Bayer Study Synopsis
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-
APEC Port Development Report 2019
2019 APEC Port Development Report 2019 1 2 2018 APEC Port Development Report www.apecpsn.org APEC Port Services Network (APSN) is an international organization established in response to the directives of the 14th APEC Economic Leaders’ Meeting in 2006 and with the support of all leaders from APEC member economies to promote exchanges and cooperation among port and port-related industries in the Asia-Pacific region. The mandate of the APSN is to facilitate trade and investment and enhance supply chain security by strengthening economic cooperation, capacity building, information and personnel exchanges among port and port-related industries and services in the region, so as to achieve the common prosperity of the APEC member economies as a whole. Ever since establishment of APSN, as a complimentary service for port-related industries in the Asia-Pacific region, APEC Port Development Report has published 10 issues. This report focuses on the development of Asia-Pacific ports in 2019, covering trade, ocean shipping, port infrastructure and operation, laws and regulations, intelligent and sustainable development. With its detailed statistics, and in-depth analyses, APEC Port Development Report has become an important reference for those engaging in port-related industries. The APSN secretariat sincerely welcomes your advice, and we hope that ports and organizations can contribute variously valuable information so that we can follow the development of the industry even closer, and provide our readers with more accurate information in a more -

Relics of the Bulgarian National Epic
PAISStt OF HILENDAR: FOUNDER OF THE NATIONAL IDEOLOGY In modern historiography the first centuries of the of the respectful image of Mediaeval Bulgaria. In Sremski Ottoman rule of Bulgarian lands are determined as Late Karlovci, one of the most active literary centres of the Middle Ages. The time from the beginning of the 18th time, Paissi read the book of Dubrovnik Abbot Mavro century to the 1877-1878 Russo-Turkish War is called Orbini "The Realm of the Slavs" in which he discovered Bulgarian National Revival. If the National Revival period considerable evidence about the Bulgarians' past. for Northern Bulgaria and the Sofia Region continued by In 1762 he completed "Slav-Bulgarian History, about 1878, for Eastern Rumelia it was by 1885 and for the People and the Kings, the Bulgarian Saints and All Macedonia and Adrianople Thrace by 1912-1913. Bulgarian Activities and Events". In 83 hand-written The National Revival in the Bulgarian lands witnessed pages the inspired Hilendar Monk interpreted using considerable economic progress. The Bulgarian were romantic and heightened tone the grandour of increasingly getting rid of their mediaeval restricted out- Mediaeval Bulgaria, the victory of the Bulgarian army look and helplessness and were gradually getting aware over Byzantium, the impressive bravery and manliness of as people, aspiring towards economic and cultural the Bulgarians, the historic mission of the Cyril and progress. Hilendar monk Paissii became a mouthpiece of Methodius brothers and other eloquent facts, worthy to these changes in the national self-awareness. He was be remembers and respected by the successors. Already the first to perceive the beginning of the new time and in the forward this noted Bulgarian appealed with gen- the need of formulating verbally the maturing historical uine sincerity towards his compatriots to love and keep prospects and tasks before the Bulgarian people. -

Combined and Uneven Development: Towards a New Theory of World-Literature
Combined and Uneven Development: Towards a New Theory of World-Literature Postcolonialism across the Disciplines 17 Postcolonialism across the Disciplines Series Editors Graham Huggan, University of Leeds Andrew Thompson, University of Exeter Postcolonialism across the Disciplines showcases alternative directions for postcolonial studies. It is in part an attempt to counteract the dominance in colonial and postcolonial studies of one particular discipline – English literary/ cultural studies – and to make the case for a combination of disciplinary knowledges as the basis for contemporary postcolonial critique. Edited by leading scholars, the series aims to be a seminal contribution to the field, spanning the traditional range of disciplines represented in postcolonial studies but also those less acknowledged. It will also embrace new critical paradigms and examine the relationship between the transnational/cultural, the global and the postcolonial. Combined and Uneven Development Towards a New Theory of World-Literature WReC (Warwick Research Collective) Liverpool University Press Warwick Research Collective: Sharae Deckard Nicholas Lawrence Neil Lazarus Graeme Macdonald Upamanyu Pablo Mukherjee Benita Parry Stephen Shapiro First published 2015 by Liverpool University Press 4 Cambridge Street Liverpool L69 7ZU Copyright © Sharae Deckard, Nicholas Lawrence, Neil Lazarus, Graeme Macdonald, Upamanyu Pablo Mukherjee, Benita Parry and Stephen Shapiro The right of Sharae Deckard, Nicholas Lawrence, Neil Lazarus, Graeme Macdonald, Upamanyu Pablo Mukherjee, Benita Parry and Stephen Shapiro to be identified as the authors of this book has been asserted by them in accordance with the Copyright, Design and Patents Act 1988. All rights reserved. No part of this book may be reproduced, stored in a retrieval system, or transmitted, in any form or by any means, electronic, mechanical, photocopying, recording, or otherwise, without the prior written permission of the publisher. -

Abstracts from the 50Th European Society of Human Genetics Conference: Electronic Posters
European Journal of Human Genetics (2019) 26:820–1023 https://doi.org/10.1038/s41431-018-0248-6 ABSTRACT Abstracts from the 50th European Society of Human Genetics Conference: Electronic Posters Copenhagen, Denmark, May 27–30, 2017 Published online: 1 October 2018 © European Society of Human Genetics 2018 The ESHG 2017 marks the 50th Anniversary of the first ESHG Conference which took place in Copenhagen in 1967. Additional information about the event may be found on the conference website: https://2017.eshg.org/ Sponsorship: Publication of this supplement is sponsored by the European Society of Human Genetics. All authors were asked to address any potential bias in their abstract and to declare any competing financial interests. These disclosures are listed at the end of each abstract. Contributions of up to EUR 10 000 (ten thousand euros, or equivalent value in kind) per year per company are considered "modest". Contributions above EUR 10 000 per year are considered "significant". 1234567890();,: 1234567890();,: E-P01 Reproductive Genetics/Prenatal and fetal echocardiography. The molecular karyotyping Genetics revealed a gain in 8p11.22-p23.1 region with a size of 27.2 Mb containing 122 OMIM gene and a loss in 8p23.1- E-P01.02 p23.3 region with a size of 6.8 Mb containing 15 OMIM Prenatal diagnosis in a case of 8p inverted gene. The findings were correlated with 8p inverted dupli- duplication deletion syndrome cation deletion syndrome. Conclusion: Our study empha- sizes the importance of using additional molecular O¨. Kırbıyık, K. M. Erdog˘an, O¨.O¨zer Kaya, B. O¨zyılmaz, cytogenetic methods in clinical follow-up of complex Y. -

Pomagalo Philosophy 9Kl-Eng.Pdf
МИНИСТЕРСТВО НА ОБРАЗОВАНИЕТО И НАУКАТА НАЦИОНАЛНА ПРОГРАМА „Разработване на учебни помагала и на методически ръководства, оценяване и одобряване на проекти на учебни помагала за подпомагане на обучението, организирано в чужбина, на проекти на учебници и на проекти на учебни комплекти“ МОДУЛ „Разработване на учебни помагала за обучение по общообразователни предмети на чужд език“ 9. Философия КЛАС на английски език Учебно помагало Разработено от авторски екип към Профилирана езикова гимназия „Йоан Екзарх“, гр. Враца Национално издателство за образование и наука „Аз-буки“ 2020 г. Dear students, The Student’s book is a secondary level course for learners studying Philosophy in English at CEFR level B1 and the Bulgarian Ministry of Education and Science CURRICULUM – 9th grade. It contains themes corresponding to the curriculum and others, which address philosophy-oriented students. The book contains a variety of theory and practice. The practical tasks aim at developing students’ critical thinking and their positive attitude towards life. The themes relate to interpretation of value system, goal orientation towards the meaning of life and cognition of main ethical and aesthetic categories. It also contains interesting tasks, tests and illustrations. ФИЛОСОФИЯ ЗА 9. КЛАС НА АНГЛИЙСКИ ЕЗИК Учебно помагало, разработено от авторски екип към Профилирана езикова гимназия „Йоан Екзарх“, гр. Враца Автор на текста: Христомила Каменова Благовескова, 2020 г. Преводач: Таня Денова Илиева, 2020 г. Консултант: проф. д.н. Вихрен Янакиев Бузов, 2020 г. Автори на графичния дизайн: Диана Иванова Гергова и Мариета Любенова Иванова, 2020 г. Автори на илюстрациите: Мариета Любенова Иванова, 2020 г. Веселка Пламенова Йорданова, Василена Стоянова Николова, Ева Евгениева Ценкова, Лили Тихомирова Котова, Биляна Цветомирова Добрилова – ученици в ПЕГ „Йоан Екзарх“, 2020 г. -

VASE Studio Portrait of Revolutionaries Belonging to Hristo Botev's
VASE Visual Archive Southeastern Europe Permalink: https://gams.uni-graz.at/o:vase.191 Studio portrait of revolutionaries belonging to Hristo Botev's armed company (cheta) Object: Studio portrait of revolutionaries belonging to Hristo Botev's armed company (cheta) Description: Full length shot of two men wearing military uniforms and fur caps, traditional peasant shoes (tsarvuli), and leggings. They are holding long rifles and swords and are standing between artificial rocks. A painted canvas backdrop is creating the illusion of the scene being set in nature. Comment: On the right: Dimitar Todorov Donkov- Dimitroto (1855 - 1940), who participated Studio portrait of revolutionaries belonging in the military uprising led by Hristo to Hristo Botev's armed company (cheta) Botev. When the revolt was crushed, © National Museum of Military History Sofia Dimitar Todorov Dimitroto was arrested, yet his death sentence was commuted to life imprisonment. Hristo Botev (Botyov) Petkov (1848 - 1876) was a Bulgarian poet and national revolutionary, who died in a uprising against the Ottoman rule in 1876. He is considered a symbolic historical figure and national hero. Relations: https://gams.uni-graz.at/o:vase.480 Date: Not before 1886 Location: Sofia Country: Bulgaria Type: Photograph Creator: Karastoyanov, Dimitar Anastasov, (Photographer) Studio portrait of revolutionaries belonging Dimensions: Artefact: 265mm x 222mm to Hristo Botev's armed company (cheta) © National Museum of Military History Image: 236mm x 183mm Sofia Format: Not specified Technique: Not specified Keywords: 550 Individuation and Mobility > 551 Personal Names 700 Armed Forces 710 Military Technology > 714 Uniform and Accouterment 660 Political Behavior > 669 Revolution 530 Arts > 5310 Verbal Arts https://gams.uni-graz.at/vase 1 VASE Visual Archive Southeastern Europe Permalink: https://gams.uni-graz.at/o:vase.191 Bibliograpy: Kassabova, Anelia (2012): Identities in frame. -

"Shoot the Teacher!": Education and the Roots of the Macedonian Struggle
"SHOOT THE TEACHER!" EDUCATION AND THE ROOTS OF THE MACEDONIAN STRUGGLE Julian Allan Brooks Bachelor of Arts, University of Victoria, 1992 Bachelor of Education, University of British Columbia, 200 1 THESIS SUBMITTED IN PARTIAL FULFILLMENT OF THE REQUIREMENTS FOR THE DEGREE OF MASTER OF ARTS In the Department of History O Julian Allan Brooks 2005 SIMON FRASER UNIVERSITY Fall 2005 All rights reserved. This work may not be reproduced in whole or in part, by photocopy or other means, without permission of the author. APPROVAL Name: Julian Allan Brooks Degree: Master of Arts Title of Thesis: "Shoot the Teacher!" Education and the Roots of the Macedonian Struggle Examining Committee: Chair: Professor Mark Leier Professor of History Professor AndrC Gerolymatos Senior Supervisor Professor of History Professor Nadine Roth Supervisor Assistant Professor of History Professor John Iatrides External Examiner Professor of International Relations Southern Connecticut State University Date Approved: DECLARATION OF PARTIAL COPYRIGHT LICENCE The author, whose copyright is declared on the title page of this work, has granted to Simon Fraser University the right to lend this thesis, project or extended essay to users of the Simon Fraser University Library, and to make partial or single copies only for such users or in response to a request from the library of any other university, or other educational institution, on its own behalf or for one of its users. The author has further granted permission to Simon Fraser University to keep or make a digital copy for use in its circulating collection, and, without changing the content, to translate the thesislproject or extended essays, if technically possible, to any medium or format for the purpose of preservation of the digital work. -

Towards a History of the Literary Cultures in East-Central Europe: Theoretical Reflections
Towards a History of the Literary Cultures in East-Central Europe: Theoretical Reflections Marcel Cornis-Pope John Neubauer American Council of Learned Societies ACLS OCCASIONAL PAPER, No. 52 ISSN 1041-536X Towards a History of the Literary Cultures in East-Central Europe: Theoretical Reflections Marcel Cornis-Pope John Neubauer American Council of Learned Societies ACLS OCCASIONAL PAPER, No. 52 Copyright © 2002 Marcel Cornis-Pope and John Neubauer Towards a History of the Literary Cultures in East-Central Europe: Theoretical Reflections Marcel Cornis-Pope Virginia Commonwealth University John Neubauer University ofAmsterdam Historical approaches to literature and culture have experienced a remarkable revival in the last decades, accompanied by severe critiques of past historiographies. The new approaches reject the positivist and orthodox Marxist traditions that regard literature as a mimetic reflection of an underlying "reality," "internalist" histories that isolate the discipline from the surrounding culture, Hegelian, organicist, and teleological generalizations of periods and cultures, reductive national perspectives, and, last but not least, histories dominated by "grand narratives." But if there is a reasonable consensus on the critique of the past, new histories have been slow in coming and controversial when published. Witness the series that the International Comparative Literature Association (ICLA) has been preparing on the history of literature in the European languages, and the French literary history that Denis Hollier and his collaborators have published-both of which we shall discuss later in this paper. The following essay delineates the contours of an ongoing project on the history of the literary cultures in East-Central Europe, which will be published by John Benjamins Press in three volumes. -
Documentary On
TV FICTION Details of all programmes nominated for PRIX EUROPA 2020 are based on the information provided by the submitting organisation. TV FICTION Programmes in Competition 2020 01 Vienna Blood Austria 02 Blackout Belgium 03 Actor Czech Republic 04 Traitor Estonia 05 Peacemaker Finland 06 Merkel Germany 07 The Turncoat - Part 1 Germany 08 The Windermere Children Germany 09 Unterleuten Germany 10 The Minister Iceland 11 My Brilliant Friend - The Story of a New Name Italy 12 ANNE+Sara The Netherlands 13 Bitch The Netherlands 14 22 July Norway 15 The Butler Poland 16 24 Land – The Spy Portugal 17 Spring on the Last Lake Serbia 18 Quarantine Diaries Spain 19 The Paradise Spain 20 Caliphate Sweden 21 Limboland Sweden 22 Labyrinth of Peace Switzerland 23 No. 47 - Sophie Switzerland 24 Anthony United Kingdom 26 Foodie Love Spain TV FICTION Vienna Blood, Episode 1 Vienna Blood Vienna Blood is set in 1900s Vienna: a hot bed of philosophy, science and art, where a clash of cultures and ideas play out in the city’s grand cafes and opera houses. Max Liebermann is a brilliant young English doctor, studying under the famed psychoanalyst Sigmund Freud. Max is keen to understand the criminal mind and begins to observe Oskar Rheinhardt, a Detective Inspector in the Vienna Police Department, who is struggling with a perplexing case. Max’s extraordinary skills of perception and forensics, and his deep understanding of human behaviour and deviance, help Oskar solve Vienna’s most mysterious cases. In ‘The Last Séance’ Junior doctor Max Liebermann is undertaking research in the new discipline of psychotherapy much to the disgust of his professor. -

“To Get Rid of Turks”. the South-Slavic States and Muslim Remigration in the Turn of 1870S and 1880S1
“TO GET RID OF TURKS”. THE SOUTH-SLAVIC STATES AND MUSLIM REMIGRATION IN THE TURN OF 1870S AND 1880S1 Krzysztof Popek Jagiellonian University in Kraków, Institute of History ORCID ID: 0000-0001-5864-5264 Introduction The Great Eastern Crisis (1875–1878) led to migrations on an in- comparable scale in the Balkan Peninsula. The Russian-Turkish War of 1877–1878 forced about 350,000 Muslims to leave the Bulgarian lands, which we will understand as the area covering the Principality of Bulgaria and Eastern Rumelia. Sanjak of Niš’s occupation by the Serbian Army resulted in the exodus of 71,000 Muslims. After the situation in the region had stabilized, the refugees (so-called Muhajirs) wanted to get back to their homes in the newly created Principality of Bulgaria, autonomous Eastern Rumelia (first controlled by Russians and later by Bulgarians), and the lands annexed by Serbia. The return of war refugees was one of the central problems the South-Slavic states faced in the first years after the Great Eastern Cri- sis. It led to serious complications, which had various reasons. Among the most significant ones was the logistic deployment of the remigrants in the areas often settled by Bulgarians of Macedonia and Thrace, and by Serbians of Kosovo and Montenegro. Another one was diplomatic disputes between the Sublime Porte and the Great Powers, the latter 1 ����������������������������������������������������������������������������������������Research presented in this article was financed by the grant of the Polish National Sci- ence Center: The Balkan Migration Processes in the 19th Century. Cases of Bulgaria and Serbia (2017/25/N/HS3/00576). -

LEONARDO PROJECT – English Summary the Project Main Goal Is
Project national LLP-LdV/PAR/2011/RO//129 number Project title “Introducing standards of the best medical practice for the patients with inherited Alpha-1 Antitrypsin Deficiency in Central Eastern Europe” LEONARDO PROJECT – english summary The project main goal is to support development of Central Eastern European Network (CEE) for Alpha-1 Antytrypsin Deficiency (A1ATD) diagnostics and treatment that will function within AIR (Alpha One International Registry) European network of medical centers specializing in A1ATD. Parteners 1. The National Institute of Tuberculosis and Lung Diseases/ Poland (Coordinator) 2. Hannover Medical School/ Germany 3. Institute of Pneumophtysiology “Marius Nasta”/ Romania 4. PJ Safarik University, Faculty of Medicine/ Slovakia 5. Leiden University Medical Center h/o Academisch Ziekenhuis Leiden/ Netherlands 6. UMHAT “Dr.Georgi Stranski” Pleven EAD, Clinic for pneumonology and phthisiatry"/ Bulgaria 7. Vilnius University Faculty of Medicine/ Lithuania 8. Università degli Studi di Pavia/ Italy The project is designed to address specific CEE regional educational needs, therefore its aims are: • to develop individualized training program for respiratory professionals : physicians, physiotherapists, laboratory staff involved in A1ATD diagnostics and medical care in CEE; program will be tailored according to specific country needs • to develop educational materials for respiratory professionals in national CEE languages • to create awareness of A1ATD problem and patient needs in CEE • to promote A1ATD European network in CEE European countries Project Stages: Stage 1: Central Eastern European Network establishment: assessing local needs and potential to launch close cooperation both regionally as well as within the existing European network (AIR)- workshop Stage 2A: Training visits Stage 2B: Focus group workshops Stage 3A: European network AIR conference in Warsaw Stage 3B: Educational materials for respiratory professionals and dissemination of results . -
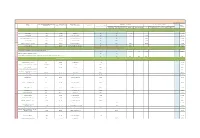
L Shire 2020 Disclosure Report ENG 21 June.Xlsx
Date of publication: 2021-06-21 HCPs: City of Principal Practice HCOs: city Unique country identifier Full Name Country of Principal Practice Principal Practice Address Contribution to costs of Events Fee for service and consultancy where registered OPTIONAL TOTAL Donations and Grants to HCOs Sponsorship agreements with HCOs / third parties Related expenses agreed in the fee for service or consultancy contract, OPTIONAL Registration Fees Travel & Accomodation Fees appointed by HCOs to manage an Event including travel & accomodation relevant to the contract INDIVIDUAL NAMED DISCLOSURE - one line per HCP (i.e. all transfers of value during a year for an individual HCP will be summed up: itemization should be available for the individual Recipient or public authorities' consultation only, as appropriate) Atanas Banchev Sofia Bulgaria Byalo More 8 N/A N/A 1,706.00 1,706.00 Анна Валериева София Bulgaria ул.Св.Георги Софийски 1 N/A N/A 176.02 5,307.00 5,483.02 Даниела Мирчева Авджиева Тзавелла София Bulgaria ул.Свето Преображение 20 N/A N/A 1,024.00 1,024.00 Емил Паскалев София Bulgaria ул.Св.Георги Софийски 1 N/A N/A 1,173.00 1,173.00 HCPs Мария Тончева Стаевска Коташева София Bulgaria ул.Св.Георги Софийски 1 N/A N/A 176.02 1,227.00 1,403.02 Мила Жекова Байчева София Bulgaria бул.Акад.Иван Евстратиев Гешов 11 N/A N/A 352.05 352.05 OTHER, NOT INCLUDED ABOVE - where information cannot be disclosed on an individual basis for legal reasons Aggregate amount attributable to transfers of value to such Recipients - Art.