Systematic Evaluation of 1-Chlorobutane for Liquid-Liquid Extraction of Drugs U
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

AO-Klasifikácia Faktúr →Zlomeniny
AO-klasifikácia faktúr →zlomeniny. AOP-syndróm – skr. syndroma adipositas–oligomenorrhoea–parotis. aorta – [g. aorté srdcovnica] srdcovnica. Začína sa z ľavej komory a vystupuje kraniálne aţ do výšky 2. pravého sternokostálneho kĺbu ako aorta ascendens, pokračovaním je oblúk arcus aortae, aorta descendens, aorta thoracia a aorta abdominalis. Aorta ascendens – začína sa v ľavej komore nad polmesiačikovitými chlopňami a skoro celá sa nachádza v perikarde. Je dlhá asi 4 – 5 cm, jej priemer je 22 – 30 mm. Ihneď nad chlop-ňami je následkom spätných nárazov krvi mierne vydutá do tzv. sinus aortae, výraznejšie u starších osôb. Oddiely a. obsahujúce sinus aortae sa nazývajú bulbus aortae. U starších osôb býva následkom nárazov krvi širší aj koncový úsek vzostupnej a. pred jej prechodom do oblúka, tzv. sinus maximus (quartus) aortae. Tu býva u starších osôb a. často rozširená. A. ascendens, ako aj začiatok arcus aortae majú špeciálne vasa vasorum pochádzajúce z vencovitých tepien (aa. cardiaortales). Tento úsek osobitne patogeneticky rizikový. Začiatok aorta ascendens je ešte obalený vo vagina serosa arteriarum, kt. tvorí na ventrálnom obvode a. priečnu krkvu podloţenú subseróznym tukovým väzivom (Concatova-Bacceli tuková krkva). Vnútri vagina arteriarum je aorta ascendens a začiatrok a. pulmonalis spojené tuhým väzivom (vincula aortae Rindfleischi). Výstup aorta ascendens kryje spredu začiatok a. pulmonalis, ventrálne a vpravo je auricula dextra, dorzálne je uloţený r. dexter a. pulmonalis. Kraniálne vpravo od a. je v. cava superior, vľavo kmeň a. pulmonalis. Z ventrálneho a ľavého sinus aortae sa začína a. coronaria cordis dextra et sinistra. Aorta ascendens a arcus aortae Arcus aortae – je dlhý asi 6 cm, začína sa za sternom vo výške úponu 2. -

(19) United States (12) Patent Application Publication (10) Pub
US 20130289061A1 (19) United States (12) Patent Application Publication (10) Pub. No.: US 2013/0289061 A1 Bhide et al. (43) Pub. Date: Oct. 31, 2013 (54) METHODS AND COMPOSITIONS TO Publication Classi?cation PREVENT ADDICTION (51) Int. Cl. (71) Applicant: The General Hospital Corporation, A61K 31/485 (2006-01) Boston’ MA (Us) A61K 31/4458 (2006.01) (52) U.S. Cl. (72) Inventors: Pradeep G. Bhide; Peabody, MA (US); CPC """"" " A61K31/485 (201301); ‘4161223011? Jmm‘“ Zhu’ Ansm’ MA. (Us); USPC ......... .. 514/282; 514/317; 514/654; 514/618; Thomas J. Spencer; Carhsle; MA (US); 514/279 Joseph Biederman; Brookline; MA (Us) (57) ABSTRACT Disclosed herein is a method of reducing or preventing the development of aversion to a CNS stimulant in a subject (21) App1_ NO_; 13/924,815 comprising; administering a therapeutic amount of the neu rological stimulant and administering an antagonist of the kappa opioid receptor; to thereby reduce or prevent the devel - . opment of aversion to the CNS stimulant in the subject. Also (22) Flled' Jun‘ 24’ 2013 disclosed is a method of reducing or preventing the develop ment of addiction to a CNS stimulant in a subj ect; comprising; _ _ administering the CNS stimulant and administering a mu Related U‘s‘ Apphcatlon Data opioid receptor antagonist to thereby reduce or prevent the (63) Continuation of application NO 13/389,959, ?led on development of addiction to the CNS stimulant in the subject. Apt 27’ 2012’ ?led as application NO_ PCT/US2010/ Also disclosed are pharmaceutical compositions comprising 045486 on Aug' 13 2010' a central nervous system stimulant and an opioid receptor ’ antagonist. -

UFC PROHIBITED LIST Effective June 1, 2021 the UFC PROHIBITED LIST
UFC PROHIBITED LIST Effective June 1, 2021 THE UFC PROHIBITED LIST UFC PROHIBITED LIST Effective June 1, 2021 PART 1. Except as provided otherwise in PART 2 below, the UFC Prohibited List shall incorporate the most current Prohibited List published by WADA, as well as any WADA Technical Documents establishing decision limits or reporting levels, and, unless otherwise modified by the UFC Prohibited List or the UFC Anti-Doping Policy, Prohibited Substances, Prohibited Methods, Specified or Non-Specified Substances and Specified or Non-Specified Methods shall be as identified as such on the WADA Prohibited List or WADA Technical Documents. PART 2. Notwithstanding the WADA Prohibited List and any otherwise applicable WADA Technical Documents, the following modifications shall be in full force and effect: 1. Decision Concentration Levels. Adverse Analytical Findings reported at a concentration below the following Decision Concentration Levels shall be managed by USADA as Atypical Findings. • Cannabinoids: natural or synthetic delta-9-tetrahydrocannabinol (THC) or Cannabimimetics (e.g., “Spice,” JWH-018, JWH-073, HU-210): any level • Clomiphene: 0.1 ng/mL1 • Dehydrochloromethyltestosterone (DHCMT) long-term metabolite (M3): 0.1 ng/mL • Selective Androgen Receptor Modulators (SARMs): 0.1 ng/mL2 • GW-1516 (GW-501516) metabolites: 0.1 ng/mL • Epitrenbolone (Trenbolone metabolite): 0.2 ng/mL 2. SARMs/GW-1516: Adverse Analytical Findings reported at a concentration at or above the applicable Decision Concentration Level but under 1 ng/mL shall be managed by USADA as Specified Substances. 3. Higenamine: Higenamine shall be a Prohibited Substance under the UFC Anti-Doping Policy only In-Competition (and not Out-of- Competition). -

Central Valley Toxicology Drug List
Chloroform ~F~ Lithium ~A~ Chlorpheniramine Loratadine Famotidine Acebutolol Chlorpromazine Lorazepam Fenoprofen Acetaminophen Cimetidine Loxapine Fentanyl Acetone Citalopram LSD (Lysergide) Fexofenadine 6-mono- Clomipramine acetylmorphine Flecainide ~M~ Clonazepam a-Hydroxyalprazolam Fluconazole Maprotiline Clonidine a-Hydroxytriazolam Flunitrazepam MDA Clorazepate Albuterol Fluoxetine MDMA Clozapine Alprazolam Fluphenazine Medazepam Cocaethylene Amantadine Flurazepam Meperidine Cocaine 7-Aminoflunitrazepam Fluvoxamine Mephobarbital Codeine Amiodarone Fosinopril Meprobamate Conine Amitriptyline Furosemide Mesoridazine Cotinine Amlodipine Methadone Cyanide ~G~ Amobarbital Methanol Cyclobenzaprine Gabapentin Amoxapine d-Methamphetamine Cyclosporine GHB d-Amphetamine l-Methamphetamine Glutethamide l-Amphetamine ~D~ Methapyrilene Guaifenesin Aprobarbital Demoxepam Methaqualone Atenolol Desalkylfurazepam ~H~ Methocarbamol Atropine Desipramine Halazepam Methylphenidate ~B~ Desmethyldoxepin Haloperidol Methyprylon Dextromethoraphan Heroin Metoclopramide Baclofen Diazepam Hexobarbital Metoprolol Barbital Digoxin Hydrocodone Mexiletine Benzoylecgonine Dihydrocodein Hydromorphone Midazolam Benzphetamine Dihydrokevain Hydroxychloroquine Mirtazapine Benztropine Diltiazem Hydroxyzine Morphine (Total/Free) Brodificoum Dimenhydrinate Bromazepam ~N~ Diphenhydramine ~I~ Bupivacaine Nafcillin Disopyramide Ibuprofen Buprenorphine Naloxone Doxapram Imipramine Bupropion Naltrexone Doxazosin Indomethacin Buspirone NAPA Doxepin Isoniazid Butabarbital Naproxen -

CAS Number Index
2334 CAS Number Index CAS # Page Name CAS # Page Name CAS # Page Name 50-00-0 905 Formaldehyde 56-81-5 967 Glycerol 61-90-5 1135 Leucine 50-02-2 596 Dexamethasone 56-85-9 963 Glutamine 62-44-2 1640 Phenacetin 50-06-6 1654 Phenobarbital 57-00-1 514 Creatine 62-46-4 1166 α-Lipoic acid 50-11-3 1288 Metharbital 57-22-7 2229 Vincristine 62-53-3 131 Aniline 50-12-4 1245 Mephenytoin 57-24-9 1950 Strychnine 62-73-7 626 Dichlorvos 50-23-7 1017 Hydrocortisone 57-27-2 1428 Morphine 63-05-8 127 Androstenedione 50-24-8 1739 Prednisolone 57-41-0 1672 Phenytoin 63-25-2 335 Carbaryl 50-29-3 569 DDT 57-42-1 1239 Meperidine 63-75-2 142 Arecoline 50-33-9 1666 Phenylbutazone 57-43-2 108 Amobarbital 64-04-0 1648 Phenethylamine 50-34-0 1770 Propantheline bromide 57-44-3 191 Barbital 64-13-1 1308 p-Methoxyamphetamine 50-35-1 2054 Thalidomide 57-47-6 1683 Physostigmine 64-17-5 784 Ethanol 50-36-2 497 Cocaine 57-53-4 1249 Meprobamate 64-18-6 909 Formic acid 50-37-3 1197 Lysergic acid diethylamide 57-55-6 1782 Propylene glycol 64-77-7 2104 Tolbutamide 50-44-2 1253 6-Mercaptopurine 57-66-9 1751 Probenecid 64-86-8 506 Colchicine 50-47-5 589 Desipramine 57-74-9 398 Chlordane 65-23-6 1802 Pyridoxine 50-48-6 103 Amitriptyline 57-92-1 1947 Streptomycin 65-29-2 931 Gallamine 50-49-7 1053 Imipramine 57-94-3 2179 Tubocurarine chloride 65-45-2 1888 Salicylamide 50-52-2 2071 Thioridazine 57-96-5 1966 Sulfinpyrazone 65-49-6 98 p-Aminosalicylic acid 50-53-3 426 Chlorpromazine 58-00-4 138 Apomorphine 66-76-2 632 Dicumarol 50-55-5 1841 Reserpine 58-05-9 1136 Leucovorin 66-79-5 -
Kava - the Unfolding Story: Report on a Work-In-Progress
Article Kava - the unfolding story: Report on a work-in-progress. Denham, Alison, McIntyre, Michael and Whitehouse, Jule Available at http://clok.uclan.ac.uk/9455/ Denham, Alison, McIntyre, Michael and Whitehouse, Jule Kava - the unfolding story: Report on a work-in-progress. Journal of Alternative and Complementary Medicine, 8 (3). pp. 237-263. It is advisable to refer to the publisher’s version if you intend to cite from the work. For more information about UCLan’s research in this area go to http://www.uclan.ac.uk/researchgroups/ and search for <name of research Group>. For information about Research generally at UCLan please go to http://www.uclan.ac.uk/research/ All outputs in CLoK are protected by Intellectual Property Rights law, including Copyright law. Copyright, IPR and Moral Rights for the works on this site are retained by the individual authors and/or other copyright owners. Terms and conditions for use of this material are defined in the policies page. CLoK Central Lancashire online Knowledge www.clok.uclan.ac.uk THE JOURNAL OF ALTERNATIVE AND COMPLEMENTARY MEDICINE Volume 8, Number 3, 2002, pp. 237–263 © Mary Ann Liebert, Inc. SPECIAL REPORT Kava—the Unfolding Story: Report on a Work-in-Progress ALISON DENHAM, B.A. (Soc.), M.N.I.M.H., 1 MICHAEL McINTYRE, M.A., F.N.I.M.H., F.R.C.H.M., M.B.Ac.C., 2 and JULIE WHITEHOUSE, Ph.D., M.N.I.M.H. 3 ABSTRACT This paper, originated as a submission (now updated) to the U.K. Medicines Control Agency and Committee of Safety of Medicines (CSM) on January 11, 2002, in response to a report circu- lated by the German Federal Institute for Drugs and Medical Products (German initials are BfArM), a compilation of which is summarized in Appendix 2. -

Letters to the Editor
Letters to the Editor Internet Pharmacy Prescription complete the medication database. Of course, patients can abuse and Phentermine Overdose any medications, so collaboration between pharmacies and physicians is essential to minimize this risk. Sir: The Internet is now widely used by patients for both Dr. Takeshita reports no financial or other relationship relevant to the health information and prescription services. Yet, a MEDLINE subject matter of this letter. search in January 2002 using the phrase “Internet pharmacy” showed a total of 99 articles; nearly all were geared toward REFERENCES health care management or the general public. There are only a few published reports of bad outcome resulting from medical 1 1. Crocco AG, Villasis-Keever M, Jadad AR. Analysis of cases of information obtained from the Internet. The U.S. Food and harm associated with use of health information on the Internet. Drug Administration noted 326 Internet sites selling pharma- JAMA 2002;287:2867–2871 ceutical products.2 The exact numbers are difficult to quantify 2. Henney JE. Cyberpharmacies and the role of the US Food and Drug as Web sites are constantly changing. I report a case of overdose Administration. J Med Internet Res 2001;3:E3 with phentermine that was obtained through an Internet 3. Gardin JM, Schumacher D, Constantine G, et al. Valvular abnormali- pharmacy. ties and cardiovascular status following exposure to dexfenfluramine or phentermine/fenfluramine. JAMA 2000;283:1703–1709 4. Koury E, Stone CK, Stapczynski JS, et al. Sympathetic overactivity Case report. Ms. A, a 20-year-old woman with a prior from fenfluramine-phentermine overdose. -
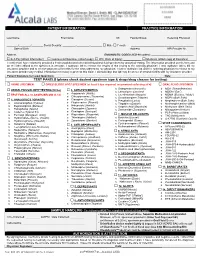
Please Check Desired Specimen Type & Drugs/Drug Classes for Testing
PATIENT INFORMATION PRACTICE INFORMATION ____________________________________ _____________________________________ _______ ________________________ __________________ Last Name First Name MI Facility/Group Referring Physician ________/________/________ Social Security: _________-_________-________ ☐ Male ☐ Female ___________________________________________ Date of Birth Address NPI Provider Nr. __________________________________________________________________ Address DIAGNOSTIC CODES (ICD-10 codes): _____________________________ ☐ Self-Pay (attach Information) ☐ Commercial Insurance (attach copy) ☐ W/C (Date of Injury): ____________ ☐ Medicare (attach copy of Insurance) I certify that I have voluntarily provided a fresh unadulterated urine/dried blood/oral fluid specimen for analytical testing. The information provided on this form and on the label affixed to the specimen is accurate. I authorize lab to release the results of this testing to the ordering physician. I also authorize lab to bill my insurance provider and to receive payment of benefits for the tests ordered by my physician. I further authorize lab and the ordering physician to release to my insurance provider any medical information necessary to process this claim. I acknowledge that lab may be an out-of-network facility with my insurance provider. Patient Signature (or Legal Guardian): ___________________________________________________________________________ Date: _______________ TEST PANELS (please check desired specimen type & drugs/drug classes for testing): ☐ URINE -

Kava Kava Extract Is Available from Ashland Chemical Co., Mini Star International, Inc., and QBI (Quality Botanical Ingredients, Inc.)
SUMMARY OF DATA FOR CHEMICAL SELECTION Kava Kava 9000-38-8; 84696-40-2 November 1998 TABLE OF CONTENTS Basis for Nomination Chemical Identification Production Information Use Pattern Human Exposure Regulatory Status Evidence for Possible Carcinogenic Activity Human Data Animal Data Metabolism Other Biological Effects Structure-Activity Relationships References BASIS OF NOMINATION TO THE CSWG Kava kava is brought to the attention of the CSWG because it is a rapidly growing, highly used dietary supplement introduced into the mainstream U.S. market relatively recently. Through this use, millions of consumers using antianxiety preparations are potentially exposed to kava kava. A traditional beverage of various Pacific Basin countries, kava clearly has psychoactive properties. The effects of its long-term consumption have not been documented adequately; preliminary studies suggest possibly serious organ system effects. The potential carcinogenicity of kava and its principal constituents are unknown. INPUT FROM GOVERNMENT AGENCIES/INDUSTRY The U.S. Pharmacopeia is in the process of reviewing kava kava. No decision on preparation of a monograph has been made. SELECTION STATUS ACTION BY CSWG: 12/14/98 Studies requested: - Toxicological evaluation, to include studies of reproductive toxicity and neurotoxicity - Genotoxicity Priority: High Rationale/Remarks: - Significant human exposure - Leading dietary supplement with rapidly growing use - Concern that kava has been promoted as a substitute for ritilin in children - Test extract standardized to 30 percent kavalactones - NCI is conducting studies in Salmonella typhimurium CHEMICAL IDENTIFICATION CAS Registry Number: 9000-38-8 Kava-kava resin (8CI) Chemical Abstract Service Name: 84696-40-2 CAS Registry Number: Pepper (Piper), P. methysticum, ext. Chemical Abstract Service Name: Extract of kava; kava extract; Piper Synonyms and Trade Names: methisticum extract Description: The tropical shrub Piper methysticum is widely cultivated in the South Pacific. -

Prohibited Substances List
Prohibited Substances List This is the Equine Prohibited Substances List that was voted in at the FEI General Assembly in November 2009 alongside the new Equine Anti-Doping and Controlled Medication Regulations(EADCMR). Neither the List nor the EADCM Regulations are in current usage. Both come into effect on 1 January 2010. The current list of FEI prohibited substances remains in effect until 31 December 2009 and can be found at Annex II Vet Regs (11th edition) Changes in this List : Shaded row means that either removed or allowed at certain limits only SUBSTANCE ACTIVITY Banned Substances 1 Acebutolol Beta blocker 2 Acefylline Bronchodilator 3 Acemetacin NSAID 4 Acenocoumarol Anticoagulant 5 Acetanilid Analgesic/anti-pyretic 6 Acetohexamide Pancreatic stimulant 7 Acetominophen (Paracetamol) Analgesic/anti-pyretic 8 Acetophenazine Antipsychotic 9 Acetylmorphine Narcotic 10 Adinazolam Anxiolytic 11 Adiphenine Anti-spasmodic 12 Adrafinil Stimulant 13 Adrenaline Stimulant 14 Adrenochrome Haemostatic 15 Alclofenac NSAID 16 Alcuronium Muscle relaxant 17 Aldosterone Hormone 18 Alfentanil Narcotic 19 Allopurinol Xanthine oxidase inhibitor (anti-hyperuricaemia) 20 Almotriptan 5 HT agonist (anti-migraine) 21 Alphadolone acetate Neurosteriod 22 Alphaprodine Opiod analgesic 23 Alpidem Anxiolytic 24 Alprazolam Anxiolytic 25 Alprenolol Beta blocker 26 Althesin IV anaesthetic 27 Althiazide Diuretic 28 Altrenogest (in males and gelidngs) Oestrus suppression 29 Alverine Antispasmodic 30 Amantadine Dopaminergic 31 Ambenonium Cholinesterase inhibition 32 Ambucetamide Antispasmodic 33 Amethocaine Local anaesthetic 34 Amfepramone Stimulant 35 Amfetaminil Stimulant 36 Amidephrine Vasoconstrictor 37 Amiloride Diuretic 1 Prohibited Substances List This is the Equine Prohibited Substances List that was voted in at the FEI General Assembly in November 2009 alongside the new Equine Anti-Doping and Controlled Medication Regulations(EADCMR). -

Kavain, the Major Constituent of the Anxiolytic Kava
RESEARCH ARTICLE Kavain, the Major Constituent of the Anxiolytic Kava Extract, Potentiates GABAA Receptors: Functional Characteristics and Molecular Mechanism Han Chow Chua1, Emilie T. H. Christensen1,2, Kirsten Hoestgaard-Jensen2, Leonny Y. Hartiadi1, Iqbal Ramzan1, Anders A. Jensen2, Nathan L. Absalom1, Mary Chebib1* 1 Faculty of Pharmacy, The University of Sydney, Sydney, New South Wales, Australia, 2 Department of a11111 Drug Design and Pharmacology, Faculty of Health and Medical Sciences, University of Copenhagen, Copenhagen, Denmark * [email protected] Abstract OPEN ACCESS Extracts of the pepper plant kava (Piper methysticum) are effective in alleviating anxiety in Citation: Chua HC, Christensen ETH, Hoestgaard- Jensen K, Hartiadi LY, Ramzan I, Jensen AA, et al. clinical trials. Despite the long-standing therapeutic interest in kava, the molecular target(s) (2016) Kavain, the Major Constituent of the Anxiolytic of the pharmacologically active constituents, kavalactones have not been established. γ- Kava Extract, Potentiates GABAA Receptors: Aminobutyric acid type A receptors (GABAARs) are assumed to be the in vivo molecular tar- Functional Characteristics and Molecular Mechanism. PLoS ONE 11(6): e0157700. doi:10.1371/journal. get of kavalactones based on data from binding assays, but evidence in support of a direct pone.0157700 interaction between kavalactones and GABAARs is scarce and equivocal. In this study, we Editor: Steven Barnes, Dalhousie University, characterised the functional properties of the major anxiolytic kavalactone, kavain at human CANADA recombinant α1β2, β2γ2L, αxβ2γ2L (x = 1, 2, 3 and 5), α1βxγ2L (x = 1, 2 and 3) and α4β2δ Received: March 24, 2016 GABAARs expressed in Xenopus oocytes using the two-electrode voltage clamp technique. -

Doping Control of Athletes
trends in analytical chemistry, vol. 7, no. IO, I988 375 trends Doping control of athletes E. G. de Jong*, I?. A. A. Maes and The definition of the Council of Europe for doping J. M. van Rossum is2: Utrecht, Netherlands ‘The administration to or the use by a healthy indi- vidual in any way of compounds which are not natu- History ral to the organism or the use of physiological com- The origin of the word doping is not certain. It first pounds in abnormal doses or in an abnormal way appeared in the English dictionaries at the end of the with the only purpose to artificially and dishonestly nineteenth century. The first reference to the use of influence the performance of this person during doping by athletes was in 1864 during swimming competition.’ competitions that were held in the canals of Amster- Another possible definition is: dam. The use of what is known as a ‘speedball’, a ‘The use of compounds which are not synthesized mixture of heroine and cocaine, by cyclists was de- by the human body or the use of endogenous com- scribed in 1869. In 1904 the Russian chemist pounds in excessive doses with the aim to improve Bukowski was able to identify some alkaloids in the performance in sport competitions.’ saliva of horses’. A simpler definition is: Australia was the first country to take measures ‘The use of forbidden drugs. ’ against doping in sports in 1962, and England fol- The last definition can only be used when we have lowed with the drugs bill in 1964.