329 Abscesses, 17, 189. See Also Carbuncles
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Smelly Foot Rash
CLINICAL Smelly foot rash Paulo Morais Ligia Peralta Keywords: skin diseases, infectious Case study A previously healthy Caucasian girl, 6 years of age, presented with pruritic rash on both heels of 6 months duration. The lesions appeared as multiple depressions 1–2 mm in diameter that progressively increased in size. There was no history of trauma or insect bite. She reported local pain when walking, worse with moisture and wearing sneakers. On examination, multiple small crater- like depressions were present, some Figure 1. Heel of patient coalescing into a larger lesion on both heels (Figure 1). There was an unpleasant ‘cheesy’ protective/occluded footwear for prolonged odour and a moist appearance. Wood lamp periods.1–4 examination and potassium hydroxide testing for fungal hyphae were negative. Answer 2 Question 1 Pitted keratolysis is frequently seen during What is the diagnosis? summer and rainy seasons, particularly in tropical regions, although it occurs Question 2 worldwide.1,3,4 It is caused by Kytococcus What causes this condition? sedentarius, Dermatophilus congolensis, or species of Corynebacterium, Actinomyces or Question 3 Streptomyces.1–4 Under favourable conditions How would you confirm the diagnosis? (ie. hyperhidrosis, prolonged occlusion and increased skin surface pH), these bacteria Question 4 proliferate and produce proteinases that destroy What are the differential diagnoses? the stratum corneum, creating pits. Sulphur containing compounds produced by the bacteria Question 5 cause the characteristic malodor. What is your management strategy? Answer 3 Answer 1 Pitted keratolysis is usually a clinical Based on the typical clinical picture and the negative diagnosis with typical hyperhidrosis, malodor ancillary tests, the diagnosis of pitted keratolysis (PK) (bromhidrosis) and occasionally, tenderness, is likely. -

What Certified Athletic Trainers and Therapists Need to Know Thomas M
PHYSICIAN PERSPECTIVE Tracy Ray, MD, Column Editor Sports Dermatology: What Certified Athletic Trainers and Therapists Need to Know Thomas M. Dougherty, MD • American Sports Medicine Institute, Birmingham AL OST SPECIAL SKIN problems of athletes are ting shoes for all athletes and gloves for weight lifters M easily observable and can be recognized and racket-sport players can help. and treated early. Proper care can prevent Occlusive folliculitis, also known as acne mechanica disruption of the training or competition schedule. or “football acne,” is a flare of sometimes preexisting Various athletic settings expose the skin to a multi- acne caused by heat, occlusion, and pressure distrib- tude of infectious organisms while increasing its vul- uted in areas under bulky playing equipment (e.g., nerability to infection. A working knowledge of skin shoulders, forehead, chin in football players; legs, arms, disorders in athletes is essential for athletic trainers, trunk in wrestlers). Inflammatory papules and pustules who are often the first to evaluate athletes for medi- are present. A clean absorbent T-shirt should be worn cal problems. under equipment, and the affected areas should be cleansed after a workout. Direct Cutaneous Injury Follicular keloidalis is seen mostly in African-Ameri- can athletes and is a progression of occlusive folliculi- Calluses are the skin’s compensatory, protective re- tis with nontender, firm, fibrous papules around the sponse to friction, most commonly seen on the feet edges of the football helmet, especially at the posterior but also on the hands of golfers and in oar and racket neck and occipital scalp. Surgical treatment, if indicated, sports. -

WO 2014/134709 Al 12 September 2014 (12.09.2014) P O P C T
(12) INTERNATIONAL APPLICATION PUBLISHED UNDER THE PATENT COOPERATION TREATY (PCT) (19) World Intellectual Property Organization International Bureau (10) International Publication Number (43) International Publication Date WO 2014/134709 Al 12 September 2014 (12.09.2014) P O P C T (51) International Patent Classification: (81) Designated States (unless otherwise indicated, for every A61K 31/05 (2006.01) A61P 31/02 (2006.01) kind of national protection available): AE, AG, AL, AM, AO, AT, AU, AZ, BA, BB, BG, BH, BN, BR, BW, BY, (21) International Application Number: BZ, CA, CH, CL, CN, CO, CR, CU, CZ, DE, DK, DM, PCT/CA20 14/000 174 DO, DZ, EC, EE, EG, ES, FI, GB, GD, GE, GH, GM, GT, (22) International Filing Date: HN, HR, HU, ID, IL, IN, IR, IS, JP, KE, KG, KN, KP, KR, 4 March 2014 (04.03.2014) KZ, LA, LC, LK, LR, LS, LT, LU, LY, MA, MD, ME, MG, MK, MN, MW, MX, MY, MZ, NA, NG, NI, NO, NZ, (25) Filing Language: English OM, PA, PE, PG, PH, PL, PT, QA, RO, RS, RU, RW, SA, (26) Publication Language: English SC, SD, SE, SG, SK, SL, SM, ST, SV, SY, TH, TJ, TM, TN, TR, TT, TZ, UA, UG, US, UZ, VC, VN, ZA, ZM, (30) Priority Data: ZW. 13/790,91 1 8 March 2013 (08.03.2013) US (84) Designated States (unless otherwise indicated, for every (71) Applicant: LABORATOIRE M2 [CA/CA]; 4005-A, rue kind of regional protection available): ARIPO (BW, GH, de la Garlock, Sherbrooke, Quebec J1L 1W9 (CA). GM, KE, LR, LS, MW, MZ, NA, RW, SD, SL, SZ, TZ, UG, ZM, ZW), Eurasian (AM, AZ, BY, KG, KZ, RU, TJ, (72) Inventors: LEMIRE, Gaetan; 6505, rue de la fougere, TM), European (AL, AT, BE, BG, CH, CY, CZ, DE, DK, Sherbrooke, Quebec JIN 3W3 (CA). -

A Clinicopathological Analysis of Granulomatous
JK SCIENCE ORIGINAL ARTICLE A Clinicopathological Analysis of Granulomatous Dermatitis : 4 Year Retrospective Study Jyotsna Suri, Subhash Bhardwaj, Rita Kumari, Shailija Kotwal Abstract The present study was carried out with an attempt to study the incidence of granulomatous dermatitis in hospital based population and to classify and compare the granulomatous dermatitis on the basis of histopathology and find the etiology. This is a four year retrospective study done on the data available in the dermatopathology section of department of pathology. The cases diagnosed as granulomatous dermatitis were retrieved, clinical data and the histopathological features compared to know the incidence of various etiologies of GD. Out of 310 cases of GD with male to female ratio 2.03:1, leprosy comprised major reported etiology (n-244) followed by tuberculosis (n-44), sarcoidosis (n-4), Leshmania Donovani (n-14)) granuloma annulare (n-1) and 3 granulomatous lesions not further classified. Infections form the commonest form of GD out of which leprosy forms the major group. Role of histopathology(H&E and special stains) is very important in confirming the diagnosis of granulomatous dermatitis . Key Words Granuloma, Dermatitis, Inflammatory, Tissue Injury Introduction Granuloma is defined as a focal chronic inflammatory dermatitis presents a diagnostic challenge, many a times. response to tissue injury, characterised by focal, compact The granulomatous dermatitis comprise a large family collection of inflammatory cells, principally of the activated sharing the common histological denominator of histiocytes, modified epitheloid macrophages & granulomas formation. Rightly said that in granulomatous multinucleate giant cells that may or may not be rimmed dermatitis, an identical histologic picture may be produced by lymphocytes and show central necrosis. -

INTERNATIONAL JOURNAL of LEPROSY Volume 72, Number 1 Printed in the U.S.A
INTERNATIONAL JOURNAL OF LEPROSY Volume 72, Number 1 Printed in the U.S.A. (ISSN 0148-916X) INTERNATIONAL JOURNAL OF LEPROSY and Other Mycobacterial Diseases VOLUME 72, NUMBER 1MARCH 2004 Relapses in Multibacillary Patients Treated with Multi-drug Therapy until Smear Negativity: Findings after Twenty Years1 Gift Norman, Geetha Joseph, and Joseph Richard2 ABSTRACT The Schieffelin Leprosy Research and Training Center at Karigiri, India participated in several of the World Health Organization (WHO) trials. The first trial on combined therapy in multi-bacillary leprosy was initiated in 1981. The main objectives of this field trial were to evaluate the efficacy of WHO recommended regimens in preventing relapses, especially drug resistance relapses. This paper reports on the relapses twenty years after patients were inducted into the WHO field trial. Between 1981 and 1982, 1067 borderline lepromatous and lepromatous patients were in- ducted into the WHO field trial for combined therapy in multi-bacillary leprosy trial. Among them, 357 patients were skin smear positive. During the follow-up in 2002, only 173 of them could be traced and assessed. The mean duration of follow-up was 16.4 ± 1.83 years. Two patients relapsed 14 and 15 years after being released from treatment, the relapse rate being 0.07 per 100 person years follow-up. Drug susceptibility tests done on one of the relapsed patients revealed drug sensitive organisms to all multi-drug therapy drugs. RÉSUMÉ Le centre de recherche et de formation de Schieffelin à Karigiri aux Indes a participé à plusieurs études cliniques sponsorisées par l’Organisation Mondiale de la Santé (OMS). -

Fungal Infections in HIV-Positive Peruvian Patients: Could the Venezuelan Migration Cause a Health Warning Related-Infectious Diseases?
Moya-Salazar J, Salazar-Hernández R, Rojas-Zumaran V, Quispe WC. Fungal Infections in HIV-positive Peruvian Patients: Could the Venezuelan Migration Cause a Health Warning Related-infectious Diseases?. J Infectiology. 2019; 2(2): 3-10 Journal of Infectiology Journal of Infectiology Research Article Open Access Fungal Infections in HIV-positive Peruvian Patients: Could the Venezuelan Migration Cause a Health Warning Related-infectious Diseases? Jeel Moya-Salazar1,2*, Richard Salazar-Hernández3, Victor Rojas-Zumaran2, Wanda C. Quispe3 1School of Medicine, Faculties of Health Science, Universidad Privada Norbert Wiener, Lima, Peru 2Pathology Department, Hospital Nacional Docente Madre Niño San Bartolomé, Lima, Peru 3Cytopathology and Genetics Service, Department of Pathology, Hospital Nacional Guillermo Almenara Irigoyen, Lima, Peru Article Info Abstract Article Notes In patients with human immunodeficiency virus (HIV), opportunistic Received: December 22, 2018 infections occur that could compromise the health of patients. In order to Accepted: March 7, 2019 determine the frequency of fungal opportunistic and superficial infections *Correspondence: in HIV-positive men-who-have-sex-with-men (MSM) patients at the Hospital Jeel Moya-Salazar, M.T, M.Sc., 957 Pacific Street, Urb. Sn Nacional Guillermo Almenara, we conducted a cross-sectional retrospective Felipe, 07 Lima, Lima 51001, Peru; Telephone No: +51 986- study. We include Peruvian patients >18 years-old, derived from infectious or 014-954; Email: [email protected]. gynecological offices, with or without antiretroviral treatment. © 2019 Moya-Salazar J. This article is distributed under the One hundred thirteen patients were enrolled (36.7±10, range: 21 to terms of the Creative Commons Attribution 4.0 International 68 years), which 46 (40.7%) has an opportunistic fungal infection, mainly License. -

Histopathology of Important Fungal Infections
Journal of Pathology of Nepal (2019) Vol. 9, 1490 - 1496 al Patholo Journal of linic gist C of of N n e o p ti a a l- u i 2 c 0 d o n s 1 s 0 a PATHOLOGY A m h t N a e K , p d of Nepal a l a M o R e d n i io ca it l A ib ss xh www.acpnepal.com oc g E iation Buildin Review Article Histopathology of important fungal infections – a summary Arnab Ghosh1, Dilasma Gharti Magar1, Sushma Thapa1, Niranjan Nayak2, OP Talwar1 1Department of Pathology, Manipal College of Medical Sciences, Pokhara, Nepal. 2Department of Microbiology, Manipal College of Medical Sciences , Pokhara, Nepal. ABSTRACT Keywords: Fungus; Fungal infections due to pathogenic or opportunistic fungi may be superficial, cutaneous, subcutaneous Mycosis; and systemic. With the upsurge of at risk population systemic fungal infections are increasingly common. Opportunistic; Diagnosis of fungal infections may include several modalities including histopathology of affected tissue Systemic which reveal the morphology of fungi and tissue reaction. Fungi can be in yeast and / or hyphae forms and tissue reactions may range from minimal to acute or chronic granulomatous inflammation. Different fungi should be differentiated from each other as well as bacteria on the basis of morphology and also clinical correlation. Special stains like GMS and PAS are helpful to identify fungi in tissue sections. INTRODUCTION Correspondence: Dr Arnab Ghosh, MD Fungal infections or mycoses may be caused by Department of Pathology, pathogenic fungi which infect healthy individuals or by Manipal College of Medical Sciences, Pokhara, Nepal. -

Pseudomonas Skin Infection Clinical Features, Epidemiology, and Management
Am J Clin Dermatol 2011; 12 (3): 157-169 THERAPY IN PRACTICE 1175-0561/11/0003-0157/$49.95/0 ª 2011 Adis Data Information BV. All rights reserved. Pseudomonas Skin Infection Clinical Features, Epidemiology, and Management Douglas C. Wu,1 Wilson W. Chan,2 Andrei I. Metelitsa,1 Loretta Fiorillo1 and Andrew N. Lin1 1 Division of Dermatology, University of Alberta, Edmonton, Alberta, Canada 2 Department of Laboratory Medicine, Medical Microbiology, University of Alberta, Edmonton, Alberta, Canada Contents Abstract........................................................................................................... 158 1. Introduction . 158 1.1 Microbiology . 158 1.2 Pathogenesis . 158 1.3 Epidemiology: The Rise of Pseudomonas aeruginosa ............................................................. 158 2. Cutaneous Manifestations of P. aeruginosa Infection. 159 2.1 Primary P. aeruginosa Infections of the Skin . 159 2.1.1 Green Nail Syndrome. 159 2.1.2 Interdigital Infections . 159 2.1.3 Folliculitis . 159 2.1.4 Infections of the Ear . 160 2.2 P. aeruginosa Bacteremia . 160 2.2.1 Subcutaneous Nodules as a Sign of P. aeruginosa Bacteremia . 161 2.2.2 Ecthyma Gangrenosum . 161 2.2.3 Severe Skin and Soft Tissue Infection (SSTI): Gangrenous Cellulitis and Necrotizing Fasciitis. 161 2.2.4 Burn Wounds . 162 2.2.5 AIDS................................................................................................. 162 2.3 Other Cutaneous Manifestations . 162 3. Antimicrobial Therapy: General Principles . 163 3.1 The Development of Antibacterial Resistance . 163 3.2 Anti-Pseudomonal Agents . 163 3.3 Monotherapy versus Combination Therapy . 164 4. Antimicrobial Therapy: Specific Syndromes . 164 4.1 Primary P. aeruginosa Infections of the Skin . 164 4.1.1 Green Nail Syndrome. 164 4.1.2 Interdigital Infections . 165 4.1.3 Folliculitis . -

CHAPTER E16 Atlas of Skin Manifestations of Internal Disease CHAPTER E16 Thomas J
CHAPTER e16 Atlas of Skin Manifestations of Internal Disease CHAPTER e16 Thomas J. Lawley Robert A. Swerlick In the practice of medicine, virtually every clinician encounters patients with skin disease. Physicians of all specialties face the daily task of determining the nature and clinical implication of dermatologic disease. In patients with skin eruptions and rashes, the physician must confront the question of whether the cutaneous Atlas of Skin Manifestations Internal Disease process is confined to the skin, representing a pure dermatologic event, or whether it is a manifestation of internal disease relating to the patient’s overall medical condition. Evaluation and accurate diagnosis of skin lesions are also critical given the marked rise in both melanoma and nonmelanoma skin cancer. Dermatologic conditions can be classified and categorized in many different ways, Figure e16-2 Acne rosacea with prominent facial erythema, telangiecta- and in this Atlas, a selected group of inflammatory skin eruptions sias, scattered papules, and small pustules. (Courtesy of Robert Swerlick, and neoplastic conditions are grouped in the following manner: MD; with permission.) (A) common skin diseases and lesions, (B) nonmelanoma skin cancer, (C) melanoma and pigmented lesions, (D) infectious dis- ease and the skin, (E) immunologically mediated skin disease, and (F) skin manifestations of internal disease. COMMON SKIN DISEASES AND LESIONS ( Figs. e16-1 to e16-19) In this section, several common inflamma- tory skin diseases and benign neoplastic and reactive lesions are presented. While most of these dermatoses usually present as a pre- dominantly dermatologic process, underlying systemic associations may be made in some settings. Atopic dermatitis is often present in patients with an atopic diathesis, including asthma and sinusitis. -
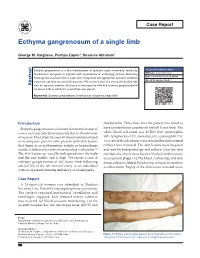
Ecthyma Gangrenosum of a Single Limb
Case Report Ecthyma gangrenosum of a single limb George M. Varghese, Pushpa Eapen1, Susanne Abraham1 Ecthyma gangrenosum is a skin manifestation of systemic sepsis commonly caused by Access this article online Pseudomonas aeruginosa in patients with neutropenia or underlying immune deficiency. Website: www.ijccm.org Although the usual outcome is poor, early recognition and appropriate systemic antibiotic DOI: 10.4103/0972-5229.84898 treatment can lead to successful outcome. We report a case of a previously healthy lady Quick Response Code: Abstract with no apparent immune deficiency or neutropenia who had ecthyma gangrenosum of left lower limb in which the arterial line was placed. Keywords: Ecthyma gangrenosum, Pseudomonas aeruginosa, single limb Introduction thachycardia. Three days later the patient was noted to Ecthyma gangrenosum is a known skin manifestation of have erythematous papules on the left lower limb. The 3 severe systemic infection commonly due to Pseudomonas white blood cell count was 16,500/mm (neutrophils aeruginosa. Most often it is seen in immunocompromised 84%, lymphocytes 12%, monocytes 3%, eosinophils 1%). or neutropenic patients who present with skin lesions Two sets of blood cultures were sent and the intra-arterial that begin as an erythematous nodule or hemorrhagic catheter was removed. The skin lesions were biopsied vesicle, which evolves into a necrotic ulcer with eschar. [1] and sent for histopathology and culture. Over the next The skin lesions are usually widespread over the body few days the skin lesions became blackish with necrotic and the case fatality rate is high. We report a case of areas (arrow) [Figure 1]. The blood, catheter tip, and skin ecthyma gangrenosum of left lower limb following lesion cultures yielded Pseudomonas aeruginosa sensitive arterial line in the left femoral artery in an individual to ceftazidime. -

Wade Histoid Leprosy: Histological and Immunohistochemical Analysis
Lepr Rev (2013) 84, 176–185 Wade histoid Leprosy: histological and immunohistochemical analysis DANIELA A.M. DA COSTA*, MI´LVIA M.S.S. ENOKIHARA**, SUELY NONOGAKI***, SOLANGE M. MAEDA****, ADRIANA M. PORRO**** & JANE TOMIMORI**** *Medical resident, Escola Paulista de Medicina/UNIFESP, Sa˜o Paulo, Brazil **Department of Pathology, Escola Paulista de Medicina/UNIFESP, Sa˜o Paulo, Brazil ***Pathology Center, Instituto Adolfo Lutz, Sa˜o Paulo, Brazil ****Department of Dermatology, Escola Paulista de Medicina/UNIFESP, Brazil Accepted for publication 1 October 2013 Summary Histoid leprosy is a rare multibacillary form that presents with disseminated papule-nodular cutaneous lesions. To study the inflammatory infiltrate of the histoid form and to compare it with other lepromatous forms, we performed histological and immunohistochemical analysis on skin biopsies. Fifteen patients were included for histopathological analysis (10 histoid and five lepromatous) via the haematoxylin-eosin and Ziehl-Neelsen-Faraco stains. Thus, immunohistochemical techniques using immunoperoxidase assay were performed for: anti-BCG, anti-M. leprae, anti-CD8, anti-CD3, anti-CD20, anti-S100, anti-CD1a, anti-CD68 and anti- vimentin. Spindle cells were present in all histoid patients. A pseudocapsule was observed in half of both studied forms. A comparison using the Ziehl-Neelsen-Faraco stain to evaluate anti-BCG and anti-M.leprae showed no major differences. The CD3þ cells were more pronounced in the histoid form than the lepromatous form. There was greater immunoreactivity toward CD8þ cells in the histoid form, as well as the CD20þ cell count. A similar count of S100þ cells in the epidermis of both leprosy forms was observed. There was a slight increase of dendritic cells in the histoid patients in the superficial and deep dermis. -

Skin and Soft Tissue Infections Following Marine Injuries
CHAPTER 6 Skin and Soft Tissue Infections Following Marine Injuries V. Savini, R. Marrollo, R. Nigro, C. Fusella, P. Fazii Spirito Santo Hospital, Pescara, Italy 1. INTRODUCTION Bacterial diseases following aquatic injuries occur frequently worldwide and usually develop on the extremities of fishermen and vacationers, who are exposed to freshwater and saltwater.1,2 Though plenty of bacterial species have been isolated from marine lesions, superficial soft tissue and invasive systemic infections after aquatic injuries and exposures are related to a restricted number of microorganisms including, in alphabetical order, Aeromonas hydrophila, Chromobacterium violaceum, Edwardsiella tarda, Erysipelothrix rhusiopathiae, Myco- bacterium fortuitum, Mycobacterium marinum, Shewanella species, Streptococcus iniae, and Vibrio vulnificus.1,2 In particular, skin disorders represent the third most common cause of morbidity in returning travelers and are usually represented by bacterial infections.3–12 Bacterial skin and soft tissue infectious conditions in travelers often follow insect bites and can show a wide range of clinical pictures including impetigo, ecthyma, erysipelas, abscesses, necro- tizing cellulitis, myonecrosis.3–12 In general, even minor abrasions and lacerations sustained in marine waters should be considered potentially contaminated with marine bacteria.3–12 Despite variability of the causative agents and outcomes, the initial presentations of skin and soft tissue infections (SSTIs) complicating marine injuries are similar to those occurring after terrestrial exposures and usually include erysipelas, impetigo, cellulitis, and necrotizing infections.3 Erysipelas is characterized by fiery red, tender, painful plaques showing well-demarcated edges, and, though Streptococcus pyogenes is the major agent of this pro- cess, E. rhusiopathiae infections typically cause erysipeloid displays.3 Impetigo is initially characterized by bullous lesions and is usually due to Staphylococcus aureus or S.