Laminin-511-E8 Promotes Efficient in Vitro Expansion of Human Limbal
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Human and Mouse CD Marker Handbook Human and Mouse CD Marker Key Markers - Human Key Markers - Mouse
Welcome to More Choice CD Marker Handbook For more information, please visit: Human bdbiosciences.com/eu/go/humancdmarkers Mouse bdbiosciences.com/eu/go/mousecdmarkers Human and Mouse CD Marker Handbook Human and Mouse CD Marker Key Markers - Human Key Markers - Mouse CD3 CD3 CD (cluster of differentiation) molecules are cell surface markers T Cell CD4 CD4 useful for the identification and characterization of leukocytes. The CD CD8 CD8 nomenclature was developed and is maintained through the HLDA (Human Leukocyte Differentiation Antigens) workshop started in 1982. CD45R/B220 CD19 CD19 The goal is to provide standardization of monoclonal antibodies to B Cell CD20 CD22 (B cell activation marker) human antigens across laboratories. To characterize or “workshop” the antibodies, multiple laboratories carry out blind analyses of antibodies. These results independently validate antibody specificity. CD11c CD11c Dendritic Cell CD123 CD123 While the CD nomenclature has been developed for use with human antigens, it is applied to corresponding mouse antigens as well as antigens from other species. However, the mouse and other species NK Cell CD56 CD335 (NKp46) antibodies are not tested by HLDA. Human CD markers were reviewed by the HLDA. New CD markers Stem Cell/ CD34 CD34 were established at the HLDA9 meeting held in Barcelona in 2010. For Precursor hematopoetic stem cell only hematopoetic stem cell only additional information and CD markers please visit www.hcdm.org. Macrophage/ CD14 CD11b/ Mac-1 Monocyte CD33 Ly-71 (F4/80) CD66b Granulocyte CD66b Gr-1/Ly6G Ly6C CD41 CD41 CD61 (Integrin b3) CD61 Platelet CD9 CD62 CD62P (activated platelets) CD235a CD235a Erythrocyte Ter-119 CD146 MECA-32 CD106 CD146 Endothelial Cell CD31 CD62E (activated endothelial cells) Epithelial Cell CD236 CD326 (EPCAM1) For Research Use Only. -
Corneal Cell Therapy: with Ipscs, It Is No More a Far-Sight Koushik Chakrabarty1* , Rohit Shetty2 and Arkasubhra Ghosh1
Chakrabarty et al. Stem Cell Research & Therapy (2018) 9:287 https://doi.org/10.1186/s13287-018-1036-5 REVIEW Open Access Corneal cell therapy: with iPSCs, it is no more a far-sight Koushik Chakrabarty1* , Rohit Shetty2 and Arkasubhra Ghosh1 Abstract Human-induced pluripotent stem cells (hiPSCs) provide a personalized approach to study conditions and diseases including those of the eye that lack appropriate animal models to facilitate the development of novel therapeutics. Corneal disease is one of the most common causes of blindness. Hence, significant efforts are made to develop novel therapeutic approaches including stem cell-derived strategies to replace the diseased or damaged corneal tissues, thus restoring the vision. The use of adult limbal stem cells in the management of corneal conditions has been clinically successful. However, its limited availability and phenotypic plasticity necessitate the need for alternative stem cell sources to manage corneal conditions. Mesenchymal and embryonic stem cell-based approaches are being explored; nevertheless, their limited differentiation potential and ethical concerns have posed a significant hurdle in its clinical use. hiPSCs have emerged to fill these technical and ethical gaps to render clinical utility. In this review, we discuss and summarize protocols that have been devised so far to direct differentiation of human pluripotent stem cells (hPSCs) to different corneal cell phenotypes. With the summarization, our review intends to facilitate an understanding which would allow developing efficient and robust protocols to obtain specific corneal cell phenotype from hPSCs for corneal disease modeling and for the clinics to treat corneal diseases and injury. Keywords: Cornea, Induced pluripotent stem cells, Differentiation, Disease modeling, Cell replacement therapy Background using viral vectors. -

Selective Expansion of Limbal Epithelial Stem Cells in Culture Using Hypoxia
1 Selective Expansion of Limbal Epithelial Stem Cells in Culture Using Hypoxia Chris Bath1,2, Sufang Yang2,3, Danson Muttuvelu1, Trine Fink2, Jeppe Emmersen2, Henrik Vorum1, Jesper Hjortdal4 and Vladimir Zachar2 1Department of Ophthalmology, Aalborg University Hospital, 9000 Denmark 2Laboratory for Stem Cell Research, Aalborg University, Fredrik Bajers Vej 3B, 9220 Aalborg, Denmark 3Animal Reproduction Institute, Guangxi University, China 4Department of Ophthalmology, Aarhus University Hospital, 8000 Aarhus, Denmark Abstract Limbal epithelial stem cells (LESCs) maintain the corneal epithelium through- out life and are crucial for both corneal integrity and vision. In this study, LESCs were expanded in either a culture system using 3T3 feeder cells in growth medium supplemented with serum, or in a culture system without feeder cells using commercially available serum-free medium (EpiLife). Cells were maintained at an ambient oxygen concentration of 20% or at various levels of hypoxia (15%, 10%, 5%, and 2%) throughout the period of expansion. The effect of ambient oxygen concentration on growth, cell cycle, colony forming efficiency (CFE), and expression of stem cell markers ABCG2 and p63α and differentiation marker CK3 were determined at different time points. Low oxygen levels were found to maintain a stem cell phenotype with low proliferative rate, high CFE, and high expression of ABCG2 and p63α as well as low expression of CK3. The relation between degree of differentiation and ambient oxygen concentration in the culture system seems to mirror the natural environment of the limbal niche. Hypoxic culture could therefore potentially improve stem cell grafts for cultured limbal epithelial transplantation (CLET). 1 2 Selective Expansion of Limbal Epithelial Stem Cells in Culture Using Hypoxia Keywords: Limbus cornea, Adult stem cells, Regenerative medicine, Cell hypoxia, Primary cell culture. -
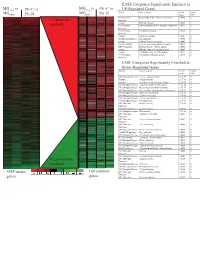
Supplement 1 Microarray Studies
EASE Categories Significantly Enriched in vs MG vs vs MGC4-2 Pt1-C vs C4-2 Pt1-C UP-Regulated Genes MG System Gene Category EASE Global MGRWV Pt1-N RWV Pt1-N Score FDR GO Molecular Extracellular matrix cellular construction 0.0008 0 110 genes up- Function Interpro EGF-like domain 0.0009 0 regulated GO Molecular Oxidoreductase activity\ acting on single dono 0.0015 0 Function GO Molecular Calcium ion binding 0.0018 0 Function Interpro Laminin-G domain 0.0025 0 GO Biological Process Cell Adhesion 0.0045 0 Interpro Collagen Triple helix repeat 0.0047 0 KEGG pathway Complement and coagulation cascades 0.0053 0 KEGG pathway Immune System – Homo sapiens 0.0053 0 Interpro Fibrillar collagen C-terminal domain 0.0062 0 Interpro Calcium-binding EGF-like domain 0.0077 0 GO Molecular Cell adhesion molecule activity 0.0105 0 Function EASE Categories Significantly Enriched in Down-Regulated Genes System Gene Category EASE Global Score FDR GO Biological Process Copper ion homeostasis 2.5E-09 0 Interpro Metallothionein 6.1E-08 0 Interpro Vertebrate metallothionein, Family 1 6.1E-08 0 GO Biological Process Transition metal ion homeostasis 8.5E-08 0 GO Biological Process Heavy metal sensitivity/resistance 1.9E-07 0 GO Biological Process Di-, tri-valent inorganic cation homeostasis 6.3E-07 0 GO Biological Process Metal ion homeostasis 6.3E-07 0 GO Biological Process Cation homeostasis 2.1E-06 0 GO Biological Process Cell ion homeostasis 2.1E-06 0 GO Biological Process Ion homeostasis 2.1E-06 0 GO Molecular Helicase activity 2.3E-06 0 Function GO Biological -

Binding of Recombinant Human Cytokeratin 19 to Laminin
CELL STRUCTURE AND FUNCTION 25: 171–175 (2000) © 2000 by Japan Society for Cell Biology Binding of Recombinant Human Cytokeratin 19 to Laminin: A Possible Role in Interaction between Intermediate Filament Derived from Epithelial Cells and Extracellular Matrixes Naomi Dobashi1, Jiro Fujita1,*, Masayuki Murota2, Yuji Ohtsuki3, Shuji Bandoh1, Yutaka Ueda1, Kazutaka Dohmoto1, Satoko Hojo1, Mikio Nishioka2, Toshihiko Ishida, and Jiro Takahara1 1First Department of Internal Medicine, Kagawa Medical University, Kagawa 2Third Department of Internal Medicine, Kagawa Medical University, Kagawa 3Department of Pathology, Kochi Medical School, Kochi, Japan ABSTRACT. Cytokeratin 8 (CK8) and cytokeratin 19 (CK19) is a specific cytoskeletal component of simple epi- thelia, including bronchial epithelial cells. We hypothesized that CK8 or CK19 released from epithelial cells may bind to and cause damage to extracellular matrixes through binding of anti-CK8 or anti-CK19 autoantibodies. In the present study, bindings of recombinant human CK8 and CK19 to laminin (both derived from mouse sarcoma cells and human), collagen, gelatin, and fibronectin were evaluated by a modified enzyme-linked immunosorbent assay (ELISA). In addition, binding of CK19 to laminin was also confirmed by inhibition assay. As a result, CK19 strongly bound to mouse laminin as well as human laminin. Pretreatment with laminin significantly reduced the binding of CK19 to laminin. However, binding of recombinant CK19 to laminin was not demonstrated by Western immunoblot, suggesting that SDS treatment of laminin diminished the binding. These results suggest that released CK19 from epithelial cells may have played a role in the damage of basement membrane by accumulation of an immune complex composed by CK19 and anti-CK19 autoantibody. -

Congenital Muscular Dystrophy Due to Laminin Α2 (Merosin) Deficiency (MDC1A) in an Ethnic Malay Girl 1MK Thong, 3Sofiah Ali,4 YE Park, 5DS Kim, 6KJ Goh, 2KT Wong
Neurology Asia 2017; 22(2) : 155 – 159 Congenital muscular dystrophy due to laminin α2 (merosin) deficiency (MDC1A) in an ethnic Malay girl 1MK Thong, 3Sofiah Ali, 4YE Park, 5DS Kim, 6KJ Goh, 2KT Wong 1Departments of Paediatrics, 2Pathology and 6Medicine, Faculty of Medicine, University of Malaya, Kuala Lumpur, Malaysia; 3Sime Darby Medical Centre, Subang Jaya, Selangor, Malaysia; 4Department of Neurology and Biomedical Research Institute, Pusan National University Hospital, Busan, Korea; 5Department of Neurology, Research Institute for Convergence of Biomedical Science and Technology, Pusan National University Yangsan Hospital, Yangsan, Korea Abstract We report the first known ethnic Malay patient with laminin alpha-2 (merosin) deficiency (MDC1A), a subtype of congenital muscular dystrophy (CMD)as a result of novel LAMA2 gene mutations. The 21-month-old female presented with hypotonia at birth and gross motor delay of her distal lower limbs. Physical examination showed generalised hypotonia, hyporeflexia and myopathic facies but good cognitive functions. Serum creatine kinase was elevated and white matter changes were detected in the brain MRI. Muscle biopsy showed dystrophic changes with complete laminin α2 deficiency by immunohistochemistry. Mutation analysis of LAMA2 showed compound heterozygote at exon 21, c.2888delG(p.Gly963Alafs*111) and exon 34, c.4886dupC(p.Pro1629Profs*40) leading to premature stop codon for each of the frameshift mutations. Patient review at seven years of age showed satisfactory cognitive functions despite having contractures and weakness. Genetic testing of LAMA2 related muscular dystrophy facilitated the earlier diagnosis of MDC1A and genetic counselling for this family. Keywords: laminin alpha-2 deficiency; merosin deficiency. LAMA2, Malaysia, congenital muscular dystrophy, MDC1A INTRODUCTION mutations in the laminin alpha-2 (LAMA2)gene. -

Methylation of the NT5E Gene Is Associated with Poor Prognostic Factors in Breast Cancer
diagnostics Article Methylation of the NT5E Gene Is Associated with Poor Prognostic Factors in Breast Cancer Young Ju Jeong 1,* , Hoon Kyu Oh 2 , Hye Ryeon Choi 3 and Sung Hwan Park 1 1 Department of Surgery, Catholic University of Daegu School of Medicine, Daegu 42471, Korea; [email protected] 2 Department of Pathology, Catholic University of Daegu School of Medicine, Daegu 42471, Korea; [email protected] 3 Department of Thyroid and Endocrine Surgery, Thyroid Cancer Center, Severance Hospital, Yonsei University College of Medicine, Seoul 03722, Korea; [email protected] * Correspondence: [email protected]; Tel.: +82-53-560-4875 Received: 8 October 2020; Accepted: 11 November 2020; Published: 12 November 2020 Abstract: Cluster of differentiation (CD) 73, which is encoded by the NT5E gene, regulates production of immunosuppressive adenosine and is an emerging checkpoint in cancer immunotherapy. Despite the significance of CD73 in immuno-oncology, the roles of the NT5E gene methylation in breast cancer have not been well-defined yet. Therefore, we aimed to investigate the prognostic significance of the NT5E gene methylation in breast cancer. The DNA methylation status of the NT5E gene was analyzed using pyrosequencing in breast cancer tissues. In addition, the levels of inflammatory markers and lymphocyte infiltration were evaluated. The mean methylation level of the NT5E gene was significantly higher in breast cancer than in normal breast tissues. In the analysis of relevance with clinicopathologic characteristics, the mean methylation levels of the NT5E gene were significantly higher in patients with large tumor size, high histologic grade, negative estrogen receptor expression, negative Bcl-2 expression, and premenopausal women. -

Induced Pluripotent Stem Cells As a Potential Therapeutic Source for Corneal Epithelial Stem Cells
iPSCs for corneal diseases ·Review· Induced pluripotent stem cells as a potential therapeutic source for corneal epithelial stem cells Jie Zhu1, Mark Slevin2,3, Bao-Qiang Guo2,3, Shou-Rong Zhu4 1Queen Mary School, Medical College of Nanchang Citation: Zhu J, Slevin M, Guo BQ, Zhu SR. Induced pluripotent University, Nanchang 330006, Jiangxi Province, China stem cells as a potential therapeutic source for corneal epithelial stem 2School of Healthcare Science, Faculty of Science and cells. Int J Ophthalmol 2018;11(12):2004-2010 Engineering, Manchester Metropolitan University, Chester Street, Manchester M15GD, United Kingdom INTRODUCTION 3Research Institute of Brain Vascular Disease, Weifang Medical luripotent stem cells are primitive cells that are able University, Weifang 261000, Shandong Province, China P to be self-renewing, proliferating indefinitely in their 4Department of Ophthalmology, Affiliated Hospital of Weifang undifferentiated state, and differentiate into different cell [1-2] Medical University, Weifang 261000, Shandong Province, types . They can efficiently differentiate into specific cell China types under defined conditions. Therefore, stem cells have Correspondence to: Bao-Qiang Guo. Research Institute of been regarded as unlimited source of cell transplantation. Brain Vascular Disease, Weifang Medical University, Weifang Over the last decade, stem or progenitor cells transplantation 261000, Shandong Province, China. [email protected]; as a means of replacing tissue have evolved rapidly. There are Shou-Rong Zhu. Department of Ophthalmology, Affiliated distinct kinds of stem cells according to their differentiation Hospital of Weifang Medical University, Weifang 261000, potential. It has already been found that embryonic stem cells Shandong Province, China. [email protected]. (ESCs) and mesenchymal stem cells (MSCs) can directly Received: 2018-08-21 Accepted: 2018-10-12 differentiate into specialized cells, which attracted considerable interest. -

CD Markers Are Routinely Used for the Immunophenotyping of Cells
ptglab.com 1 CD MARKER ANTIBODIES www.ptglab.com Introduction The cluster of differentiation (abbreviated as CD) is a protocol used for the identification and investigation of cell surface molecules. So-called CD markers are routinely used for the immunophenotyping of cells. Despite this use, they are not limited to roles in the immune system and perform a variety of roles in cell differentiation, adhesion, migration, blood clotting, gamete fertilization, amino acid transport and apoptosis, among many others. As such, Proteintech’s mini catalog featuring its antibodies targeting CD markers is applicable to a wide range of research disciplines. PRODUCT FOCUS PECAM1 Platelet endothelial cell adhesion of blood vessels – making up a large portion molecule-1 (PECAM1), also known as cluster of its intracellular junctions. PECAM-1 is also CD Number of differentiation 31 (CD31), is a member of present on the surface of hematopoietic the immunoglobulin gene superfamily of cell cells and immune cells including platelets, CD31 adhesion molecules. It is highly expressed monocytes, neutrophils, natural killer cells, on the surface of the endothelium – the thin megakaryocytes and some types of T-cell. Catalog Number layer of endothelial cells lining the interior 11256-1-AP Type Rabbit Polyclonal Applications ELISA, FC, IF, IHC, IP, WB 16 Publications Immunohistochemical of paraffin-embedded Figure 1: Immunofluorescence staining human hepatocirrhosis using PECAM1, CD31 of PECAM1 (11256-1-AP), Alexa 488 goat antibody (11265-1-AP) at a dilution of 1:50 anti-rabbit (green), and smooth muscle KD/KO Validated (40x objective). alpha-actin (red), courtesy of Nicola Smart. PECAM1: Customer Testimonial Nicola Smart, a cardiovascular researcher “As you can see [the immunostaining] is and a group leader at the University of extremely clean and specific [and] displays Oxford, has said of the PECAM1 antibody strong intercellular junction expression, (11265-1-AP) that it “worked beautifully as expected for a cell adhesion molecule.” on every occasion I’ve tried it.” Proteintech thanks Dr. -

SOX9 Keeps Growth Plates and Articular Cartilage Healthy by Inhibiting Chondrocyte Dedifferentiation/ Osteoblastic Redifferentiation
SOX9 keeps growth plates and articular cartilage healthy by inhibiting chondrocyte dedifferentiation/ osteoblastic redifferentiation Abdul Haseeba,1, Ranjan Kca,1, Marco Angelozzia, Charles de Charleroya, Danielle Ruxa, Robert J. Towerb, Lutian Yaob, Renata Pellegrino da Silvac, Maurizio Pacificia, Ling Qinb, and Véronique Lefebvrea,2 aDivision of Orthopaedic Surgery, Children’s Hospital of Philadelphia, Philadelphia, PA 19104; bDepartment of Orthopaedic Surgery, University of Pennsylvania, Philadelphia, PA 19104; and cCenter for Applied Genomics, Children’s Hospital of Philadelphia, Philadelphia, PA 19104 Edited by Denis Duboule, University of Geneva, Geneva, Switzerland, and approved January 13, 2021 (received for review September 19, 2020) Cartilage is essential throughout vertebrate life. It starts develop- The skeleton is a model system to study cell fate and differ- ing in embryos when osteochondroprogenitor cells commit to entiation mechanisms. It arises developmentally from multi- chondrogenesis, activate a pancartilaginous program to form carti- potent mesenchymal cells, often called osteochondroprogenitors. laginous skeletal primordia, and also embrace a growth-plate pro- Guided by spatiotemporal cues, these cells commit to chondro- gram to drive skeletal growth or an articular program to build genesis or osteoblastogenesis to build cartilage or bone, respec- permanent joint cartilage. Various forms of cartilage malformation tively (5–7). Cartilage exists in several forms. Articular cartilage and degeneration diseases afflict humans, but underlying mecha- (AC) is a mostly resting tissue that protects opposing bone ends nisms are still incompletely understood and treatment options sub- in synovial joints throughout life, whereas growth plates (GPs) optimal. The transcription factor SOX9 is required for embryonic are transient, dynamic structures that drive skeletal growth while chondrogenesis, but its postnatal roles remain unclear, despite evi- being gradually replaced by bone (endochondral ossification). -

Blood Vitronectin Is a Major Activator of LIF and IL-6 in the Brain Through Integrin–FAK and Upar Signaling Matthew P
© 2018. Published by The Company of Biologists Ltd | Journal of Cell Science (2018) 131, jcs202580. doi:10.1242/jcs.202580 RESEARCH ARTICLE Blood vitronectin is a major activator of LIF and IL-6 in the brain through integrin–FAK and uPAR signaling Matthew P. Keasey1, Cuihong Jia1, Lylyan F. Pimentel1,2, Richard R. Sante1, Chiharu Lovins1 and Theo Hagg1,* ABSTRACT Microglia and astrocytes express the VTN receptors αvβ3 and α β We defined how blood-derived vitronectin (VTN) rapidly and potently v 5 integrin (Herrera-Molina et al., 2012; Kang et al., 2008; activates leukemia inhibitory factor (LIF) and pro-inflammatory Milner, 2009; Welser-Alves et al., 2011). Microglia and astrocytes, interleukin 6 (IL-6) in vitro and after vascular injury in the brain. as well as endothelial cells, are major producers of pro- α in vitro Treatment with VTN (but not fibrinogen, fibronectin, laminin-111 or inflammatory cytokines, such as IL-6 and TNF , and collagen-I) substantially increased LIF and IL-6 within 4 h in after traumatic or ischemic injury to the brain (Banner et al., 1997; C6-astroglioma cells, while VTN−/− mouse plasma was less effective Erta et al., 2012; Lau and Yu, 2001) or upon self-induction by IL-6 than that from wild-type mice. LIF and IL-6 were induced by (Van Wagoner and Benveniste, 1999). IL-6 is a major regulator of a intracerebral injection of recombinant human (rh)VTN in mice, but variety of inflammatory disorders and a target for therapies (Hunter induction seen upon intracerebral hemorrhage was less in VTN−/− and Jones, 2015). -

Transcriptomic and Proteomic Profiling Provides Insight Into
BASIC RESEARCH www.jasn.org Transcriptomic and Proteomic Profiling Provides Insight into Mesangial Cell Function in IgA Nephropathy † † ‡ Peidi Liu,* Emelie Lassén,* Viji Nair, Celine C. Berthier, Miyuki Suguro, Carina Sihlbom,§ † | † Matthias Kretzler, Christer Betsholtz, ¶ Börje Haraldsson,* Wenjun Ju, Kerstin Ebefors,* and Jenny Nyström* *Department of Physiology, Institute of Neuroscience and Physiology, §Proteomics Core Facility at University of Gothenburg, University of Gothenburg, Gothenburg, Sweden; †Division of Nephrology, Department of Internal Medicine and Department of Computational Medicine and Bioinformatics, University of Michigan, Ann Arbor, Michigan; ‡Division of Molecular Medicine, Aichi Cancer Center Research Institute, Nagoya, Japan; |Department of Immunology, Genetics and Pathology, Uppsala University, Uppsala, Sweden; and ¶Integrated Cardio Metabolic Centre, Karolinska Institutet Novum, Huddinge, Sweden ABSTRACT IgA nephropathy (IgAN), the most common GN worldwide, is characterized by circulating galactose-deficient IgA (gd-IgA) that forms immune complexes. The immune complexes are deposited in the glomerular mesangium, leading to inflammation and loss of renal function, but the complete pathophysiology of the disease is not understood. Using an integrated global transcriptomic and proteomic profiling approach, we investigated the role of the mesangium in the onset and progression of IgAN. Global gene expression was investigated by microarray analysis of the glomerular compartment of renal biopsy specimens from patients with IgAN (n=19) and controls (n=22). Using curated glomerular cell type–specific genes from the published literature, we found differential expression of a much higher percentage of mesangial cell–positive standard genes than podocyte-positive standard genes in IgAN. Principal coordinate analysis of expression data revealed clear separation of patient and control samples on the basis of mesangial but not podocyte cell–positive standard genes.