Federated States of Micronesia - 2014
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-
Fsm National Judiciary Annual Report 2012
FSM NATIONAL JUDICIARY ANNUAL REPORT 2012 TABLE OF CONTENTS Message from the Supreme Court—————————————–—————————–——1 Introduction———————————————————–——————–————–——–-2 Court’s Mission, Vision and Values—————————————–—————————–-–3 Past and Present Chief Justices ———————————–————–——————–———4 Associate Justices of the FSMSC———–——————————————–——————–5 Significant Developments in 2012————————–————————–———————–6 Case Management————————————————————–——————————7-12 Ombudsman Division Services——–—————————————————–————–—13 Operations and Support Information ——————————————–——————–——14-20 A. Budget and Revenues——————–——————————14 B. Court Personnel—————–————————-—————15 C. Library and Archives Services——————–—–————––16-17 D. Special Development Projects———————–—––—–——18-19 1. 5-Year Strategic Plan———————————–18 2. Facilities Improvements—————————–—18 3. Technology Infrastructure Improvement—–—–—19 E. Human Resource Capacity Building—————————–—20 Community Outreached Activities—————————————––———————–——21-22 A. Law Day 2012————————————–———–———21 B. Student Visit Program————————————————22 C. Librarian Outreached Services-———–————————–—22 FSM Bar —————————————————————————–—————–——23 FSM Supreme Court Membership Organizations—————————–—–—————–—24 FSM Supreme Court Organizational Chart———————————————–——–——25 ii Message from the Supreme Court Chief Justice Director of Court Administration Honorable Martin G. Yinug Mr. Kapilly Capelle Introduction General information: The Federated States of Micronesia (FSM) became autonomous and self-governing on May 10, -

COMET Spring 2015 Statistical Exploration by High School
COMET Spring 2015 Statistical Exploration by High School This document is an exploration of data from the College of Micronesia-FSM spring 2015 entrance COMET with a focus on individual high school and section statistics. In this document the word "sections" refers to high school sections. The word subsection will be used to refer to the different sections of the COMET entrance instrument. This document should be construed as an occasional informal paper by a member of faculty. Any opinions expressed are solely those of the author and do not reflect an official position of the college. Basic Statistics for All Candidates The COMET consists of four subsections: a written essay, a vocabulary test, a comprehension test, and a mathematics placement test. Total possible for the essay is 50 points. The mathematics subsection has four sets of ten problems designed to help place students. The total possible for the sum of the mathematics scores is 40. Nelson-Denny is used for the vocabulary and comprehension sections. Statistic Essay Vocabulary Reading MS1 MS2 MS3 MS4 Math sum n 1455 1456 1456 1456 1456 1456 1456 1456 min 0 0 0 0 0 0 0 3 max 50 69 38 10 10 10 10 38 mode 30 22 15 8 6 2 2 18 median 30 23 16.5 7 6 3 3 19 mean 28.28 24.78 17.28 6.94 6.01 3.59 2.90 19.44 sx 12.80 10.18 6.37 2.28 2.20 2.32 1.87 6.88 cv 0.45 0.41 0.37 0.33 0.37 0.65 0.65 0.35 High School Listing The following is a list of the high school names used in tables in this report. -
Infrastructure Development Plan (IDP)
Federated States of Micronesia INFRASTRUCTURE DEVELOPMENT PLAN FY2004-FY2023 Prepared by: DEPARTMENT OF TRANSPORTATION, COMMUNICATIONS & INFRASTRUCTURE MAY 2004 TABLE OF CONTENTS EXECUTIVE SUMMARY .......................................................................................................v 1. Introduction..............................................................................................................1 2. Preparation of Infrastructure Development Plan .....................................................2 2.1 Historical Background...................................................................................... 2 2.2 Preparation of Draft Final Report.................................................................... 2 2.3 Final IDP Report .............................................................................................. 3 2.4 Formal Submission of the IDP.......................................................................... 3 2.5 Preparation of Final IDP Document ................................................................ 3 3. Planning Context......................................................................................................4 3.1 FSM Planning Framework ............................................................................... 4 3.2 Public Sector Investment Program ................................................................... 4 3.3 Public and Private Sector Management of Infrastructure................................ 5 3.4 National Government Infrastructure Priorities............................................... -
Secondary and Postsecondary Math Education in Chuuk State, Federated States of Micronesia
DOCUMENT RESUME ED 401 107 SE 059 018 AUTHOR Patacsil, Peter E. TITLE Secondary and Postsecondary Math Education in Chuuk State, Federated States of Micronesia. PUB DATE 95 NOTE 16p. PUB TYPE Reports Descriptive (141) EDRS PRICE MF01/PC01 Plus Postage. DESCRIPTORS *Educational Quality; Foreign Countries; Higher Education; *Mathematics Education; Secondary Education; *Teacher Education IDENTIFIERS *Federated States of Micronesia ABSTRACT The public high school and three private high schools in Chuuk State (formerly called Truk), Federated States of Micronesia (FSM), are located on the main island of Weno. This report documents the present state of secondary and postsecondary mathematics education in Chuuk State. The information is primarily based on interviews with administrators and mathematics teachers at both the secondary and postsecondary levels in Chuuk State. It is reported that the quality of mathematics education varies from school to school ranging from an evolving system at the public high school to high quality and a commitment to excellence at Xavier High School, one of two Catholic high schools on the island. Except for these two catholic schools, there appears to be a shortage of mathematics teachers at the secondary level. The associate degree and three of the four certificate programs offered by the extension center of the College of Micronesia (COM) specify mathematics requirements. However, data indicate that COM's Chuuk State campus has difficulty in recruiting and retaining mathematics instructors. It was concluded that there is a shortage of mathematics teachers both at the secondary and postsecondary level in Chuuk State. (JRH) *********************************************************************** Reproductions supplied by EDRS are the best that can be made from the original document. -
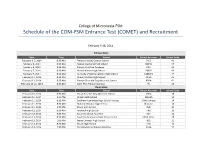
Schedule of the COM-‐FSM Entrance Test (COMET) and Recruitment
College of Micronesia-FSM Schedule of the COM-FSM Entrance Test (COMET) and Recruitment February 3-18, 2014 Pohnpei State Date Time School School Acronym School Code February 3-5, 2014 8:30 AM Pohnpei Islands Central School PICS 40 February 6, 2014 8:30 AM Nanpei Memorial High School NMHS 44 February 6, 2014 8:30 AM Calvary Christian Academy CCA 42 February 7, 2014 8:30 AM Madolenihmw High School PMHS 43 February 7, 2014 8:30 AM Our Lady of Mercy Catholic High School OLMCHS 47 February 11, 2014 8:30 AM Ohwa Christian High School OCHS 45 February 13, 2014 8:30 AM Pohnpei Seventh Day Adventist School PSDA 41 February 13-14, 2014 8:30 AM COM-FSM Pohnpei Campus PC 46 Chuuk State Date Time School School Acronym School Code February 10, 2014 8:30 AM Chuuk Seventh Day Adventist School CSDA 18 February 10, 2014 1:00 PM Mizpah High School Mizpah 15 February 11, 2014 8:30 AM Southern Namoneas High School-Tonoas SNHS-Tonoas 24 February 11, 2014 8:30 AM Nukuno Christian High School Nukuno 14 February 11, 2014 1:00 PM Xavier High School XHS 10 February 12, 2014 8:30 AM Faichuuk High School FHS 19 February 13, 2014 8:30 AM Saramen Chuuk Academy SCA 13 February 13, 2014 8:30 AM Southern Namoneas High School-Fefan SNHS-Fefan 24 February 13, 2014 1:00 AM Berea Christian High School BCS 11 February 14, 2014 8:30 AM Chuuk High School CHS 12 February 14, 2014 1:00 PM Pentecostal Lighthouse Academy PLHA 17 February 15, 2014 8:30 AM COM-FSM Chuuk Campus CC 21 Yap State Date Time School School Acronym School Code February 17, 2014 8:30 AM Yap Catholic High School YCHS 66 February 17, 2014 8:30 AM Outer Island High School (Ulithi) OIHS 63 February 17, 2014 8:30 AM Yap Seventh Day Adventist School YSDA 61 February 17, 2014 1:00 P.M. -

Taking Responsibility for Our Schools: a Series of Four Articles on Education in Micronesia. INSTITUTION Pacific Resources for Education and Learning, Honolulu, HI
DOCUMENT RESUME ED 467 541 RC 023 666 AUTHOR Hezel, Francis X. TITLE Taking Responsibility for Our Schools: A Series of Four Articles on Education in Micronesia. INSTITUTION Pacific Resources for Education and Learning, Honolulu, HI. Region XV Comprehensive Assistance Center. SPONS AGENCY Department of Education, Washington, DC. PUB DATE 2002-06-00 NOTE 49p.; Introduction by Hilda C. Heine. CONTRACT S283A950001 PUB TYPE Opinion Papers (120) Reports Descriptive (141) EDRS PRICE EDRS Price MF01/PCO2 Plus Postage. DESCRIPTORS Academic Achievement; Brain Drain; Community Involvement; Education Work Relationship; Educational Change; *Educational Objectives; Elementary Secondary Education; Foreign Countries; *Pacific Islanders; Parent Participation; *Role of Education; *School Community Relationship; School Culture; *School Effectiveness IDENTIFIERS Exemplary Schools; *Federated States of Micronesia; Marshall Islands; Palau ABSTRACT Mobilizing communities to support educational improvements is one of the challenges confronting educators in the Freely Associated States (FAS), which consists of the Federated States of Micronesia, the Republic of the Marshall Islands, and the Republic of Palau. This booklet aims to establish a consensus on broad educational goals and to rebuild the sense of community ownership of schools that is missing today. "What Should Our Schools Be Doing?" describes conflicting views about whether education should provide for manpower training, cultural preservation, or academic skills, given the current poor academic achievement in the FAS and high rates of emigration to find work. It is suggested that a new education system can accommodate all three visions. "How Good Are Our Schools?" attempts to show the current status of schooling in each country but is hampered by incomplete data. Although test scores are the only data consistently available, there are other measures for school success. -

Chuuk State Infrastructure Development Plan FY2016-FY2025
Federated States of Micronesia INFRASTRUCTURE DEVELOPMENT PLAN FY2016-FY2025 Volume 3: Chuuk State Infrastructure Development Plan FY2016-FY2025 This Federated States of Micronesia Infrastructure Development Plan FY2016-FY2025 comprises the following parts: Introduction Volume 1 Plan Outline Annexes Volume 2 National Infrastructure Development Plan Volume 3 Chuuk State Infrastructure Development Plan Volume 4 Kosrae State Infrastructure Development Plan Volume 5 Pohnpei State Infrastructure Development Plan Volume 6 Yap State Infrastructure Development Plan The following Federated States of Micronesia Infrastructure Development Plan FY2016-FY2025 documents are available: Federated States of Micronesia Infrastructure Development Plan FY2016-FY2025 (all parts) FSM Infrastructure Development Plan FY2016-FY2025 Outline (Introduction, Volume 1 & Annexes) National Infrastructure Development Plan FY2016-FY2025 (Volume 2) Chuuk State Infrastructure Development Plan FY2016-FY2025 (Volume 3) Kosrae State Infrastructure Development Plan FY2016-FY2025 (Volume 4) Pohnpei State Infrastructure Development Plan FY2016-FY2025 (Volume 5) Yap State Infrastructure Development Plan FY2016-FY2025 (Volume 6) FSM Infrastructure Development Plan FY2016-FY2025 Summary (abbreviated outline and listings of projects) FSM Infrastructure Development Plan FY2016-FY2025 Volume 3 Chuuk State Infrastructure Development Plan Foreword by the Governor LAN P EVELOPMENT D NFRASTRUCTURE I TATE S HUUK C V o l u m e 3 Chuuk State Infrastructure Development Plan P a g e | i FSM -

Envisioning a Culturally Responsive Educational System for Chuuk State
WAY FINDING: ENVISIONING A CULTURALLY RESPONSIVE EDUCATIONAL SYSTEM FOR CHUUK STATE, FEDERATED STATES OF MICRONESIA A DISSERTATION SUBMITTED TO THE GRADUATE DIVISION OF THE UNIVERSITY OF HAWAI`I AT MĀNOA IN PARTIAL FULFILLMENT OF THE REQUIREMENTS FOR THE DEGREE OF DOCTOR OF PHILOSOPHY IN EDUCATION MAY 2013 By Margarita Cholymay Dissertation Committee: Pauline Chinn, Chairperson James Skouge Margaret Maaka Mark Merlin Andrea Bartlett Lola Quan Bautista Keywords: Chuuk, Micronesia, Indigenous, Educational Reform, and Traditional Value. UMI Number: 3572416 All rights reserved INFORMATION TO ALL USERS The quality of this reproduction is dependent upon the quality of the copy submitted. In the unlikely event that the author did not send a complete manuscript and there are missing pages, these will be noted. Also, if material had to be removed, a note will indicate the deletion. UMI 3572416 Published by ProQuest LLC (2013). Copyright in the Dissertation held by the Author. Microform Edition © ProQuest LLC. All rights reserved. This work is protected against unauthorized copying under Title 17, United States Code ProQuest LLC. 789 East Eisenhower Parkway P.O. Box 1346 Ann Arbor, MI 48106 - 1346 ACKNOWLEDGEMENTS “Aramas chok angang” is a driving force behind this study in that “no work is a product of one woman.” This work might not have come this far without the support of many. Papa, as early as 1960s when fathers thought of nothing but only wanted to see their daughters getting married and had kids, your words keep ringing in my ears, “Iei ii nei ei lekkis epwe tori college.” (Gesturing to his friends, “Here is my daughter who will destine to college.” A Special gratitude goes to you, only if you lived to witness such an honor. -

FOURTH REGULAR SESSION TWENTIETH CONGRESS Federated States of Micronesia
JOURNAL FOURTH REGULAR SESSION TWENTIETH CONGRESS of the Federated States of Micronesia PALIKIR, POHNPEI August 2015 PALIKIR, POHNPEI Convened on Friday, 11th of May 2018 Adjourned on Monday, 28th of May 2018 JOURNAL FOURTH REGULAR SESSION TWENTIETH CONGRESS OF THE FEDERATED STATES OF MICRONESIA July 2018 PALIKIR, POHNPEI Convened on Friday, 11th, of May 2018 Adjourned on Monday, 28th of May 2018 Compiled by the Office of the Speaker And Printed by Good News Press – Kolonia, Pohnpei Twentieth Congress of the Federated States of Micronesia FOURTH REGULAR SESSION May 11th, 2018 thru May 28th, 2018 TABLE OF CONTENTS SECTION No. Page CERTIFICATION …………………… IV ORGANIZATION Leadership and Membership …………………… V Standing Committees …………………… VI Congressional Offices …………………… VII SUMMARY OF LEGISLATION …………………… VIII-XII DAILY JOURNAL INDEX …………………… XIII-XIV DAILY JOURNAL …………………… 1-172 STANDING COMMITTEE REPORTS …………………… 173-218 SPECIAL COMMITTEE REPORTS ............................... 219-221 COMMUNICATIONS Presidential Communications …………………… 222-227 FSM Supreme Court Communications …………………… 228-229 Member Communications …………………… 230-232 Departmental Communications …………………… 233-234 Agencies and Governmental Authorities …………………… 235-236 State Communications …………………… 237-238 State Supreme Court Communications …………………… 239-240 Municipal or Town Communications …………………… 241-242 Foreign Government Communications …………………… 243-245 Miscellaneous Communications …………………… 246-247 PRESIDENTIAL VETO MESSAGE …………………… 248-249 CONSTITUTION OF THE FEDERATED STATES -

NMCT Math Trend 35% 33% 30% 30% 29% 27% 25% 25% 20% 15% 10% 5% 0% 2014-2015 2016-2017 2017-2018
1 | P a g e Contents Background......................................................................................................................... 3 Student Assessment .......................................................................................................... 3 Exams Results for Nation-wide Performance by Benchmarks .................................. 3 Exam Results for Recent Years by Standards .............................................................. 3 Exams Results Comparing States ................................................................................. 3 Sixth Grade Reading Results ......................................................................................... 4 Eighth Grade Reading Results ....................................................................................... 4 Tenth Grade Reading Results ........................................................................................ 5 Sixth Grade Math Results .............................................................................................. 6 Tenth Grade Math Results ............................................................................................. 8 List of Figures Figure 1: Grade 6 Reading Benchmarks – meeting or exceeding ................................. 4 Figure 2: Grade 8 – Reading Benchmarks – meeting or exceeding ............................... 5 Figure 3: Grade 10 -Reading Benchmarks – meeting or exceeding .............................. 5 Figure 4: Grade 4 Math benchmarks – meeting or exceeding -

Chuuk State Strategic Development Plan
Chuuk State Economic Development Commission Chuuk State Strategic Development Plan 2018 to 2023 DRESCO Consulting: Roger Arnold 8/31/2016 CHUUK STATE STRATEGIC DEVELOPMENT PLAN 1 CHUUK STATE STRATEGIC DEVELOPMENT PLAN Table of Content Abbreviations Pg. 2-4 Section 1 Foreword Pg. 5 Chapter 1. Chuuk State Pg. 6-11 Chapter 2. Development Areas Pg. 12-34 Chapter 3. Format (SDP) Pg. 35-44 Section 2 Strategic Plans Pg. 45 Chapter 4. Private Sector Pg. 46-65 Chapter 5. Agriculture Sector Pg. 67-84 Chapter 6. Marine Resources Sector Pg. 85-101 Chapter 7. Tourism Sector Pg. 102-118 Chapter 8. Health Sector Pg. 119-142 Chapter 9. Education Sector Pg. 143-166 Chapter 10. Social Sector Pg. 167-180 Chapter 11. Environment Sector Pg. 181-196 Chapter 12. Energy Sector Pg. 197-209 Chapter 13. Infrastructure Sector Pg. 210-231 Section 3 Activity Matrices Pg. 232 Private Sector Matrices Pg. 233-238 Agriculture Sector Matrices Pg. 239-245 Marine Resources Sector Matrices Pg. 246-252 Tourism Sector Matrices Pg. 253-258 Health Sector Matrices Pg. 259-270 Education Sector Matrices Pg. 271-279 Social Sector Matrices Pg. 280-284 Environment Sector Matrices Pg. 285-291 Energy Sector Matrices Pg. 292-297 Infrastructure Sector Matrices Pg. 298-303 Section 4 Appendices and References Pg. 310 References Pg. 311-313 Appendices 2 CHUUK STATE STRATEGIC DEVELOPMENT PLAN Abbreviations ADB Asian Development Bank AFT Agriculture Food and Technology AWOL Absent Without Official Leave C&I Commerce and Industry CAC Chuuk Athletic Club CCDP Chuuk Community Development Program -
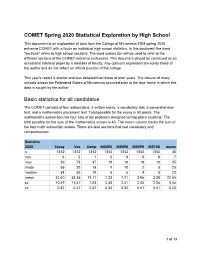
COMET Spring 2020 High School Report
COMET Spring 2020 Statistical Exploration by High School This document is an exploration of data from the College of Micronesia-FSM spring 2020 entrance COMET with a focus on individual high school statistics. In this document the word "sections" refers to high school sections. The word subsection will be used to refer to the different sections of the COMET entrance instrument. This document should be construed as an occasional informal paper by a member of faculty. Any opinions expressed are solely those of the author and do not reflect an official position of the college. This year's report is shorter and less detailed than those of prior years. The closure of many schools across the Federated States of Micronesia occurred prior to the time frame in which this data is sought by the author. Basic statistics for all candidates The COMET consists of four subsections: a written essay, a vocabulary test, a comprehension test, and a mathematics placement test. Total possible for the essay is 50 points. The mathematics subsection has four sets of ten problems designed to help place students. The total possible for the sum of the mathematics scores is 40. The msum column tracks the sum of the four math subsection scores. There are also sections that test vocabulary and comprehension. Statistics 2020 Essay Voc Comp MS095 MS096 MS099 MS100 msum n 1352 1352 1352 1352 1352 1352 1352 48 min 0 2 1 0 0 0 0 7 max 50 79 37 10 10 10 10 35 mode 36 20 18 9 10 2 3 25 median 34 30 19 8 8 4 3 23 mean 32.40 33.46 19.17 7.23 7.21 3.96 3.38 22.65 sx 10.49 15.67 7.04 2.48 2.31 2.43 2.06 5.56 cv 0.32 0.47 0.37 0.34 0.32 0.61 0.61 0.25 1 of 13 Correlations internal to the data Correlations Essay Voc Comp MS095 MS096 MS099 MS100 msum Essay 1.00 0.38 0.63 0.47 0.48 0.33 0.22 -0.03 Vocab 0.38 1.00 0.44 0.26 0.30 0.28 0.28 0.26 Comp 0.63 0.44 1.00 0.48 0.53 0.47 0.33 0.30 Math sum -0.03 0.26 0.30 0.73 0.67 0.79 0.61 1.00 Correlation of the language sections of the COMET to the mathematics sections are low, with especially poor correlations to skills in college algebra.