizomes, which are 1-acetoxysandara- copimaradien-2-one (1) and 1-acetoxysandaracopimaradiene (4), along with seven known compounds from the hexane and chloroform fractions including two pimarane-type diterpenes [marginatol (5), sandaracopimaradiene (8)], one kavalactone [desmethoxyyangonin (3)], three steroids [sitosterol--D-glucoside (2), the mixture of stigmasterol and -sitosterol (6 + 7)] and one diarylheptanoid [bisdemethoxycurcumin (9)]. Compounds 3 and 9 exhibited potent effect against NO production with IC50 of 10.1 and 6.8 µM, respectively. Compound 3 inhibited iNOS mRNA expression in a dose-dependent manner, while 9 suppressed both of iNOS and COX-2 genes. Moreover, compounds 2, 3, 6 + 7 and 9 were isolated for the first time from K. marginata. These results revealed that diterpenes, diarylheptanoid and kavalactone are components of K. marginata that afford anti-inflammatory effect through a mechanism involving a decrease in inflammatory mediators. Keywords: Kaempferia marginata, diterpenes, diarylheptanoid, kavalactone, anti-inflammatory activity 1. -

Herbal Insomnia Medications That Target Gabaergic Systems: a Review of the Psychopharmacological Evidence
Send Orders for Reprints to [email protected] Current Neuropharmacology, 2014, 12, 000-000 1 Herbal Insomnia Medications that Target GABAergic Systems: A Review of the Psychopharmacological Evidence Yuan Shia, Jing-Wen Donga, Jiang-He Zhaob, Li-Na Tanga and Jian-Jun Zhanga,* aState Key Laboratory of Bioactive Substance and Function of Natural Medicines, Institute of Materia Medica, Chinese Academy of Medical Sciences and Peking Union Medical College, Beijing, P.R. China; bDepartment of Pharmacology, School of Marine, Shandong University, Weihai, P.R. China Abstract: Insomnia is a common sleep disorder which is prevalent in women and the elderly. Current insomnia drugs mainly target the -aminobutyric acid (GABA) receptor, melatonin receptor, histamine receptor, orexin, and serotonin receptor. GABAA receptor modulators are ordinarily used to manage insomnia, but they are known to affect sleep maintenance, including residual effects, tolerance, and dependence. In an effort to discover new drugs that relieve insomnia symptoms while avoiding side effects, numerous studies focusing on the neurotransmitter GABA and herbal medicines have been conducted. Traditional herbal medicines, such as Piper methysticum and the seed of Zizyphus jujuba Mill var. spinosa, have been widely reported to improve sleep and other mental disorders. These herbal medicines have been applied for many years in folk medicine, and extracts of these medicines have been used to study their pharmacological actions and mechanisms. Although effective and relatively safe, natural plant products have some side effects, such as hepatotoxicity and skin reactions effects of Piper methysticum. In addition, there are insufficient evidences to certify the safety of most traditional herbal medicine. In this review, we provide an overview of the current state of knowledge regarding a variety of natural plant products that are commonly used to treat insomnia to facilitate future studies. -

Central Valley Toxicology Drug List
Chloroform ~F~ Lithium ~A~ Chlorpheniramine Loratadine Famotidine Acebutolol Chlorpromazine Lorazepam Fenoprofen Acetaminophen Cimetidine Loxapine Fentanyl Acetone Citalopram LSD (Lysergide) Fexofenadine 6-mono- Clomipramine acetylmorphine Flecainide ~M~ Clonazepam a-Hydroxyalprazolam Fluconazole Maprotiline Clonidine a-Hydroxytriazolam Flunitrazepam MDA Clorazepate Albuterol Fluoxetine MDMA Clozapine Alprazolam Fluphenazine Medazepam Cocaethylene Amantadine Flurazepam Meperidine Cocaine 7-Aminoflunitrazepam Fluvoxamine Mephobarbital Codeine Amiodarone Fosinopril Meprobamate Conine Amitriptyline Furosemide Mesoridazine Cotinine Amlodipine Methadone Cyanide ~G~ Amobarbital Methanol Cyclobenzaprine Gabapentin Amoxapine d-Methamphetamine Cyclosporine GHB d-Amphetamine l-Methamphetamine Glutethamide l-Amphetamine ~D~ Methapyrilene Guaifenesin Aprobarbital Demoxepam Methaqualone Atenolol Desalkylfurazepam ~H~ Methocarbamol Atropine Desipramine Halazepam Methylphenidate ~B~ Desmethyldoxepin Haloperidol Methyprylon Dextromethoraphan Heroin Metoclopramide Baclofen Diazepam Hexobarbital Metoprolol Barbital Digoxin Hydrocodone Mexiletine Benzoylecgonine Dihydrocodein Hydromorphone Midazolam Benzphetamine Dihydrokevain Hydroxychloroquine Mirtazapine Benztropine Diltiazem Hydroxyzine Morphine (Total/Free) Brodificoum Dimenhydrinate Bromazepam ~N~ Diphenhydramine ~I~ Bupivacaine Nafcillin Disopyramide Ibuprofen Buprenorphine Naloxone Doxapram Imipramine Bupropion Naltrexone Doxazosin Indomethacin Buspirone NAPA Doxepin Isoniazid Butabarbital Naproxen -

(12) Patent Application Publication (10) Pub. No.: US 2010/0311593 A1 Fischer Et Al
US 20100311593A1 (19) United States (12) Patent Application Publication (10) Pub. No.: US 2010/0311593 A1 Fischer et al. (43) Pub. Date: Dec. 9, 2010 (54) HALOALKYLMETHYLENEOXYPHENYL- AOIPI3/00 (2006.01) SUBSTITUTED KETOENOLS C07D 207/00 (2006.01) C07D 305/12 (2006.01) (75) Inventors: Reiner Fischer, Monheim (DE): CD7C 49/00 (2006.01) Thomas Bretschneider, Lohmar C07D 23/00 (2006.01) (DE); Stefan Lehr, Liederbach C07C 229/00 (2006.01) (DE); Eva-Maria Franken, Lyon C07C 69/76 (2006.01) (FR): Olga Malsam, Rosrath (DE); CD7C 24I/00 (2006.01) Arnd Voerste, Koln (DE); Ulrich CD7C 63/04 (2006.01) Görgens, Ratingen (DE); Jan (52) U.S. Cl. ......... 504/219;564/170; 514/622:504/336; Dittgen, Frankfurt (DE); Dieter Feucht, Eschborn (DE); Isolde 504/236; 514/248; 544/235; 540/545; 514/211.08; Hauser-Hahn, Leverkusen (DE); 548/544; 549/319; 568/379: 548/366.4; 560/37; Christopher Hugh Rosinger, 560/76; 560/105:564/149; 562/493 Hofheim (DE); Alfred Angermann, Kriftel (DE) (57) ABSTRACT The invention relates to novel compounds of the formula (I), Correspondence Address: STERNE, KESSLER, GOLDSTEIN & FOX P.L. L.C. (I) 1100 NEW YORKAVENUE, N.W. WASHINGTON, DC 20005 (US) (73) Assignee: Bayer Cropscience AG, Monheim (DE) (21) Appl. No.: 12/639,536 (22) Filed: Mar. 11, 2010 in which W, X, Y, Z and CKE are each as defined above, to several methods and intermediates for preparation thereof (30) Foreign Application Priority Data and to the use thereofas pesticides and/or herbicides. The invention also relates to selective herbicidal composi Mar. -

CAS Number Index
2334 CAS Number Index CAS # Page Name CAS # Page Name CAS # Page Name 50-00-0 905 Formaldehyde 56-81-5 967 Glycerol 61-90-5 1135 Leucine 50-02-2 596 Dexamethasone 56-85-9 963 Glutamine 62-44-2 1640 Phenacetin 50-06-6 1654 Phenobarbital 57-00-1 514 Creatine 62-46-4 1166 α-Lipoic acid 50-11-3 1288 Metharbital 57-22-7 2229 Vincristine 62-53-3 131 Aniline 50-12-4 1245 Mephenytoin 57-24-9 1950 Strychnine 62-73-7 626 Dichlorvos 50-23-7 1017 Hydrocortisone 57-27-2 1428 Morphine 63-05-8 127 Androstenedione 50-24-8 1739 Prednisolone 57-41-0 1672 Phenytoin 63-25-2 335 Carbaryl 50-29-3 569 DDT 57-42-1 1239 Meperidine 63-75-2 142 Arecoline 50-33-9 1666 Phenylbutazone 57-43-2 108 Amobarbital 64-04-0 1648 Phenethylamine 50-34-0 1770 Propantheline bromide 57-44-3 191 Barbital 64-13-1 1308 p-Methoxyamphetamine 50-35-1 2054 Thalidomide 57-47-6 1683 Physostigmine 64-17-5 784 Ethanol 50-36-2 497 Cocaine 57-53-4 1249 Meprobamate 64-18-6 909 Formic acid 50-37-3 1197 Lysergic acid diethylamide 57-55-6 1782 Propylene glycol 64-77-7 2104 Tolbutamide 50-44-2 1253 6-Mercaptopurine 57-66-9 1751 Probenecid 64-86-8 506 Colchicine 50-47-5 589 Desipramine 57-74-9 398 Chlordane 65-23-6 1802 Pyridoxine 50-48-6 103 Amitriptyline 57-92-1 1947 Streptomycin 65-29-2 931 Gallamine 50-49-7 1053 Imipramine 57-94-3 2179 Tubocurarine chloride 65-45-2 1888 Salicylamide 50-52-2 2071 Thioridazine 57-96-5 1966 Sulfinpyrazone 65-49-6 98 p-Aminosalicylic acid 50-53-3 426 Chlorpromazine 58-00-4 138 Apomorphine 66-76-2 632 Dicumarol 50-55-5 1841 Reserpine 58-05-9 1136 Leucovorin 66-79-5 -

Letters to the Editor
Letters to the Editor Internet Pharmacy Prescription complete the medication database. Of course, patients can abuse and Phentermine Overdose any medications, so collaboration between pharmacies and physicians is essential to minimize this risk. Sir: The Internet is now widely used by patients for both Dr. Takeshita reports no financial or other relationship relevant to the health information and prescription services. Yet, a MEDLINE subject matter of this letter. search in January 2002 using the phrase “Internet pharmacy” showed a total of 99 articles; nearly all were geared toward REFERENCES health care management or the general public. There are only a few published reports of bad outcome resulting from medical 1 1. Crocco AG, Villasis-Keever M, Jadad AR. Analysis of cases of information obtained from the Internet. The U.S. Food and harm associated with use of health information on the Internet. Drug Administration noted 326 Internet sites selling pharma- JAMA 2002;287:2867–2871 ceutical products.2 The exact numbers are difficult to quantify 2. Henney JE. Cyberpharmacies and the role of the US Food and Drug as Web sites are constantly changing. I report a case of overdose Administration. J Med Internet Res 2001;3:E3 with phentermine that was obtained through an Internet 3. Gardin JM, Schumacher D, Constantine G, et al. Valvular abnormali- pharmacy. ties and cardiovascular status following exposure to dexfenfluramine or phentermine/fenfluramine. JAMA 2000;283:1703–1709 4. Koury E, Stone CK, Stapczynski JS, et al. Sympathetic overactivity Case report. Ms. A, a 20-year-old woman with a prior from fenfluramine-phentermine overdose. -
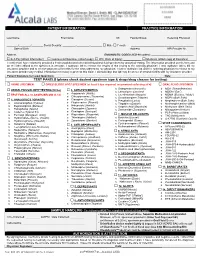
Please Check Desired Specimen Type & Drugs/Drug Classes for Testing
PATIENT INFORMATION PRACTICE INFORMATION ____________________________________ _____________________________________ _______ ________________________ __________________ Last Name First Name MI Facility/Group Referring Physician ________/________/________ Social Security: _________-_________-________ ☐ Male ☐ Female ___________________________________________ Date of Birth Address NPI Provider Nr. __________________________________________________________________ Address DIAGNOSTIC CODES (ICD-10 codes): _____________________________ ☐ Self-Pay (attach Information) ☐ Commercial Insurance (attach copy) ☐ W/C (Date of Injury): ____________ ☐ Medicare (attach copy of Insurance) I certify that I have voluntarily provided a fresh unadulterated urine/dried blood/oral fluid specimen for analytical testing. The information provided on this form and on the label affixed to the specimen is accurate. I authorize lab to release the results of this testing to the ordering physician. I also authorize lab to bill my insurance provider and to receive payment of benefits for the tests ordered by my physician. I further authorize lab and the ordering physician to release to my insurance provider any medical information necessary to process this claim. I acknowledge that lab may be an out-of-network facility with my insurance provider. Patient Signature (or Legal Guardian): ___________________________________________________________________________ Date: _______________ TEST PANELS (please check desired specimen type & drugs/drug classes for testing): ☐ URINE -

Kava Kava Extract Is Available from Ashland Chemical Co., Mini Star International, Inc., and QBI (Quality Botanical Ingredients, Inc.)
SUMMARY OF DATA FOR CHEMICAL SELECTION Kava Kava 9000-38-8; 84696-40-2 November 1998 TABLE OF CONTENTS Basis for Nomination Chemical Identification Production Information Use Pattern Human Exposure Regulatory Status Evidence for Possible Carcinogenic Activity Human Data Animal Data Metabolism Other Biological Effects Structure-Activity Relationships References BASIS OF NOMINATION TO THE CSWG Kava kava is brought to the attention of the CSWG because it is a rapidly growing, highly used dietary supplement introduced into the mainstream U.S. market relatively recently. Through this use, millions of consumers using antianxiety preparations are potentially exposed to kava kava. A traditional beverage of various Pacific Basin countries, kava clearly has psychoactive properties. The effects of its long-term consumption have not been documented adequately; preliminary studies suggest possibly serious organ system effects. The potential carcinogenicity of kava and its principal constituents are unknown. INPUT FROM GOVERNMENT AGENCIES/INDUSTRY The U.S. Pharmacopeia is in the process of reviewing kava kava. No decision on preparation of a monograph has been made. SELECTION STATUS ACTION BY CSWG: 12/14/98 Studies requested: - Toxicological evaluation, to include studies of reproductive toxicity and neurotoxicity - Genotoxicity Priority: High Rationale/Remarks: - Significant human exposure - Leading dietary supplement with rapidly growing use - Concern that kava has been promoted as a substitute for ritilin in children - Test extract standardized to 30 percent kavalactones - NCI is conducting studies in Salmonella typhimurium CHEMICAL IDENTIFICATION CAS Registry Number: 9000-38-8 Kava-kava resin (8CI) Chemical Abstract Service Name: 84696-40-2 CAS Registry Number: Pepper (Piper), P. methysticum, ext. Chemical Abstract Service Name: Extract of kava; kava extract; Piper Synonyms and Trade Names: methisticum extract Description: The tropical shrub Piper methysticum is widely cultivated in the South Pacific. -

A Review of the Literature
Pharmacogn J. 2019; 11(6)Suppl:1511-1525 A Multifaceted Journal in the field of Natural Products and Pharmacognosy Original Article www.phcogj.com Phytochemical and Pharmacological Support for the Traditional Uses of Zingiberacea Species in Suriname - A Review of the Literature Dennis RA Mans*, Meryll Djotaroeno, Priscilla Friperson, Jennifer Pawirodihardjo ABSTRACT The Zingiberacea or ginger family is a family of flowering plants comprising roughly 1,600 species of aromatic perennial herbs with creeping horizontal or tuberous rhizomes divided into about 50 genera. The Zingiberaceae are distributed throughout tropical Africa, Asia, and the Americas. Many members are economically important as spices, ornamentals, cosmetics, Dennis RA Mans*, Meryll traditional medicines, and/or ingredients of religious rituals. One of the most prominent Djotaroeno, Priscilla Friperson, characteristics of this plant family is the presence of essential oils in particularly the rhizomes Jennifer Pawirodihardjo but in some cases also the leaves and other parts of the plant. The essential oils are in general Department of Pharmacology, Faculty of made up of a variety of, among others, terpenoid and phenolic compounds with important Medical Sciences, Anton de Kom University of biological activities. The Republic of Suriname (South America) is well-known for its ethnic and Suriname, Paramaribo, SURINAME. cultural diversity as well as its extensive ethnopharmacological knowledge and unique plant Correspondence biodiversity. This paper first presents some general information on the Zingiberacea family, subsequently provides some background about Suriname and the Zingiberacea species in the Dennis RA Mans country, then extensively addresses the traditional uses of one representative of the seven Department of Pharmacology, Faculty of Medical Sciences, Anton de Kom genera in the country and provides the phytochemical and pharmacological support for these University of Suriname, Kernkampweg 6, uses, and concludes with a critical appraisal of the medicinal values of these plants. -

Kavain, the Major Constituent of the Anxiolytic Kava
RESEARCH ARTICLE Kavain, the Major Constituent of the Anxiolytic Kava Extract, Potentiates GABAA Receptors: Functional Characteristics and Molecular Mechanism Han Chow Chua1, Emilie T. H. Christensen1,2, Kirsten Hoestgaard-Jensen2, Leonny Y. Hartiadi1, Iqbal Ramzan1, Anders A. Jensen2, Nathan L. Absalom1, Mary Chebib1* 1 Faculty of Pharmacy, The University of Sydney, Sydney, New South Wales, Australia, 2 Department of a11111 Drug Design and Pharmacology, Faculty of Health and Medical Sciences, University of Copenhagen, Copenhagen, Denmark * [email protected] Abstract OPEN ACCESS Extracts of the pepper plant kava (Piper methysticum) are effective in alleviating anxiety in Citation: Chua HC, Christensen ETH, Hoestgaard- Jensen K, Hartiadi LY, Ramzan I, Jensen AA, et al. clinical trials. Despite the long-standing therapeutic interest in kava, the molecular target(s) (2016) Kavain, the Major Constituent of the Anxiolytic of the pharmacologically active constituents, kavalactones have not been established. γ- Kava Extract, Potentiates GABAA Receptors: Aminobutyric acid type A receptors (GABAARs) are assumed to be the in vivo molecular tar- Functional Characteristics and Molecular Mechanism. PLoS ONE 11(6): e0157700. doi:10.1371/journal. get of kavalactones based on data from binding assays, but evidence in support of a direct pone.0157700 interaction between kavalactones and GABAARs is scarce and equivocal. In this study, we Editor: Steven Barnes, Dalhousie University, characterised the functional properties of the major anxiolytic kavalactone, kavain at human CANADA recombinant α1β2, β2γ2L, αxβ2γ2L (x = 1, 2, 3 and 5), α1βxγ2L (x = 1, 2 and 3) and α4β2δ Received: March 24, 2016 GABAARs expressed in Xenopus oocytes using the two-electrode voltage clamp technique. -

Analytical Studies on the Kavain Metabolism in Human Specimen and Liver Cell Lines
Analytical studies on the kavain metabolism in human specimen and liver cell lines Inaugural-Dissertation zur Erlangung des Doktorgrades der Mathematisch-Naturwissenschaftlichen Fakultät der Heinrich-Heine-Universität Düsseldorf Vorgelegt von Fuad Ali Tarbah aus Derna, Libyen Düsseldorf 2003 Gedruckt mit Genehmigung der Mathematisch-Naturwissenschaftlichen Fakultät der Heinrich-Heine-Universität Düsseldorf Referent: Prof. Dr. Th. Daldrup Korreferent: Prof. Dr. G. Willuhn, Prof. Dr. H. Weber Tag der mündlichen Prüfung: 17. 12. 2003 Parts of this Ph.D. Thesis have already been presented and/or published in: Tarbah F. A., Mahler H., Temme O. and Daldrup Th. Mass spectral characterisation of hepatic cell metabolites of D,L-kavain using HPLC and GC/MS systems. Special issue: 37th TIAFT triennial meeting “Problems of Forensic Sciences” XLII: 173-180 (1999) Tarbah F. A., Mahler H., Temme O. and Daldrup Th. Determination of D,L-kavain and its metabolites in blood, serum and urine. Rapid quantitative method using fluid/fluid extraction and gas chromatography/mass spectrometry (GC/MS). Poster in 79. Jahrestagung der Deutschen Gesellschaft für Rechtsmedizin, Medizinische Einrichtungen der Universität / Gesamthochschule Essen (2000) Tarbah F., Mahler H., Kardel B., Weinmann W., Hafner D. and Daldrup Th. Kinetics of kavain and its metabolites after oral application. J. Chromatogr. B 789 (1): 115-130 (2003) Cabalion P., Barguil Y., Duhet D., Mandeau A., Warter S., Russmann S., Tarbah F. and Daldrup Th. Kava in modern therapeutic uses: to a better evaluation -

Piper Methysticum)
Journal of Student Research (2015) Volume 4, Issue 2: pp. 69-72 Research Article A Closer Look at the Risks vs. Benefits of Kava (Piper methysticum) Anan A. Husseina If you took a trip to Fiji, the locals would probably welcome you with a drink of Kava. For centuries, the indigenous people of the South Pacific Islands have used the roots of a plant known as Kava. Beyond the use of Kava as a psychoactive substance, it has been incorporated as a cultural drink that is used in many ceremonies. In the late 1990’s Kava use spread quickly in Western countries including Europe, North America, and Australia. It was used as a treatment for anxiety. But just as quickly as it spread, the enthusiasm for it faded, because it was banned or restricted in many Western countries following reports of liver toxicity. In the United States, the Food and Drug Administration’s (FDA) concern for safety prompted a request for more research on the substance. The issues of safety and efficacy remain more specifically whether the benefits of using Kava outweigh the risks. History Kava is a beverage made from the roots of the plant included alcohol, cocaine, tobacco, and heroin. The findings Piper methysticum, and has been used historically in the suggest that kava may reduce the craving associated with the South Pacific Islands as a ceremonial drink. Kava was aforementioned substances, which may make kava a great introduced in Europe around the 1700s by Captain James future candidate to help with addiction. 13 Cook and has since spread widely to Australia, Europe, and Although the mechanism of action is not clear, it is the United States.