Management of Hypertriglyceridemia: Common Questions and Answers
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Lipid Lowering Agents, Cognitive Decline, and Dementia: the Three-City Study
Lipid lowering agents, cognitive decline, and dementia: the three-city study. Marie-Laure Ancelin, Isabelle Carrière, Pascale Barberger-Gateau, Sophie Auriacombe, Olivier Rouaud, Spiros Fourlanos, Claudine Berr, Anne-Marie Dupuy, Karen Ritchie To cite this version: Marie-Laure Ancelin, Isabelle Carrière, Pascale Barberger-Gateau, Sophie Auriacombe, Olivier Rouaud, et al.. Lipid lowering agents, cognitive decline, and dementia: the three-city study.: Lipid Lowering Agents and Cognitive Decline. Journal of Alzheimer’s Disease, IOS Press, 2012, 30 (3), pp.629-37. 10.3233/JAD-2012-120064. inserm-00707350 HAL Id: inserm-00707350 https://www.hal.inserm.fr/inserm-00707350 Submitted on 12 Jun 2012 HAL is a multi-disciplinary open access L’archive ouverte pluridisciplinaire HAL, est archive for the deposit and dissemination of sci- destinée au dépôt et à la diffusion de documents entific research documents, whether they are pub- scientifiques de niveau recherche, publiés ou non, lished or not. The documents may come from émanant des établissements d’enseignement et de teaching and research institutions in France or recherche français ou étrangers, des laboratoires abroad, or from public or private research centers. publics ou privés. Lipid lowering agents, cognitive decline, and dementia: the three-city study Marie-Laure Ancelin 1 * , Isabelle Carrière 1 , Pascale Barberger-Gateau 2 , Sophie Auriacombe 2 , Olivier Rouaud 3 , Spiros Fourlanos 4 , Claudine Berr 1 , Anne-Marie Dupuy 1 5 , Karen Ritchie 1 6 1 Neuropsychiatrie : Recherche Epidémiologique -

Blood Fats Explained
Blood Fats Explained HEART UK – The Cholesterol Charity providing expert support, education and influence 2 | Fats in the blood At risk of cardiovascular disease? | 3 Fats in the blood At risk of cardiovascular disease? Fats that circulate in the blood are called lipids. Very low density lipoproteins (VLDL) transport Cardiovascular disease (CVD) is the medical Blood pressure is a measure of the resistance Cholesterol and triglycerides are both lipids. mainly triglycerides made by the liver to where name for circulatory diseases such as coronary to the flow of blood around your body. It is They have essential roles in the body. In excess they are either used to fuel our muscles or stored heart disease (CHD), stroke, mini stroke (transient measured in millimetres of mercury (mmHg). Your they are harmful. for later use. ischaemic attack or TIA), angina and peripheral doctor or nurse will measure both your systolic vascular disease (PVD). You are more likely to (upper figure) and diastolic (lower figure) blood Cholesterol is needed to build cell walls and Low density lipoproteins (LDL) carry most of the develop CVD the more risk factors you have. pressure. About a third of adults have high blood to make hormones and vitamin D. Some of our cholesterol in our body from the liver to the cells pressure. If untreated it increases the risk of cholesterol comes from the food we eat; but most that need it. The cholesterol that is carried on LDLs There are two types of risk factors: heart attack and stroke. High blood pressure is is made in the liver. -

Case Report: Eruptive Xanthoma in a 14-Year-Old Boy Ryan M
Case Report: Eruptive Xanthoma in a 14-year-old boy Ryan M. Proctor, DO; Warren A. Peterson, DO; Michael W. Peterson, DO: Michael R. Proctor, DO; J. Ryan Jackson, DO; Andrew C. Duncanson OMS4; Allen E. Stout, DC. Dr. R. Proctor, Dr. W. Peterson, Dr. M. Peterson are from Aspen Dermatology Residency, Spanish Fork, UT; Dr. M. Proctor is from Arizona Desert Dermatology, Kingman, AZ; Dr. Jackson is from Sampson Regional Medical Center, Clinton, NC; OMS4 Duncanson is from Des Moines University, Des Moines, IA; DC Stout is from Stout Wellness Center, Fort Mohave, AZ. INTRODUCTION CLINICAL PHOTOS DISCUSSION Xanthomas are benign collections of lipid deposits that manifest as yellow to Eruptive xanthomas (EX) are often an indicator of severe red firm papules, nodules, or plaques. This yellow/red coloration is due to the hypertriglyceridemia and can indicate undiagnosed or Figure 1 Figure 2 carotene in lipids. Xanthomas are composed of lipid filled macrophages decompensated diabetes mellitus (DM).1 The triglyceride levels in known as “foam cells”. Xanthomas can be due to genetic disorders of lipid these patients can be >3000-4000 mg/dl (normal <150 mg/dl).2 metabolism, such as autosomal dominant hypocholesteremia or familial lipoprotein lipase(LPL) deficiency.1,2 They can also be caused by severe It is important to quickly diagnose and manage these patients due hypertriglyceridemia and have been associated with undiagnosed diabetic to the possible sequela of diabetes mellitus and hyperlipidemia. dyslipidemia, hypothyroidism, cholestasis, nephrotic -

Genetic Testing for Familial Hypercholesterolemia AHS – M2137
Corporate Medical Policy Genetic Testing for Familial Hypercholesterolemia AHS – M2137 File Name: genetic_testing_for_familial_hypercholesterolemia Origination: 01/01/2019 Last CAP Review: 07/2021 Next CAP Review: 07/2022 Last Review: 07/2021 Description of Procedure or Service Definitions Familial hypercholesterolemia (FH) is a genetic condition that results in premature atherosclerotic cardiovascular disease due to lifelong exposure to elevated low-density lipoprotein cholesterol (LDL-C) levels (Sturm et al., 2018). FH encompasses multiple clinical phenotypes associated with distinct molecular etiologies. The most common is an autosomal dominant disorder caused by mutations in one of three genes, low-density lipoprotein receptor (LDLR), apolipoprotein B-100 (APOB), and proprotein convertase subtilisin-like kexin type 9 (PCSK9) (Ahmad et al., 2016; Goldberg et al., 2011). Rare autosomal recessive disease results from mutation in low-density lipoprotein receptor adaptor protein (LDLRAP) (Garcia et al., 2001). Related Policies Cardiovascular Disease Risk Assessment AHS – G2050 ***Note: This Medical Policy is complex and technical. For questions concerning the technical language and/or specific clinical indications for its use, please consult your physician. Policy BCBSNC will provide coverage for genetic testing for familial hypercholesterolemia when it is determined the medical criteria or reimbursement guidelines below are met. Benefits Application This medical policy relates only to the services or supplies described herein. Please refer to the Member's Benefit Booklet for availability of benefits. Member's benefits may vary according to benefit design; therefore member benefit language should be reviewed before applying the terms of this medical policy. When Genetic Testing for Familial Hypercholesterolemia is covered 1. Genetic testing to establish a molecular diagnosis of Familial Hypercholesterolemia is considered medically necessary when BOTH of the following criteria are met: A. -

Apoa5genetic Variants Are Markers for Classic Hyperlipoproteinemia
CLINICAL RESEARCH CLINICAL RESEARCH www.nature.com/clinicalpractice/cardio APOA5 genetic variants are markers for classic hyperlipoproteinemia phenotypes and hypertriglyceridemia 1 1 1 2 2 1 1 Jian Wang , Matthew R Ban , Brooke A Kennedy , Sonia Anand , Salim Yusuf , Murray W Huff , Rebecca L Pollex and Robert A Hegele1* SUMMARY INTRODUCTION Hypertriglyceridemia is a common biochemical Background Several known candidate gene variants are useful markers for diagnosing hyperlipoproteinemia. In an attempt to identify phenotype that is observed in up to 5% of adults. other useful variants, we evaluated the association of two common A plasma triglyceride concentration above APOA5 single-nucleotide polymorphisms across the range of classic 1.7 mmol/l is a defining component of the meta 1 hyperlipoproteinemia phenotypes. bolic syndrome and is associated with several comorbidities, including increased risk of cardio Methods We assessed plasma lipoprotein profiles and APOA5 S19W and vascular disease2 and pancreatitis.3,4 Factors, –1131T>C genotypes in 678 adults from a single tertiary referral lipid such as an imbalance between caloric intake and clinic and in 373 normolipidemic controls matched for age and sex, all of expenditure, excessive alcohol intake, diabetes, European ancestry. and use of certain medications, are associated Results We observed significant stepwise relationships between APOA5 with hypertriglyceridemia; however, genetic minor allele carrier frequencies and plasma triglyceride quartiles. The factors are also important.5,6 odds ratios for hyperlipoproteinemia types 2B, 3, 4 and 5 in APOA5 S19W Complex traits, such as plasma triglyceride carriers were 3.11 (95% CI 1.63−5.95), 4.76 (2.25−10.1), 2.89 (1.17−7.18) levels, usually do not follow Mendelian patterns of and 6.16 (3.66−10.3), respectively. -

Lipodystrophy Due to Adipose Tissue Specific Insulin Receptor
Page 1 of 50 Diabetes Lipodystrophy Due to Adipose Tissue Specific Insulin Receptor Knockout Results in Progressive NAFLD Samir Softic1,2,#, Jeremie Boucher1,3,#, Marie H. Solheim1,4, Shiho Fujisaka1, Max-Felix Haering1, Erica P. Homan1, Jonathon Winnay1, Antonio R. Perez-Atayde5, and C. Ronald Kahn1. 1 Section on Integrative Physiology and Metabolism, Joslin Diabetes Center and Department of Medicine, Harvard Medical School, Boston, MA 2 Division of Gastroenterology, Hepatology and Nutrition, Boston Children’s Hospital, Boston, MA 3 Cardiovascular and Metabolic Diseases iMed, AstraZeneca R&D, 431 83 Mölndal, Sweden (current address) 4 KG Jebsen Center for Diabetes Research, Department of Clinical Science, University of Bergen, Bergen, Norway 5 Department of Pathology, Boston Children’s Hospital, and Harvard Medical School, Boston, MA # These authors contributed equally to this work. Corresponding author: C. Ronald Kahn, MD Joslin Diabetes Center One Joslin Place Boston, MA 02215 Phone: (617)732-2635 Fax:(617)732-2487 E-mail: [email protected] Keywords: Insulin receptors, IGF-1 receptors, lipodystrophy, diabetes, dyslipidemia, fatty liver, liver tumor, NAFLD, NASH. Running title: Lipodystrophic mice develop progressive NAFLD 1 Diabetes Publish Ahead of Print, published online May 10, 2016 Diabetes Page 2 of 50 SUMMARY Ectopic lipid accumulation in the liver is an almost universal feature of human and rodent models of generalized lipodystrophy and also is a common feature of type 2 diabetes, obesity and metabolic syndrome. Here we explore the progression of fatty liver disease using a mouse model of lipodystrophy created by a fat-specific knockout of the insulin receptor (F-IRKO) or both IR and insulin-like growth factor-1 receptor (F- IR/IGF1RKO). -

Stems for Nonproprietary Drug Names
USAN STEM LIST STEM DEFINITION EXAMPLES -abine (see -arabine, -citabine) -ac anti-inflammatory agents (acetic acid derivatives) bromfenac dexpemedolac -acetam (see -racetam) -adol or analgesics (mixed opiate receptor agonists/ tazadolene -adol- antagonists) spiradolene levonantradol -adox antibacterials (quinoline dioxide derivatives) carbadox -afenone antiarrhythmics (propafenone derivatives) alprafenone diprafenonex -afil PDE5 inhibitors tadalafil -aj- antiarrhythmics (ajmaline derivatives) lorajmine -aldrate antacid aluminum salts magaldrate -algron alpha1 - and alpha2 - adrenoreceptor agonists dabuzalgron -alol combined alpha and beta blockers labetalol medroxalol -amidis antimyloidotics tafamidis -amivir (see -vir) -ampa ionotropic non-NMDA glutamate receptors (AMPA and/or KA receptors) subgroup: -ampanel antagonists becampanel -ampator modulators forampator -anib angiogenesis inhibitors pegaptanib cediranib 1 subgroup: -siranib siRNA bevasiranib -andr- androgens nandrolone -anserin serotonin 5-HT2 receptor antagonists altanserin tropanserin adatanserin -antel anthelmintics (undefined group) carbantel subgroup: -quantel 2-deoxoparaherquamide A derivatives derquantel -antrone antineoplastics; anthraquinone derivatives pixantrone -apsel P-selectin antagonists torapsel -arabine antineoplastics (arabinofuranosyl derivatives) fazarabine fludarabine aril-, -aril, -aril- antiviral (arildone derivatives) pleconaril arildone fosarilate -arit antirheumatics (lobenzarit type) lobenzarit clobuzarit -arol anticoagulants (dicumarol type) dicumarol -

Commonly Used Lipidcentric ICD-10 (ICD-9) Codes
Commonly Used Lipidcentric ICD-10 (ICD-9) Codes *This is not an all inclusive list of ICD-10 codes R.LaForge 11/2015 E78.0 (272.0) Pure hypercholesterolemia E78.3 (272.3) Hyperchylomicronemia (Group A) (Group D) Familial hypercholesterolemia Grütz syndrome Fredrickson Type IIa Chylomicronemia (fasting) (with hyperlipoproteinemia hyperprebetalipoproteinemia) Hyperbetalipoproteinemia Fredrickson type I or V Hyperlipidemia, Group A hyperlipoproteinemia Low-density-lipoid-type [LDL] Lipemia hyperlipoproteinemia Mixed hyperglyceridemia E78.4 (272.4) Other hyperlipidemia E78.1 (272.1) Pure hyperglyceridemia Type 1 Diabetes Mellitus (DM) with (Group B) hyperlipidemia Elevated fasting triglycerides Type 1 DM w diabetic hyperlipidemia Endogenous hyperglyceridemia Familial hyperalphalipoproteinemia Fredrickson Type IV Hyperalphalipoproteinemia, familial hyperlipoproteinemia Hyperlipidemia due to type 1 DM Hyperlipidemia, Group B Hyperprebetalipoproteinemia Hypertriglyceridemia, essential E78.5 (272.5) Hyperlipidemia, unspecified Very-low-density-lipoid-type [VLDL] Complex dyslipidemia hyperlipoproteinemia Elevated fasting lipid profile Elevated lipid profile fasting Hyperlipidemia E78.2 (272.2) Mixed hyperlipidemia (Group C) Hyperlipidemia (high blood fats) Broad- or floating-betalipoproteinemia Hyperlipidemia due to steroid Combined hyperlipidemia NOS Hyperlipidemia due to type 2 diabetes Elevated cholesterol with elevated mellitus triglycerides NEC Fredrickson Type IIb or III hyperlipoproteinemia with E78.6 (272.6) -

The Effect of Omega-3 Fatty Acids on Hypertriglyceridemia: a Review
Review Article ISSN: 2574 -1241 DOI: 10.26717/BJSTR.2020.26.004382 The Effect of Omega-3 Fatty Acids on Hypertriglyceridemia: A Review Alaa Abousetta, Ibrahim Abousetta, Theresa Dobler, Lia Ebrahimi, Vassillis Frangoullis, Stephanos Christodoulides and Ioannis Patrikios* School of Medicine, European University Cyprus, Cyprus *Corresponding author: Ioannis Patrikios, School of Medicine, European University Cyprus, Cyprus ARTICLE INFO Abstract Received: March 06, 2020 Hypertriglyceridemia is a common problem in adults in the developed world. It is associated with increased levels of triglycerides within the blood, which subsequently Published: March 17, 2020 promote the development of other diseases such as cardiovascular disease and pancreatitis. Triglycerides are mostly consumed through the diet and act as a source of energy in between meals. However, the levels of triglycerides increase proportionally Citation: Alaa A, Ibrahim A, Theresa D, Lia with the number of calories consumed. This only leads to a problem if the total daily E, Ioannis P, et al., The Effect of Omega-3 energy expenditure is exceeded. Additionally, the type of macronutrients taken in Fatty Acids on Hypertriglyceridemia: A Re- view. Biomed J Sci & Tech Res 26(4)-2020. for instance, high carbohydrate intake has been associated with an increased plasma BJSTR. MS.ID.004382. triglyceridethrough the level.diet has If thea direct levels influence of the triglycerideson having an inincreased the blood level rise of abovetriglycerides, 150 mg/ as Abbreviations: FHTG: Familial hypertri- dL, it is considered as hypertriglyceridemia. Increasing numbers of triglycerides can glyceridemia; FCH: Familial Combined Hy- have multiple underlying causes, which can be divided into primary and secondary perlipidemia, systemic lupus erythemato- causes. -
Omega-3 Fatty Acids Fact Sheet for Consumers
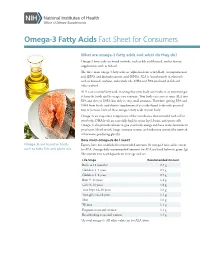
Omega-3 Fatty Acids Fact Sheet for Consumers What are omega-3 fatty acids and what do they do? Omega-3 fatty acids are found in foods, such as fish and flaxseed, and in dietary supplements, such as fish oil. The three main omega-3 fatty acids are alpha-linolenic acid (ALA), eicosapentaenoic acid (EPA), and docosahexaenoic acid (DHA). ALA is found mainly in plant oils such as flaxseed, soybean, and canola oils. DHA and EPA are found in fish and other seafood. ALA is an essential fatty acid, meaning that your body can’t make it, so you must get it from the foods and beverages you consume. Your body can convert some ALA into EPA and then to DHA, but only in very small amounts. Therefore, getting EPA and DHA from foods (and dietary supplements if you take them) is the only practical way to increase levels of these omega-3 fatty acids in your body. Omega-3s are important components of the membranes that surround each cell in your body. DHA levels are especially high in retina (eye), brain, and sperm cells. Omega-3s also provide calories to give your body energy and have many functions in your heart, blood vessels, lungs, immune system, and endocrine system (the network of hormone-producing glands). How much omega-3s do I need? Omega-3s are found in foods Experts have not established recommended amounts for omega-3 fatty acids, except such as fatty fish and plant oils. for ALA. Average daily recommended amounts for ALA are listed below in grams (g). -

The Effects of Statin and Fibrate Drugs on Cholesterol Metabolism And
The effects of statin and fibrate drugs on cholesterol metabolism and steroid production in two fish species. By Aziz Al-Habsi Thesis submitted to the Faculty of Graduate and Postdoctoral Studies University of Ottawa In partial fulfillment of the requirements for the PhD degree in the Ottawa-Carleton Institute of Biology Thèse soumise à la Faculté des Études Supérieurs et Postdoctorales Université d’Ottawa En vue de la réalisation partielle du doctorat à L’Institut de Biologie Ottawa-Carleton ©Aziz Al-Habsi, Ottawa, Canada, 2014 This thesis is dedicated to my wife and children who have always stood by me and dealt with all my absence from many family occasions with a smile. ii Acknowledgments Completing a PhD is truly a marathon event, and I would not have able to complete this journey without the aid and support of countless people over the past seven years. First and foremost I would like to gratefully and sincerely thank my supervisor Dr. Thomas W. Moon for his guidance, understanding, friendship, and most importantly, his patience during my graduate studies at University of Ottawa. His mentorship was paramount in providing a well-rounded experience consistent my long-term career goals. He encouraged me not only to be a biologist but also be an instructor and independent thinker. I am not sure many graduate students are given the opportunity to develop their own individuality and self- sufficiency by being allowed to work with such independence. For everything you’ve done for me, Dr. Moon, I thank you. I would like to extend my thanks the Department of Biology at University of Ottawa, especially those members of my doctoral committee for their input, valuable discussions and accessibility. -

Pathophysiology of Adipocyte Defects and Dyslipidemia in HIV Lipodystrophy: New Evidence from Metabolic and Molecular Studies
American Journal of Infectious Diseases 2 (3): 167-172, 2006 ISSN 1553-6203 © 2006 Science Publications Pathophysiology of Adipocyte Defects and Dyslipidemia in HIV Lipodystrophy: New Evidence from Metabolic and Molecular Studies 1,6Ashok Balasubramanyam, 1,6Rajagopal V. Sekhar, 2,3Farook Jahoor 4Henry J. Pownall and 5Dorothy Lewis 1Translational Metabolism Unit, Division of Diabetes, Endocrinology and Metabolism, 2Department of Pediatrics, 3Children’s Nutrition Research Center 4Section of Atherosclerosis and Lipoprotein Metabolism, 5Department of Immunology Baylor College of Medicine; 6Endocrine Service, Ben Taub General Hospital, Houston, Texas Abstract: Despite a burgeoning mass of descriptive information regarding the epidemiology, clinical features, body composition changes, hormonal alterations and dyslipidemic patterns in patients with HIV lipodystrophy syndrome (HLS), the specific biochemical pathways that are dysregulated in the condition and the molecular mechanisms that lead to their dysfunction, remain relatively unexplored. In this paper, we review studies that detail the metabolic basis of the dyslipidemia - specifically, the hypertriglyceridemia - that is the serologic hallmark of HLS and present new data relevant to mechanisms of dyslipidemia in the postprandial state. We also describe preliminary experiments showing that in addition to the well-known effects of highly-active antiretroviral drugs, the functional disruption of adipocytes and preadipocytes by factors intrinsic to HIV-infected immunocytes may play a role in the pathogenesis of HLS. Key words: Triglycerides, cholesterol, lipoprotein lipase, lipolysis, lymphocyte INTRODUCTION Metabolic basis of HLS - studies in the fasting and fed state: Whole body kinetic studies have Characteristics of dyslipidemia and its relationship demonstrated defects in specific lipid metabolic [19-21] to lipodystrophy: A characteristic dyslipidemic pattern pathways in HLS patients in both the fasting and observed in the majority of patients with HLS is fed (25) states.