Skin and Soft Tissue Infections Following Marine Injuries
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

WO 2014/134709 Al 12 September 2014 (12.09.2014) P O P C T
(12) INTERNATIONAL APPLICATION PUBLISHED UNDER THE PATENT COOPERATION TREATY (PCT) (19) World Intellectual Property Organization International Bureau (10) International Publication Number (43) International Publication Date WO 2014/134709 Al 12 September 2014 (12.09.2014) P O P C T (51) International Patent Classification: (81) Designated States (unless otherwise indicated, for every A61K 31/05 (2006.01) A61P 31/02 (2006.01) kind of national protection available): AE, AG, AL, AM, AO, AT, AU, AZ, BA, BB, BG, BH, BN, BR, BW, BY, (21) International Application Number: BZ, CA, CH, CL, CN, CO, CR, CU, CZ, DE, DK, DM, PCT/CA20 14/000 174 DO, DZ, EC, EE, EG, ES, FI, GB, GD, GE, GH, GM, GT, (22) International Filing Date: HN, HR, HU, ID, IL, IN, IR, IS, JP, KE, KG, KN, KP, KR, 4 March 2014 (04.03.2014) KZ, LA, LC, LK, LR, LS, LT, LU, LY, MA, MD, ME, MG, MK, MN, MW, MX, MY, MZ, NA, NG, NI, NO, NZ, (25) Filing Language: English OM, PA, PE, PG, PH, PL, PT, QA, RO, RS, RU, RW, SA, (26) Publication Language: English SC, SD, SE, SG, SK, SL, SM, ST, SV, SY, TH, TJ, TM, TN, TR, TT, TZ, UA, UG, US, UZ, VC, VN, ZA, ZM, (30) Priority Data: ZW. 13/790,91 1 8 March 2013 (08.03.2013) US (84) Designated States (unless otherwise indicated, for every (71) Applicant: LABORATOIRE M2 [CA/CA]; 4005-A, rue kind of regional protection available): ARIPO (BW, GH, de la Garlock, Sherbrooke, Quebec J1L 1W9 (CA). GM, KE, LR, LS, MW, MZ, NA, RW, SD, SL, SZ, TZ, UG, ZM, ZW), Eurasian (AM, AZ, BY, KG, KZ, RU, TJ, (72) Inventors: LEMIRE, Gaetan; 6505, rue de la fougere, TM), European (AL, AT, BE, BG, CH, CY, CZ, DE, DK, Sherbrooke, Quebec JIN 3W3 (CA). -

WO 2013/042140 A4 28 March 2013 (28.03.2013) P O P C T
(12) INTERNATIONAL APPLICATION PUBLISHED UNDER THE PATENT COOPERATION TREATY (PCT) (19) World Intellectual Property Organization International Bureau (10) International Publication Number (43) International Publication Date WO 2013/042140 A4 28 March 2013 (28.03.2013) P O P C T (51) International Patent Classification: NO, NZ, OM, PA, PE, PG, PH, PL, PT, QA, RO, RS, RU, A61K 31/197 (2006.01) A61K 45/06 (2006.01) RW, SC, SD, SE, SG, SK, SL, SM, ST, SV, SY, TH, TJ, A61K 31/60 (2006.01) A61P 31/00 (2006.01) TM, TN, TR, TT, TZ, UA, UG, US, UZ, VC, VN, ZA, A61K 33/22 (2006.01) ZM, ZW. (21) International Application Number: (84) Designated States (unless otherwise indicated, for every PCT/IN20 12/000634 kind of regional protection available): ARIPO (BW, GH, GM, KE, LR, LS, MW, MZ, NA, RW, SD, SL, SZ, TZ, (22) International Filing Date UG, ZM, ZW), Eurasian (AM, AZ, BY, KG, KZ, RU, TJ, 24 September 2012 (24.09.2012) TM), European (AL, AT, BE, BG, CH, CY, CZ, DE, DK, (25) Filing Language: English EE, ES, FI, FR, GB, GR, HR, HU, IE, IS, IT, LT, LU, LV, MC, MK, MT, NL, NO, PL, PT, RO, RS, SE, SI, SK, SM, (26) Publication Language: English TR), OAPI (BF, BJ, CF, CG, CI, CM, GA, GN, GQ, GW, (30) Priority Data: ML, MR, NE, SN, TD, TG). 2792/DEL/201 1 23 September 201 1 (23.09.201 1) IN Declarations under Rule 4.17 : (72) Inventor; and — of inventorship (Rule 4.17(iv)) (71) Applicant : CHAUDHARY, Manu [IN/IN]; 51-52, In dustrial Area Phase- 1, Panchkula 1341 13 (IN). -

SNF Mobility Model: ICD-10 HCC Crosswalk, V. 3.0.1
The mapping below corresponds to NQF #2634 and NQF #2636. HCC # ICD-10 Code ICD-10 Code Category This is a filter ceThis is a filter cellThis is a filter cell 3 A0101 Typhoid meningitis 3 A0221 Salmonella meningitis 3 A066 Amebic brain abscess 3 A170 Tuberculous meningitis 3 A171 Meningeal tuberculoma 3 A1781 Tuberculoma of brain and spinal cord 3 A1782 Tuberculous meningoencephalitis 3 A1783 Tuberculous neuritis 3 A1789 Other tuberculosis of nervous system 3 A179 Tuberculosis of nervous system, unspecified 3 A203 Plague meningitis 3 A2781 Aseptic meningitis in leptospirosis 3 A3211 Listerial meningitis 3 A3212 Listerial meningoencephalitis 3 A34 Obstetrical tetanus 3 A35 Other tetanus 3 A390 Meningococcal meningitis 3 A3981 Meningococcal encephalitis 3 A4281 Actinomycotic meningitis 3 A4282 Actinomycotic encephalitis 3 A5040 Late congenital neurosyphilis, unspecified 3 A5041 Late congenital syphilitic meningitis 3 A5042 Late congenital syphilitic encephalitis 3 A5043 Late congenital syphilitic polyneuropathy 3 A5044 Late congenital syphilitic optic nerve atrophy 3 A5045 Juvenile general paresis 3 A5049 Other late congenital neurosyphilis 3 A5141 Secondary syphilitic meningitis 3 A5210 Symptomatic neurosyphilis, unspecified 3 A5211 Tabes dorsalis 3 A5212 Other cerebrospinal syphilis 3 A5213 Late syphilitic meningitis 3 A5214 Late syphilitic encephalitis 3 A5215 Late syphilitic neuropathy 3 A5216 Charcot's arthropathy (tabetic) 3 A5217 General paresis 3 A5219 Other symptomatic neurosyphilis 3 A522 Asymptomatic neurosyphilis 3 A523 Neurosyphilis, -

CHAPTER E16 Atlas of Skin Manifestations of Internal Disease CHAPTER E16 Thomas J
CHAPTER e16 Atlas of Skin Manifestations of Internal Disease CHAPTER e16 Thomas J. Lawley Robert A. Swerlick In the practice of medicine, virtually every clinician encounters patients with skin disease. Physicians of all specialties face the daily task of determining the nature and clinical implication of dermatologic disease. In patients with skin eruptions and rashes, the physician must confront the question of whether the cutaneous Atlas of Skin Manifestations Internal Disease process is confined to the skin, representing a pure dermatologic event, or whether it is a manifestation of internal disease relating to the patient’s overall medical condition. Evaluation and accurate diagnosis of skin lesions are also critical given the marked rise in both melanoma and nonmelanoma skin cancer. Dermatologic conditions can be classified and categorized in many different ways, Figure e16-2 Acne rosacea with prominent facial erythema, telangiecta- and in this Atlas, a selected group of inflammatory skin eruptions sias, scattered papules, and small pustules. (Courtesy of Robert Swerlick, and neoplastic conditions are grouped in the following manner: MD; with permission.) (A) common skin diseases and lesions, (B) nonmelanoma skin cancer, (C) melanoma and pigmented lesions, (D) infectious dis- ease and the skin, (E) immunologically mediated skin disease, and (F) skin manifestations of internal disease. COMMON SKIN DISEASES AND LESIONS ( Figs. e16-1 to e16-19) In this section, several common inflamma- tory skin diseases and benign neoplastic and reactive lesions are presented. While most of these dermatoses usually present as a pre- dominantly dermatologic process, underlying systemic associations may be made in some settings. Atopic dermatitis is often present in patients with an atopic diathesis, including asthma and sinusitis. -
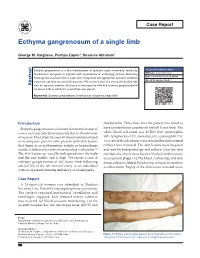
Ecthyma Gangrenosum of a Single Limb
Case Report Ecthyma gangrenosum of a single limb George M. Varghese, Pushpa Eapen1, Susanne Abraham1 Ecthyma gangrenosum is a skin manifestation of systemic sepsis commonly caused by Access this article online Pseudomonas aeruginosa in patients with neutropenia or underlying immune deficiency. Website: www.ijccm.org Although the usual outcome is poor, early recognition and appropriate systemic antibiotic DOI: 10.4103/0972-5229.84898 treatment can lead to successful outcome. We report a case of a previously healthy lady Quick Response Code: Abstract with no apparent immune deficiency or neutropenia who had ecthyma gangrenosum of left lower limb in which the arterial line was placed. Keywords: Ecthyma gangrenosum, Pseudomonas aeruginosa, single limb Introduction thachycardia. Three days later the patient was noted to Ecthyma gangrenosum is a known skin manifestation of have erythematous papules on the left lower limb. The 3 severe systemic infection commonly due to Pseudomonas white blood cell count was 16,500/mm (neutrophils aeruginosa. Most often it is seen in immunocompromised 84%, lymphocytes 12%, monocytes 3%, eosinophils 1%). or neutropenic patients who present with skin lesions Two sets of blood cultures were sent and the intra-arterial that begin as an erythematous nodule or hemorrhagic catheter was removed. The skin lesions were biopsied vesicle, which evolves into a necrotic ulcer with eschar. [1] and sent for histopathology and culture. Over the next The skin lesions are usually widespread over the body few days the skin lesions became blackish with necrotic and the case fatality rate is high. We report a case of areas (arrow) [Figure 1]. The blood, catheter tip, and skin ecthyma gangrenosum of left lower limb following lesion cultures yielded Pseudomonas aeruginosa sensitive arterial line in the left femoral artery in an individual to ceftazidime. -

Cutaneous Manifestations of Infection in the Immunocompromised Host
Cutaneous Manifestations of Infection in the Immunocompromised Host Marc E. Grossman • Lindy P. Fox • Carrie Kovarik Misha Rosenbach Cutaneous Manifestations of Infection in the Immunocompromised Host Second Edition Authors Marc E. Grossman, M.D. Carrie Kovarik, M.D. Professor of Clinical Dermatology Assistant Professor of Dermatology College of Physicians and Surgeons Dermatopathology, and Infectious Diseases Director, Hospital Consultation Service University of Pennsylvania New York Presbyterian Hospital Philadelphia, Pennsylvania, USA Columbia University Medical Center New York, New York, USA Misha Rosenbach, M.D. Assistant Professor of Dermatology Lindy P. Fox, M.D. and Internal Medicine Associate Professor of Clinical Dermatology Director, Dermatology Inpatient Consult Service Director, Hospital Consultation Service University of Pennsylvania University of California, San Francisco Philadelphia, Pennsylvania, USA San Francisco, California, USA ISBN 978-1-4419-1577-1 e-ISBN 978-1-4419-1578-8 DOI 10.1007/978-1-4419-1578-8 Springer New York Dordrecht Heidelberg London Library of Congress Control Number: 2011933837 Springer Science+Business Media, LLC 2012 All rights reserved. Th is work may not be translated or copied in whole or in part without the written permission of the publisher (Springer Science+Business Media, LLC, 233 Spring Street, New York, NY 10013, USA), except for brief excerpts in connection with reviews or scholarly analysis. Use in connection with any form of information storage and retrieval, electronic adaptation, computer software, or by similar or dissimilar methodology now known or hereafter devel- oped is forbidden. Th e use in this publication of trade names, trademarks, service marks, and similar terms, even if they are not identifi ed as such, is not to be taken as an expression of opinion as to whether or not they are subject to proprietary rights. -

Investigation of Swabs from Skin and Superficial Soft Tissue Infections
UK Standards for Microbiology Investigations Investigation of swabs from skin and superficial soft tissue infections Issued by the Standards Unit, Microbiology Services, PHE Bacteriology | B 11 | Issue no: 6.5 | Issue date: 19.12.18 | Page: 1 of 37 © Crown copyright 2018 Investigation of swabs from skin and superficial soft tissue infections Acknowledgments UK Standards for Microbiology Investigations (SMIs) are developed under the auspices of Public Health England (PHE) working in partnership with the National Health Service (NHS), Public Health Wales and with the professional organisations whose logos are displayed below and listed on the website https://www.gov.uk/uk- standards-for-microbiology-investigations-smi-quality-and-consistency-in-clinical- laboratories. SMIs are developed, reviewed and revised by various working groups which are overseen by a steering committee (see https://www.gov.uk/government/groups/standards-for-microbiology-investigations- steering-committee). The contributions of many individuals in clinical, specialist and reference laboratories who have provided information and comments during the development of this document are acknowledged. We are grateful to the medical editors for editing the medical content. For further information please contact us at: Standards Unit Microbiology Services Public Health England 61 Colindale Avenue London NW9 5EQ E-mail: [email protected] Website: https://www.gov.uk/uk-standards-for-microbiology-investigations-smi-quality- and-consistency-in-clinical-laboratories PHE publications gateway number: 2016056 UK Standards for Microbiology Investigations are produced in association with: Logos correct at time of publishing. Bacteriology | B 11 | Issue no: 6.5 | Issue date: 19.12.18 | Page: 2 of 37 UK Standards for Microbiology Investigations | Issued by the Standards Unit, Public Health England Investigation of swabs from skin and superficial soft tissue infections Contents Acknowledgments ................................................................................................................ -
Dermatology in the ER
DRUG ERUPTIONS and OTHER DISORDERS Lloyd J. Cleaver D.O. , F.A.O.C.D, F.A.A.D. Professor of Dermatology ATSU-Kirksville College of Osteopathic Medicine INTERNAL MEDICINE BOARD REVIEW COURSE I Disclosures No Relevant Financial Relationships DRUG ERUPTIONS Drug Reactions 3 things you need to know 1. Type of drug reaction 2. Statistics What drugs are most likely to cause that type of reaction? 3. Timing How long after the drug was started did the reaction begin? Clinical Pearls Drug eruptions are extremely common Tend to be generalized/symmetric Maculopapular/morbilliform are most common Best Intervention: Stop the Drug! Do not dose reduce Completely remove the exposure How to spot the culprit? Drug started within days to a week prior to rash Can be difficult and take time Tip: can generally exclude all drugs started after onset of rash Drug eruptions can continue for 1-2 weeks after stopping culprit drug LITT’s drug eruption database Drug Eruptions Skin is one of the most common targets for drug reactions Antibiotics and anticonvulsants are most common 1-5% of patients 2% of all drug eruptions are “serious” TEN, DRESS More common in adult females and boys < 3 y/o Not all drugs cause eruptions at same rate: Aminopenicillins: 1.2-8% of exposures TMP-SMX: 2.8-3.7% NSAIDs: 1 in 200 Lamotrigine: 10% Drug Eruptions Three basic rules 1. Stop any unnecessary medications 2. Ask about non-prescription medications Eye drops, suppositories, implants, injections, patches, vitamin and health supplements, friend’s medications -

Abdominal Distension, 284 Abdominal Mass, Hydatid Disease, 287
Cambridge University Press 978-0-521-69761-3 - Case Studies in Pediatric Infectious Diseases Frank E. Berkowitz Index More information Index Abdominal distension, 284 perivenous, 240 Abdominal mass, hydatid disease, psoas 287 tuberculosis, 226 Abdominal pain, 12, 79, 112, 158, 169, 177, retropharyngeal, 100, 264, 318 257, 270, 273, 304, 308 tuberculosis, 226 acute HIV infection, 311 spinal epidural, 273 appendicitis, 253 spinal cat-scratch disease, 143 paraplegia, 262 hydatid disease, 287 subphrenic, 232 leptospirosis, 139 tubo-ovarian, 322 pelvic inflammatory disease, 319 Absidia, taxonomy, 347 peritonitis, 315 Acanthameba, taxonomy, 348 pneumonia, 248 Acetaminophen, 15, 54 pyelonephritis, 244 Acetylcholine, 129 typhus, 149 Acid-fast bacilli See Mycobacteria Abdominal tenderness, 257 Acidosis, diarrhea, 80 Abscess Acinetobacter, taxonomy, 342 appendix, 159, 255 Acquired immunodeficiency syndrome, 146, brain, 43, 66, 255 193, 210, 242 meningitis, 108 reportable, 336 seizure, 195 Actinobacillus actinomycetemcomitans, 153 Brodie’s, 282 taxonomy, 343 cerebellar, 327 infective endocarditis, 297 dental, 271 Actinomyces, 124, 127 epidural, 334 taxonomy, 344 eye, 314 Actinomyces israelii, 125 lateral pharyngeal, 264 Actinomyces odontolyticus, taxonomy, liver, 13, 174 344 amebic, 174 Actinomycosis, 125 lung, 249 Acute chest syndrome, sickle cell disease, 249, odontogenic See Abscess 324 dental Acyclovir, 42 pelvic, 306 Epstein–Barr virus, 39 peritonsillar, 100, 264 herpes simplex virus, 29 Lemierre syndrome, 332 varicella, 47 355 © Cambridge University -

Dermatological Indications of Disease - Part II This Patient on Dialysis Is Showing: A
“Cutaneous Manifestations of Disease” ACOI - Las Vegas FR Darrow, DO, MACOI Burrell College of Osteopathic Medicine This 56 year old man has a history of headaches, jaw claudication and recent onset of blindness in his left eye. Sed rate is 110. He has: A. Ergot poisoning. B. Cholesterol emboli. C. Temporal arteritis. D. Scleroderma. E. Mucormycosis. Varicella associated. GCA complex = Cranial arteritis; Aortic arch syndrome; Fever/wasting syndrome (FUO); Polymyalgia rheumatica. This patient missed his vaccine due at age: A. 45 B. 50 C. 55 D. 60 E. 65 He must see a (an): A. neurologist. B. opthalmologist. C. cardiologist. D. gastroenterologist. E. surgeon. Medscape This 60 y/o male patient would most likely have which of the following as a pathogen? A. Pseudomonas B. Group B streptococcus* C. Listeria D. Pneumococcus E. Staphylococcus epidermidis This skin condition, erysipelas, may rarely lead to septicemia, thrombophlebitis, septic arthritis, osteomyelitis, and endocarditis. Involves the lymphatics with scarring and chronic lymphedema. *more likely pyogenes/beta hemolytic Streptococcus This patient is susceptible to: A. psoriasis. B. rheumatic fever. C. vasculitis. D. Celiac disease E. membranoproliferative glomerulonephritis. Also susceptible to PSGN and scarlet fever and reactive arthritis. Culture if MRSA suspected. This patient has antithyroid antibodies. This is: • A. alopecia areata. • B. psoriasis. • C. tinea. • D. lichen planus. • E. syphilis. Search for Hashimoto’s or Addison’s or other B8, Q2, Q3, DRB1, DR3, DR4, DR8 diseases. This patient who works in the electronics industry presents with paresthesias, abdominal pain, fingernail changes, and the below findings. He may well have poisoning from : A. lead. B. -

Connubial Ecthyma Gangrenosum in a Healthy Couple: a Consort Counterpart of a “Kissing Ulcer”
Acta Dermatovenerologica 2015;24:11-12 Acta Dermatovenerol APA Alpina, Pannonica et Adriatica doi: 10.15570/actaapa.2015.4 Connubial ecthyma gangrenosum in a healthy couple: a consort counterpart of a “kissing ulcer” Miloš D. Pavlović1 ✉, Metka Adamič1 Abstract Ecthyma gangrenosum is a relatively rare cutaneous infection generally thought to be linked to sepsis or bacteremia caused by Pseudomonas aeruginosa in severely ill or otherwise immunocompromised patients. Here we report on a healthy middle-aged couple with a typical ecthyma gangrenosum lesion on their thighs, obviously caused by spreading through intimate contact be- tween two skin surfaces: a sort of “consort kissing ulcer.” Although they declined to allow microbiological sampling, the lesions gradually but completely regressed with oral ciprofloxacin treatment, leaving atrophic scars. Keywords: case report, skin infection, ecthyma gangrenosum Received: 1 December 2014 | Returned for modification: 22 December 2014 | Accepted: 12 January 2015 Introduction Case report Ecthyma gangrenosum is a rare cutaneous infection, most com- A 49-year-old woman and her 53-year-old partner came to our der- monly caused by the Gram-negative bacterium Pseudomonas aer- matology center for an extremely painful red and ulcerated plaque uginosa (1, 2). It typically starts with an erythematous or purpuric on their thighs. The lesions appeared in both of them roughly si- macule and rapidly develops into a hemorrhagic bulla or pustule multaneously 2 to 3 weeks prior to presentation as a small reddish surrounded by a narrow pink to violaceous halo. Then it ruptures macule that evolved into a hemorrhagic bulla that ruptured and to become a round ulcer with a necrotic black or a gunmetal-gray transformed into an enlarging ulcer. -
Fever and Rash in the Non-HIV Immunocompromised Host
Anna Skiada University of Athens © by author ESCMID Online Lecture Library >20% of immunocompromised hosts will develop skin lesions, often with fever Multiple defects in host defense lead to different types of infection These lesions may reflect disseminated infection © by author Evaluation of the skin may provide the most ESCMIDrapid diagnosis Online Lecture Library 1. Presence of signs and symptoms other than the rash 2. Recognize the clinical settings: 1. Constructions near the hospital leads to suspicion of aspergillosis or mucormycosis 2. Cellulitis or hemorrhagic bullae in an acute febrile illness after© by exposure author to a salt water environment suggests Vibrio vulnificus ESCMID3. Fresh water Online contamination Lecture implicates Library Aeromonas. M.E. Grossman et al., Cutaneous Manifestations of Infection in the Immunocompromised Host 3. Determine the host factors that predispose to certain infections: diabetic ketoacidosis, organ transplantation, acute leukemia, etc. 4. Timing of the skin lesions: in a patient who has had neutropenia for 3 days, bacterial infection is more© probableby author than fungal infection. ESCMID Online Lecture Library 5. In the neutropenic patient, the classic findings of swelling and fluctuance may be absent. There may be scant or no pus. 6. Determine the host factors that predispose to certain infections: diabetic ketoacidosis, organ transplantation, acute leukemia, etc. 7. Don’t exclude pathogens as “contaminants” 8. Inquire about geographic, nosocomial, occupational, or© behavioral by author exposures 9. History of travel and exposure to animals ESCMID Online Lecture Library 10. Skin biopsy should be performed for histology and culture to establish a definitive diagnosis. © by author ESCMID Online Lecture Library Bacterial infections .