Investigating the Interactions of Metal Complexes with Heparan Mimetics Wyatt Ohnsonj Virginia Commonwealth University
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

And Cobalt(III): Syntheses, Structures, and Ligand Field Parameters
Inorg. Chem. 2005, 44, 8459−8468 Homoleptic Trimethylsilylacetylide Complexes of Chromium(III), Iron(II), and Cobalt(III): Syntheses, Structures, and Ligand Field Parameters Louise A. Berben and Jeffrey R. Long* Contribution from the Department of Chemistry, UniVersity of California, Berkeley California 94720-1460 Received September 10, 2005 A straightforward method for synthesizing soluble homoleptic trimethylsilylacetylide complexes of first-row transition metal ions is presented. Reaction of anhydrous CrCl2 with an excess of LiCCSiMe3 in THF at −25 °C affords orange Li3[Cr(CCSiMe3)6]‚6THF (1), while analogous reactions employing M(CF3SO3)2 (M ) Fe or Co) generate pale yellow Li4[Fe(CCSiMe3)6]‚4LiCCSiMe3‚4Et2O(2) and colorless Li3[Co(CCSiMe3)6]‚6THF (3). Slightly modified reaction conditions lead to Li8[Cr2O4(CCSiMe3)6]‚6LiCCSiMe3‚4glyme (4), featuring a bis-µ-oxo-bridged binuclear complex, and Li3[Co(CCSiMe3)5(CCH)]‚LiCF3SO3‚8THF (5). The crystal structures of 1−3 show the trimethylsilyl- acetylide complexes to display an octahedral coordination geometry, with M−C distances of 2.077(3), 1.917(7)− 1.935(7), and 1.908(3) Å for M ) CrIII,FeII, and CoIII, respectively, and nearly linear M−CtC angles. The UV− 3- 4 4 visible absorption spectrum of [Cr(CCSiMe3)6] in hexanes exhibits one spin-allowed d−d transition ( T2g r A1g) 4- 3- and three lower-energy spin-forbidden d−d transitions. The spectra of [Fe(CCSiMe3)6] and [Co(CCSiMe3)6] in acetonitrile display high-intensity charge-transfer bands, which obscure all d−d transitions except for the lowest- 1 1 energy spin-allowed band ( T1g r A1g) of the latter complex. -

Point Defects in Lithium Gallate and Gallium Oxide
Air Force Institute of Technology AFIT Scholar Theses and Dissertations Student Graduate Works 8-23-2019 Point Defects in Lithium Gallate and Gallium Oxide Christopher A. Lenyk Follow this and additional works at: https://scholar.afit.edu/etd Part of the Nuclear Engineering Commons Recommended Citation Lenyk, Christopher A., "Point Defects in Lithium Gallate and Gallium Oxide" (2019). Theses and Dissertations. 2369. https://scholar.afit.edu/etd/2369 This Dissertation is brought to you for free and open access by the Student Graduate Works at AFIT Scholar. It has been accepted for inclusion in Theses and Dissertations by an authorized administrator of AFIT Scholar. For more information, please contact [email protected]. POINT DEFECTS IN LITHIUM GALLATE AND GALLIUM OXIDE DISSERTATION Christopher A. Lenyk, Lt Col, USAF AFIT-ENP-DS-19-S-023 DEPARTMENT OF THE AIR FORCE AIR UNIVERSITY AIR FORCE INSTITUTE OF TECHNOLOGY Wright-Patterson Air Force Base, Ohio DISTRIBUTION STATEMENT A. APPROVED FOR PUBLIC RELEASE; DISTRIBUTION UNLIMITED. The views expressed in this document are those of the author and do not reflect the official policy or position of the United States Air Force, the United States Department of Defense or the United States Government. This material is declared a work of the U.S. Government and is not subject to copyright protection in the United States. AFIT-ENP-DS-19-S-023 POINT DEFECTS IN LITHIUM GALLATE AND GALLIUM OXIDE DISSERTATION Presented to the Faculty Graduate School of Engineering and Management Air Force Institute of Technology Air University Air Education and Training Command in Partial Fulfillment of the Requirements for the Degree of Doctor of Philosophy in Nuclear Engineering Christopher A. -

Inorganic Chemistry , 6Th Ed
Chapter 1 8 Interpretation of Spectra In the previous chapter the topic of spectral studies on coordination compounds was introduced only briefl y in connection with ligand fi eld theory, and some of the attendant problems that are associ- ated with interpreting the spectra were described. In this chapter, a more complete description will be presented of the process of interpreting spectra of complexes. It is from the analysis of spectra that we obtain information about energies of spectroscopic states in metal ions and the effects produced by different ligands on the d orbitals. However, it is fi rst necessary to know what spectroscopic states are appropriate for various metal ions. The analysis then progresses to how the spectroscopic states for the metal ions are affected by the presence of the ligands and how ligand fi eld parameters are determined for spectral data. 18.1 SPLITTING OF SPECTROSCOPIC STATES As we have seen, an understanding of spin-orbit coupling is necessary to determine the spectroscopic states that exist for various electron confi gurations, d n (see Section 2.6). Because they will be needed frequently in this chapter, the spectroscopic states that result from spin-orbit coupling in d n ions that have degenerate d orbitals are summarized in Table 18.1 . The spectroscopic states shown in Table 18.1 are those that arise for the so-called free or gaseous ion. When a metal ion is surrounded by ligands in a coordination compound, those ligands generate an electrostatic fi eld that removes the degeneracy of the d orbitals. The result is that eg and t 2g subsets of orbitals are produced. -

The Intensity of Ligand Absorption
Western Kentucky University TopSCHOLAR® Masters Theses & Specialist Projects Graduate School 8-1-1973 The nI tensity of Ligand Absorption Shing-Bong Chen Western Kentucky University Follow this and additional works at: http://digitalcommons.wku.edu/theses Part of the Chemistry Commons Recommended Citation Chen, Shing-Bong, "The nI tensity of Ligand Absorption" (1973). Masters Theses & Specialist Projects. Paper 1018. http://digitalcommons.wku.edu/theses/1018 This Thesis is brought to you for free and open access by TopSCHOLAR®. It has been accepted for inclusion in Masters Theses & Specialist Projects by an authorized administrator of TopSCHOLAR®. For more information, please contact [email protected]. ny THE INTENSITY OF LIGAND ABSORPTION A Thesis Presented to the Faculty of the Department of Chemistry Western Kentucky University Bowling Green, Kentucky in Partial Fulfillment of the Requirements for the Degree Master of Science by Shing-Bong Chen August 1973 THE INTENSITY OP LIGAND ABSORPTION APPROVED (Date) Director of ' TheSIS —— r •Mb >„ fir t-73 :an of the Graduate School ACKNOWLEDGMENT I would like to express gratitude to my research advisor, Dr. Earl F. Pearson, who has given freely of his time and knowledge to show me the way to scientific research. His critical advice and encour- agement are especially appreciated. In addition, I wish to thank the members of the Department of Chemistry of VJestern Kentucky University for their invaluable discussions and suggestions. I also wish to thank Mrs. Linda Moore for typing this thesis. Shing-Bong Chen iii TABLE OP CONTENTS Page ACKNOVJIEDGEJ-'ENTS ±±± LIST OF TABLES v LIST OF FIGURES ; vl ABSTRACT vll INTRDDUCTICN 1 Chapter I. -

Rapid Colorimetric Detection of Cyanide
Zurich Open Repository and Archive University of Zurich Main Library Strickhofstrasse 39 CH-8057 Zurich www.zora.uzh.ch Year: 2012 Rapid Colorimetric Detection of Cyanide Männel-Croisé, Christine Posted at the Zurich Open Repository and Archive, University of Zurich ZORA URL: https://doi.org/10.5167/uzh-74766 Dissertation Published Version Originally published at: Männel-Croisé, Christine. Rapid Colorimetric Detection of Cyanide. 2012, University of Zurich, Faculty of Science. Rapid Colorimetric Detection of Cyanide Dissertation zur Erlangung der naturwissenschaftlichen Doktorwürde (Dr. sc. nat.) vorgelegt der Mathematisch-naturwissenschaftlichen Fakultät der Universität Zürich von Christine Männel-Croisé aus Deutschland Promotionskomitee Prof. Dr. Roger Alberto (Vorsitz) Dr. Felix Zelder (Leitung) Prof. Dr. Roland K. O. Sigel Zürich 2012 Summary iii New strategies for the rapid, straightforward colorimetric detection of cyanide in complex samples with corrin-based chemosensors have been developed. In principle, laboratory equipment is not required. The methods are, therefore, promising for applications by non-expert users for the detection of blood cyanide in emergency situations and for water and food analysis, particularly in tropical countries. Challenges in these situations are posed by the complex sample medium, the low levels of detection and the selectivity of the methods. This thesis presents the first method for the rapid visual detection of blood cyanide using immobilised corrinoids and solid-phase extraction. The result in form of a colour change is obtained within a few minutes using only 1 mL of blood. The semi- quantitative determination of blood cyanide content is achieved by means of a colour chart whereas quantitative determinations are possible by diffuse reflectance spectroscopy or a hand-held spectrophotometer. -
Advanced Inorganic Chemistry ADVANCED INORGANIC CHEMISTRY Diagrams Orgel a Splitting of the Weak Field Dn Ground State Terms in an Octahedral Ligand Field DVANCED
Advanced Inorganic Chemistry ADVANCED INORGANIC CHEMISTRY Diagrams Orgel A Splitting of the weak field dn ground state terms in an octahedral ligand field DVANCED Correlation of spectroscopic terms for dn configuration in O complexes I h NORGANIC om c um er Terms in O At i N b h Term of states Symmetry S 1 A1g P 3 T 1g D 5 T2g + Eg C HEMISTRY F 7 T1g + T2g + A2g Ground state determined by inspection of degeneracy of terms for given dn ADVANCED INORGANIC CHEMISTRY A Orgel Diagrams DVANCED 3 T1g(P) 4 T1g(P) I 3P 3A 4P NORGANIC 2 2g 5 Eg 4 T2g T1g 3 T2g 2 3 4 4 5 D F F T2g D C 2 3 5 HEMISTRY T2g T1g Eg 1 3 ∆o 4 ∆o 2 ∆ d 4 d ∆ d d o A2g o 2 2 T2g E 3 3 g T1g T2g 3 3 T1g A2g 3 3 T1g T1g(P) Ti3+ V2+ Cr3+ Mn3+ A DVANCED The d-d bands of the d2 ion [V(H O) ]3+ 2 6 I NORGANIC C HEMISTRY The Tanabe-Sugano diagram ADVANCED INORGANIC CHEMISTRY A DVANCED Correlation diagrams between energies of atomic and molecular terms can drawn as so-called I NORGANIC Tanabe-Sugano diagrams for each electron configuration of free ions. C HEMISTRY Y. Tanabe, s. Sugano; J. Phys. Soc, Jap., 9, 753 (1954) Energy values in a Tanabe-Sugano diagram are only given relative to the ground state (x-axis). A DVANCED The simple correlation diagram had multiples of B (the Racah parameter) on the energy axis to denote the relative energies of the atomic terms. -
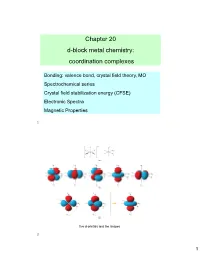
Chapter 20 D-Block Metal Chemistry: Coordination Complexes
Chapter 20 d-block metal chemistry: coordination complexes Bonding: valence bond, crystal field theory, MO Spectrochemical series Crystal field stabilization energy (CFSE) Electronic Spectra Magnetic Properties 1 five d-orbitals and the shapes 2 1 Hybridization schemes for the σ-bonding frameworks of different geometrical configurations 3 Limitations of VB Theory Vacant orbitals available to accept ligand electrons 3d 4s 4p Vacant orbitals available to accept ligand electrons 3d 2 3 Cr(III) d sp 3d d2sp3 Fe(III) For Fe(III), the two d orbitals in the sp3d2 hybrid orbitals would need to be from the 4d orbitals, which is not favorable because the 4d orbitals are much higher in energy than the 3d orbitals. 4 2 Crystal Field Theory (CFT) - - e - - e e e - - e e Mn+ e- e- e- e- - e- ∞ e Mn+ 12 e- rM-L Spherical Shell of e- density at rM-L 5 Crystal Field Stabilization Energy (CFSE) 2 3 3 o 2 o 5 5 6 3 The electronic absorption spectrum 3 of [Ti(OH2)6] in aqueous solution. 3d 7 Values of oct for some d-block metal complexes. 8 4 The trend in values of oct for 3 the complexes [M(NH3)6] where M = Co, Rh, Ir. Field strength increases as one proceeds down a column. oct Mn(II) < Ni(II) < Co(II) < Fe(II) < Cr(III) < Co(III) < Ru(III) < Mo(III) < Rh(III) < Pd(II) < Ir(III) < Pt(IV) 9 Factors affecting the CFSE First, note that the pairing energies for first-row transition metals are relatively constant. -
Tetrahedral Iron in the Active Center of Plant Ferredoxins And
Proc. Nat. Acad. Sci. USA Vol. 68, No. 12, pp. 3015-3020, December 1971 Tetrahedral Iron in the Active Center of Plant Ferredoxins and Beef Adrenodoxin* (iron-sulfur proteins/rubredoxin/near-infrared circular dichroism/ligand-field spectrum/EPR) WILLIAM A. EATONt, GRAHAM PALMERI, JAMES A. FEEt§, TOKUJI KIMURA'[, AND WALTER LOVENBERG11 t Laboratory of Physical Biology, National Institute of Arthritis and Metabolic Diseases, National In- stitutes of Health, Bethesda, Md. 20014; t Biophysics Research Division, Institute of Science and Tech- nology, University of Michigan, Ann Arbor, Mich. 48105; 'I Department of Chemistry, Wayne State University, Detroit, Mich. 48202; and 11 Experimental Therapeutics Branch, National Heart and Lung Institute, National Institutes of Health, Bethesda, Md. 20014 Communicated by Harry B. Gray, September 30, 1971 ABSTRACT The coordination structure of the iron- with a net spin of 2. Recent reviews by Tsibris and Woody sulfur complex in spinach ferredoxin and adrenodoxin is Palmer and have discussed the chem- investigated by optical spectroscopy. The circular-dichro- (6) and Brintzinger (7) ism and absorption spectra of these two-iron iron-sulfur ical, magnetic resonance, magnetic susceptibility, and M6ss- proteins reveal weak electronic transitions in the near- bauer studies, which have all been consistent with this model, infrared wavelength range, 0.8-2.5 ,Am (12,500-4000 cm-l). though no demonstration of the coordination geometry of On the basis of the low absorption intensities and large the iron-sulfur complex was possible. The basis for investigat- anisotropy factors, d d transitions of the iron can be identified in the reduced proteins at about 4000 cm-' and ing this and other aspects of the proposed structure by optical 6000 cm-. -

Inorganic Chemistry SEM VI Sample MCQ’S 1 VBT Can Explain ______Of Transition Metal Complexes
Inorganic Chemistry SEM VI sample MCQ’s 1 VBT can explain _______ of transition metal complexes . Magnetic property Spectral property Reaction mechanism Temperature dependent paramagnetism 2 In octahedral complex, the metal orbitals directly pointed towards the ligand will experience ----. Less repulsion More attraction More repulsion Less attraction 3 The symbol t refers to _____of orbitals Single degeneracy Double degeneracy Triple degeneracy Tetra degeneracy 4 The difference in energy between two sets of d- orbitals in octahedral complexes is denoted by---- ∆t p ∆t ∆sp ∆o 5 In octahedral field, d orbitals split as t2g and e g t1g ande g t2u and e g t1u e g -3 6 The complex [ Fe F6 ] will be ____ in nature. Strongly Paramagnetic Diamagnetic Ferromagnetic Weakly paramagnetic 7 The d-orbitals undergo splitting to a______ in presence of weak field ligands . Greater extent Lesser extent Equal extent Do not split 8 Which of the following is weak field ligand ? F- CN- CO en +3 9 The colour of [ Ti(H2O)6 ] is due to _____transition. Metal to Ligand Charge Transfer Ligand to Metal Charge Transfer d-d f-f 10 Electron – electron repulsions in the ________ complex will be the least. Bromo Iodo Aqua ammine 11 The nephelauxetic effect is minimum in ____complexes. Fluoro Chloro Bromo Iodo 12 The order of increasing energy of d orbital in square planar complex is _________ dxz=dyz< dz2<dxy<dx2-y2 dz2< dx2-y2=dxy <dxz=dyz dxz=dyz> dxy=dx2-y2<dz2 dxz=dyz< dxy=dx2-y2>dz2 +3 13 The magnetic moment of [ Fe (H2O)6] complex is _____ 1.73 B.M 2.82 B. -

Metal-Ligand Bonding
CHAPTER 7 Metal-Ligand Bonding: Limitation of Crystal Field Theory The main drawback of the crystal field theory is that it does not consider the covalent character in metal-ligand bonding at all. It treats the metal-ligand interaction in a purely electrostatic framework which is pretty far from reality. All the effects which originate from covalence cannot be explained by this theory. Therefore, the main limitations of crystal field theory can be concluded only after knowing the causes and magnitude of the covalence in the metal-ligand bonds. Evidences for the Covalent Character in Metal–Ligand Bond The crystal field theory considers the metal center as well as surrounding ligands as point charges and assumes that the interaction between them is 100% ionic. However, quite strong experimental evidences have proved that there is some covalent character too which cannot be ignored. Some of those experimental evidences are as follows: 1. The nephelauxetic effect: The electrons present in the partially filled d-orbitals of the metal center repel each other to produce a number of energy levels. The placement of these levels on the energy scale depends upon the arrangement of filled electrons. The energy of these levels can be given in terms of “Racah parameters” B and C (a measure of interelectronic repulsion). The energy difference between same multiplicity states is expressed in B and Dq while between different multiplicity states is given in term of B, Dq and C. It has been observed that the complexation of metal center always results in a decrease in interelectronic repulsion parameters which in turn also advocates a decrease in the repulsion between d-electron density. -

CH432 Coordination Chemistry คม432 เคมีโคออร์ดิเนชัน
CH432 Coordination Chemistry คม432 เคมีโคออร์ดิเนชัน Weerinradah Tapala (วีรินท์รดา ทะปะละ) Department of Chemistry, Faculty of Science, Maejo University, Chiang Mai, Thailand Course Outline (21.34%) I) Nomenclature of coordination compounds II) Coordinate bond II)Structure and isomer of coordination compounds III)Preparation and reaction of coordination compounds IV)Introduction of supramolecular chemistry and applications References: 1. G.A. Lawrance, Introduction to Coordination Chemistry, John Wiley & Sons Ltd, 2010. 2. P.W. Atkins, T.L. Overton, J.P. Rourke, M.T. Weller, F.A. Armstrong, Shriver and Atkins' Inorganic Chemistry, 5th Edition, W. H. Freeman and Company New York, 2010. 3. G.L. Miessler, D.A. Tarr, Inorganic Chemistry, 3th Edition, Pearson Prentice Hall, 2004. 4. C.E. Housecroft, A.G. Sharpe, Inorganic Chemistry, 2nd Edition, Pearson Prentice Hall, 2005. 5. สุจิตรา ยังมี, เคมีโคออร์ดิเนชัน, 2549. 2 Coordination concept G.A. Lawrance, Introduction to Coordination Chemistry, John Wiley & Sons Ltd, 2010. 3 Metal-Organic Materials (MOMs) 4 Metal-Organic Materials (MOMs) 0-D 5 Metal-Organic Materials (MOMs) 1-D Co(C9H10NO3)(C6H4NO2)(H2O)2 (II) 6 Metal-Organic Materials (MOMs) 2-D 7 Metals 8 Organic ligands Flexibility Carboxylased-based Rigid ligand “Displaying multiple coordination modes” “provide more rigid structures and better structural prediction” Flexibility Flexible ligand “offer a great variety of interesting structures and properties” 9 Applications of MOMs • gas storage • selective gas adsorption • catalysis The outgrowth in numbers of MOMs reported in • luminescent materials Cambridge Structure Database during 1990 to 2011 (B. Yotnoi, D.Phil Thesis, 2012.) Chem. Soc. Rev., 38 (2009) 1213 ,Coord. Chem. Rev. 253 (2009) 3042., Micropor. -
Bonding in Transition Metal Complexes
Bonding in transition metal complexes • Crystal Field Theory (CFT) Assumes electrostatic (ionic) interactions between ligands and metal ions Useful for understanding magnetism and electronic spectra • Valence Bond (VB) Theory Assumes covalent M–L bonds formed by ligand electron donation to empty metal hybrid orbitals. Useful for rationalizing magnetic properties, but cannot account for electronic spectra . Offers little that cannot be covered better by other theories. • Molecular Orbital (MO) Theory Approach using M–L general MOs Excellent quantitative agreement, but less useful in routine qualitative discussions • Ligand Field Theory (LFT) Modified CFT Makes empirical corrections to account for effects of M–L orbital overlap, improving quantitative agreement with observed spectra MO used for most sophisticated and quantitative interpretations LFT used for semi -quantitative interpretations CFT used for everyday qualitative interpretations CFT energies of d orbitals in an Octahedral (O h) Complex • Consider a spherical field equivalent to six electron pairs surrounding a central metal ion, M. • Electron repulsions will perturb the energies of the five degenerate d orbitals , making them rise in energy. • The energies of the t2g orbitals and eg orbitals, however, depend upon their orientation to the six ligand coordination positions in an Oh ligand field. • The eg orbitals have lobes that point at the ligands and so will ascend in energy. • The t2g orbitals have lobes that lie between ligands and so will descend in energy. The energy gap between t 2g and e g levels is designated ∆∆∆o (or 10Dq) • The energy of the eg set rises by +3/5 ∆o (+ 6Dq) while the energy of the t2g set falls by –2/5 ∆o (– 4Dq) resulting in no net energy change for the system.