Ian Hector Frazer (1953– ) [1]
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Picture As Pdf Download
MJA Centenary — History of Australian Medicine A history of health and medical research in Australia Timothy Dyke ealth and medical research has signifi cantly con- BVSc, PhD, MBA Summary Executive Director, tributed to improvements in human health and Health and medical research has played an important Strategic Policy Group H wellbeing throughout the world, and Australia has role in improving the life of Australians since before Warwick P Anderson played its part. As a result of this research, Australians have the 20th century, with many Australian researchers PhD benefi ted by remaining healthier for longer through better contributing to important advances both locally and Chief Executive Officer internationally. treatments and improved health care, and from contribu- National Health and Medical tions to national wealth through the development of in- The establishment of the National Health and Medical Research Council, Research Council (NHMRC) to support research and Canberra, ACT. novative industries. Despite the signifi cant role of research to work to achieve the benefi ts of research for the timothy.dyke@ in Australia, there have been few specifi c compilations on community was signifi cant. nhmrc.gov.au the Australian history of health and medical research. This The NHMRC has also provided guidance in research and article is a brief overview of Australian health and medical health ethics. doi: 10.5694/mja14.00347 research, with the role of the National Health and Medical Australian research has broadened to include basic Research Council (NHMRC) as a main focus. biomedical science, clinical medicine and science, public health and health services. The early years In October 2002, the NHMRC adopted Indigenous health research as a strategic priority. -

Annual Review LETTER of TRANSMITTAL
2016 annual review LETTER OF TRANSMITTAL The Hon Susan Close MP Minister for Education and Child Development Minister for Higher Education and Skills Level 9, 31 Flinders Street Adelaide SA 5000 30 May 2017 Dear Minister, In accordance with the requirements of regulations under Part 4, Section 18 – Annual Report of the University of South Australia Act 1990, it gives me great pleasure to submit for your information and presentation to Parliament the University of South Australia 2016 Annual Review and the University of South Australia 2016 Financial Statements, for the year ending 31 December 2016. The University Council approved the Annual Review and the Financial Statements at its meeting on 13 April 2017. Yours sincerely, Mr Jim McDowell / Chancellor COMPANION VOLUME The University’s complete annual financial statements for the year ended 31 December 2016, adopted by the University Council are contained in the University of South Australia 2016 Financial Statements, a companion volume to this report. YOUR FEEDBACK We welcome any comments or suggestions on the content or layout of this report. Please contact the Corporate Communications Manager on: Telephone: +618 8302 9136 Email: [email protected] FURTHER INFORMATION This report and the University of South Australia 2016 Financial Statements, as well as past annual reports, are available on our website unisa.edu.au/publications ACKNOWLEDGEMENT OF COUNTRY UniSA respects the Kaurna, Boandik and For hard copies of this report or the University of South Australia Barngarla peoples’ spiritual relationship 2016 Financial Statements, please contact: with their country. We also acknowledge Telephone: +618 8302 0657 the diversity of Aboriginal peoples, past Or write to: and present. -

Florey Medal Gene Therapy Tackles Leading Cause of Blindness in the Elderly
Vision News Autumn 2018 Florey Medal Gene therapy tackles leading cause of blindness in the elderly The pioneering scientist behind a potential new gene therapy treatment for a leading cause of blindness has won national recognition for her work. Professor Elizabeth Rakoczy has been awarded the 2017 CSL Florey Medal for significant lifetime achievement in biomedical science and/or human health advancement. She joins an elite list of past Florey Medallists including Nobel Laureates Barry Marshall and Robin Warren, Ian Frazer and Graeme Clark. Federal Health Minister Greg Hunt congratulates Professor Rakoczy at the Florey Medal presentation Professor Rakoczy, head of the Lions Eye (Photo credit: AAMRI/Brad Cummings Photography) Institute’s Molecular Ophthalmology research group, helped develop a new gene therapy for “The new gene therapy promises to replace wet age-related macular degeneration (wet AMD), monthly injections with a one-off treatment,” which leads to rapid vision loss and affects more Professor Rakoczy said. than 110,000 older Australians. “The gene therapy involves a single injection Wet AMD occurs when there is an overproduction of a modified and harmless version of a virus of the protein vascular endothelial growth factor containing a specific gene that stimulates supply (VEGF) in the retina. VEGF helps support oxygen of a protein which then blocks over-production supply to tissue when circulation is inadequate. of VEGF. The eye becomes a ‘bio-factory’ – When too much VEGF is produced it can cause producing its own treatment for wet AMD.” disease, including blood vessel disease in The gene therapy is not commercially available the eye. -
The-University-Of-Queensland-Not-If-When.Pdf
TOGETHER, OUR GREATEST DAYS LIE AHEAD. Thank you. Not If, When – the Campaign to Message from the Chairs The Not if, when campaign is a partnership between the generous donors in our community who have a dream for Create Change a better world, and UQ, which has the research excellence, resources and people to achieve our donors’ ambitions. We invite you to tell us about your vision for the world, to see if we can help provide you with the tools to achieve it, whether this involves increasing access to education, research, or bolstering the arts and humanities that enrich our lives. What is the campaign? What are the campaign To learn more about how you can Over our 107-year history, the priorities? Our motivation for giving back is simple – we want to make a genuine difference, visit support a community that helped and embraced us. We partnership between donors and UQ The goal of the campaign is to are grateful for the support we received, particularly the gift has had an extraordinary impact on galvanise the community and our uq.edu.au/giving that enabled Ian and Dr Jian Zhou to develop the life-saving our community, Queensland, Australia, alumni to help raise the significant cervical cancer vaccine Gardasil. and the world. funds required for three key priorities: Thank you for considering partnering with us, and for Professor Ian Frazer AC FRS and Mrs Caroline Frazer While we have come a long way, there • Empowering Student Success taking the initiative to support the change that you want to NOT IF, WHEN – THE CAMPAIGN TO CREATE CHANGE CO-CHAIRS is so much more to do and so much through life-changing scholarships, see in the world. -

Calls for Special Australian of the Year Award for Our Nation's Health Workers
Media Release Public Health Association of Australia 29 July 2020 Calls for special Australian of the Year Award for our nation’s health workers As Australia continues to battle our biggest-ever health crisis, The Public Health Association of Australia (PHAA) is calling for the Prime Minister to consider a special one-off award to recognise the life-saving work of our nation’s front-line health care workers and public health workers. Nominations for the 2021 Australian of the Year Awards close this week (Friday 31 July), and each year thousands of worthy individuals are nominated for going above and beyond in their chosen field or pursuits. PHAA CEO, Terry Slevin, says the events of the past six months have demonstrated the incredibly selfless work of the many thousands of people who have turned up for work every day – putting their own lives on the line in many cases – to help save the lives of so many fellow Australians. ‘It is in times like these that we see the best of people. People who dedicate their lives to the wellbeing of others in these times of terrible distress and tragic loss,’ Mr Slevin said. ‘The majority of our health workforce are not highly-paid. Few seek recognition or reward. They make so many personal sacrifices to keep us safe and well. And in the process, many hundreds have themselves succumbed to COVID-19,’ Mr Slevin said. ‘Our public health workers deserve a significant acknowledgement – the tireless work this year by contact tracers, researchers, epidemiologists, outbreak investigators and policy experts has been invaluable. -

Targeting EGFR/ERK/FOS Signaling As a Novel Approach for HPV-Positive Head and Neck Cancer Treatment
PhD degree in Systems Medicine (curriculum in Molecular Oncology) European School of Molecular Medicine (SEMM), University of Milan and University of Naples “Federico II” Settore disciplinare: Bio/11 Targeting EGFR/ERK/FOS signaling as a novel approach for HPV-positive Head and Neck cancer treatment Alessandro Medda European Institute of Oncology (IEO), Milan Tutor: Prof. Susanna Chiocca European Institute of Oncology (IEO), Milan PhD Coordinator: Prof. Giuseppe Viale Anno accademico 2019-2020 Targeting EGFR/ERK/FOS signaling as a novel approach for HPV-positive Head and Neck Cancer Table of contents 1 Abstract ............................................................................................................. 9 2 Introduction ..................................................................................................... 10 2.1 Human Papillomaviruses ................................................................................... 10 2.1.1 Classification ......................................................................................................... 10 2.1.2 Structure and organization .................................................................................... 12 2.1.2.1 Viral Proteins ..................................................................................................... 12 2.1.3 HPV life cycle and infection ................................................................................... 16 2.1.3.1 Viral Attachment and Entry ............................................................................... -

In This Issue: Meet Our 2015 Alumni Award Recipients Women in Science Tribute to the Chancellor CONTACT
FOR ALUMNI AND COMMUNITY SUMMER 2015 In this issue: Meet our 2015 Alumni Award recipients Women in science Tribute to the Chancellor CONTACT CONTACT is produced by the Office of Marketing and Communications and UQ Advancement, The University of Queensland, Brisbane, QLD 4072, Australia Telephone: +61 (0)7 3346 7886 Email: [email protected] Website: uq.edu.au/uqcontact Advertising: Tina Cupitt Email: [email protected] Editorial Board: Shane Rodgers (Chair) – Queensland Editor, The Australian Graham Bethune – Director, Office of Marketing and Communications Colleen Clur – Senior Director, Communications and Engagement, Children’s Health Queensland Doctor John Desmarchelier AM ED – Former General Manager, Sugar Terminals Limited Clare Pullar – Pro-Vice-Chancellor (Advancement) Editors: Prue McMillan and Mark Schroder Project coordinators: Michael Jones and Stacey King Design: Paul Thomas Contributors: Bronwyn Adams, Meredith Anderson, Sally Belford, Renae Bourke, Amanda Briggs, Patricia Danver, Joseph Diskett, Reggie Dutt, Dr Maggie Hardy, Bruce CELEBRATING Ibsen, Fiona Kennedy, Danielle Koopman, Martine Kropkowski, EXCELLENCE Professor Jenny Martin, Dr John Montgomery, Associate Professor Meet the outstanding and inspirational Neil Paulsen, Katrina Shimmin- recipients of The University of Clarke, Professor Maree Smith, John Queensland Alumni Awards 2015. Story AO, Matthew Taylor, Professor Ranjeny Thomas, Evan Williams, 12 Genevieve Worrell. Material in this publication does not necessarily reflect the policies of The University of Queensland. CHANGE OF ADDRESS: + REGULARS + FEATURES Please telephone: +61 (0)7 3346 3900 Facsimile: +61 (0)7 3346 3901 Email: [email protected] UPDATE Printing: DAI Rubicon New Director of Alumni and FOR ALUMNI AND COMMUNITY WINTER 2015 07 LEADING THE WORLD Community Relations PatriciaWITH Danver RESEARCH This product is printed on PEFC BREAKTHROUGHS Ranked well inside the world’s top 100, The University of Queensland (UQ) is one of Australia’s leading teaching discusses strengthening UQ’sand research institutions. -
Timeline of Immunology
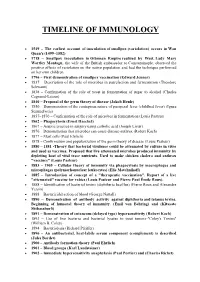
TIMELINE OF IMMUNOLOGY 1549 – The earliest account of inoculation of smallpox (variolation) occurs in Wan Quan's (1499–1582) 1718 – Smallpox inoculation in Ottoman Empire realized by West. Lady Mary Wortley Montagu, the wife of the British ambassador to Constantinople, observed the positive effects of variolation on the native population and had the technique performed on her own children. 1796 – First demonstration of smallpox vaccination (Edward Jenner) 1837 – Description of the role of microbes in putrefaction and fermentation (Theodore Schwann) 1838 – Confirmation of the role of yeast in fermentation of sugar to alcohol (Charles Cagniard-Latour) 1840 – Proposal of the germ theory of disease (Jakob Henle) 1850 – Demonstration of the contagious nature of puerperal fever (childbed fever) (Ignaz Semmelweis) 1857–1870 – Confirmation of the role of microbes in fermentation (Louis Pasteur) 1862 – Phagocytosis (Ernst Haeckel) 1867 – Aseptic practice in surgery using carbolic acid (Joseph Lister) 1876 – Demonstration that microbes can cause disease-anthrax (Robert Koch) 1877 – Mast cells (Paul Ehrlich) 1878 – Confirmation and popularization of the germ theory of disease (Louis Pasteur) 1880 – 1881 -Theory that bacterial virulence could be attenuated by culture in vitro and used as vaccines. Proposed that live attenuated microbes produced immunity by depleting host of vital trace nutrients. Used to make chicken cholera and anthrax "vaccines" (Louis Pasteur) 1883 – 1905 – Cellular theory of immunity via phagocytosis by macrophages and microphages (polymorhonuclear leukocytes) (Elie Metchnikoff) 1885 – Introduction of concept of a "therapeutic vaccination". Report of a live "attenuated" vaccine for rabies (Louis Pasteur and Pierre Paul Émile Roux). 1888 – Identification of bacterial toxins (diphtheria bacillus) (Pierre Roux and Alexandre Yersin) 1888 – Bactericidal action of blood (George Nuttall) 1890 – Demonstration of antibody activity against diphtheria and tetanus toxins. -

Part 4 Australia Today
Australia today In these pages you will learn about what makes this country so special. You will find out more about our culture, Part 4 our innovators and our national identity. In the world today, Australia is a dynamic business and trade partner and a respected global citizen. We value the contribution of new migrants to our country’s constant growth and renewal. Australia today The land Australia is unique in many ways. Of the world’s seven continents, Australia is the only one to be occupied by a single nation. We have the lowest population density in the world, with only two people per square kilometre. Australia is one of the world’s oldest land masses. It is the sixth largest country in the world. It is also the driest inhabited continent, so in most parts of Australia water is a very precious resource. Much of the land has poor soil, with only 6 per cent suitable for agriculture. The dry inland areas are called ‘the Australia is one of the world’s oldest land masses. outback’. There is great respect for people who live and work in these remote and harsh environments. Many of It is the sixth largest country in the world. them have become part of Australian folklore. Because Australia is such a large country, the climate varies in different parts of the continent. There are tropical regions in the north of Australia and deserts in the centre. Further south, the temperatures can change from cool winters with mountain snow, to heatwaves in summer. In addition to the six states and two mainland territories, the Australian Government also administers, as territories, Ashmore and Cartier Islands, Christmas Island, the Cocos (Keeling) Islands, Jervis Bay Territory, the Coral Sea Islands, Heard Island and McDonald Islands in the Australian Antarctic Territory, and Norfolk Island. -
![Cervarix HPV Vaccination Series [1]](https://docslib.b-cdn.net/cover/2061/cervarix-hpv-vaccination-series-1-2382061.webp)
Cervarix HPV Vaccination Series [1]
Published on The Embryo Project Encyclopedia (https://embryo.asu.edu) Cervarix HPV Vaccination Series [1] By: Darby, Alexis Kim, Grace Keywords: Cervarix [2] HPV [3] Papillomavirus [4] Cervical Cancer [5] In 2011, United Kingdom pharmaceutical company GlaxoSmithKline released Cervarix, a vaccination series protecting girls and women from two strains of Human Papillomavirus, or HPV. HPV, a sexually transmitted infection, can present in men and women without symptoms, or may cause symptoms such as genital warts. There is a link between HPV and cervical, vaginal, anal, head, neck, and face cancers, and Cervarix can reduce genital cancers in girls and women, particularly cervical cancer. Gardasil, a similar vaccination against HPV, approved by the United States Food and Drug Administration [6], or FDA, and available in the US in June 2006 was on the market five years prior to Cervarix’s approval in October 2009. In 2014, because of the heightened cost and lesser coverage, the US market discontinued Cervarix, but as of 2020, it remains popular in Europe, especially in the United Kingdom. Cervarix is the first HPV vaccine administered in China. Cervarix protects girls and women from contracting HPV strains sixteen and eighteen linked to eighty percent of cervical cancer instances in women. HPV is a sexually transmitted infection and primarily transmitted through genital contact, infecting the surface level epithelial cells that line organs. People with HPV can experience symptoms such as genital warts, or more commonly, they will not experience any symptoms at all. Some HPV strains are associated with increased risks of cancer, as HPV is an oncogenic [7] virus, meaning it can cause cancer. -

Patent Problem for Australian Professor Ian Frazer • Prana Co
Bi Board Look out for these Upcoming Issues Australia Patent Problem for Australian Professor Ian Frazer Australian scientist Professor Ian Frazer is most well 2006 known as the inventor of the cervical cancer vaccine, which received approval from the US Food and Drug Administration recently and is set to become commercially available in Australia later this year. Drug giant Merck is 30 Aug Drug Discovery already marketing Gardasil to American women on its website. However, there appears to be a patent problem for 15 Sep Special Issue on the cervical cancer vaccine. Biotechnology in Korea The University of Rochester is one of four research institutions claiming to be responsible for original work 30 Sep Pharmacogenomics leading to a cervical cancer vaccine. The other three are the US' National Cancer Institute (NCI), Georgetown 15 Oct Telemedicine University in Washington DC and the University of Queensland. A Georgetown University Medical Center 30 Oct Bioethics (GUMC) press release issued the day the FDA approved Gardasil explained researcher Richard Schlegel's role in the vaccine's development but says nothing about the other 15 Nov Special Issue on Clinical Trials in Asia Pacifi c efforts involved. On the other hand, Ian insists he co-invented the vaccine 30 Nov Lipodomics with University of Queensland colleague Dr Jian Zhou in 1991. Frazer and Zhou fi led a provisional patent covering their human papillomavirus (HPV) research in June 1991 15 Dec Biostatistics and presented their fi ndings at a scientifi c meeting in the US in September -

Networked Knowledge Media Reports Networked Knowledge Kathleen Folbigg Homepage This Page Set up by Dr Robert N Moles [Underlini
Networked Knowledge Media Reports Networked Knowledge Kathleen Folbigg Homepage This page set up by Dr Robert N Moles [Underlining where it occurs is for NetK editorial emphasis] On 4 March 2021 Ellen Whinnett in The Advertiser reported “Scientists want killer pardoned” 76 of Australia’s most respected doctors and scientists have put their names to an extraordinary petition demanding a pardon for Kathleen Folbigg, the mother serving a 30- year jail term for killing four of her infant children. The eminent researchers, including two Nobel laureates and several Australians of the Year, say new medical evidence about a mutant gene carried by two of the Folbigg children creates a “strong presumption’’ they died from natural causes. Pardon mum jailed for killing babies: Joined by another 14 international experts, they have called on NSW Governor Margaret Beazley to pardon Folbigg and immediately release her from jail, calling for an end to the “miscarriage of justice’’ they say the 53-year-old has suffered. Among those to put their names to the petition are Australian Academy of Science president John Shine, Nobel laureate and 1997 Australian of the Year Professor Peter Doherty and Tasmanian-born Emeritus Professor Elizabeth Blackburn, who won the Nobel prize in 2009. Professor Fiona Stanley, 2003 Australian of the Year, and Professor Ian Frazer, 2006 Australian of the Year and co-inventor of the vaccine that prevents cervical cancer, have also signed the scientific consensus statement. “The executive prerogative of mercy is designed to deal with failures of the justice system such as this one,’’ a letter with the petition states.