Corneal Cell Therapy: with Ipscs, It Is No More a Far-Sight Koushik Chakrabarty1* , Rohit Shetty2 and Arkasubhra Ghosh1
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Aging and the Cornea
814 British Journal of Ophthalmology 1997;81:814–817 Br J Ophthalmol: first published as 10.1136/bjo.81.10.814 on 1 October 1997. Downloaded from BRIEF REVIEWS ON ASPECTS OF AGING AND THE EYE Aging and the cornea RGAFaragher, B Mulholland, S J Tuft, S Sandeman, P T Khaw Aging, the persistent decline in age specific fitness of an also known as contact inhibition. Rather confusingly, both organism as a result of internal physiological deterioration, senescence and quiescence are referred to as the G0 phase is a common process among multicellular organisms.1 In of the cell cycle (sometimes more helpfully distinguished as humans, aging is usually monitored in relation to time, G0Q and G0S).15 Senescence is also distinct from cell which renders it diYcult to diVerentiate between time death, occurring either by apoptosis or necrosis, and it is dependent biological changes and damage from environ- not a form of terminal diVerentiation.16 17 The phenotypes mental insults. There are essentially three types of aging at of growth and senescence are totally distinct cell cycle work in any adult tissue; the aging of long lived proteins, compartments; there is no such thing as a half senescent the aging of dividing cells, and the aging of non-dividing cell. Cells that enter replicative senescence acquire two cells.2 Dividing cells may be derived from renewing popu- phenotypes: they leave the cell cycle with a G1 DNA lations in which the rate of cell loss and division is great. An content,18 and they undergo a characteristic series of example is the corneal epithelium in which complete changes in biology and gene expression that alters the turnover occurs within 5–7 days after terminal function of the cell.13 19 In this latter situation some genes diVerentiation.34 Conditional renewal populations, which are transcriptionally repressed, some gene expression is normally have an extremely low proliferation rate, can also upregulated, and some totally senescent specific genes are produce dividing cells in response to extrinsic stimuli. -

Selective Expansion of Limbal Epithelial Stem Cells in Culture Using Hypoxia
1 Selective Expansion of Limbal Epithelial Stem Cells in Culture Using Hypoxia Chris Bath1,2, Sufang Yang2,3, Danson Muttuvelu1, Trine Fink2, Jeppe Emmersen2, Henrik Vorum1, Jesper Hjortdal4 and Vladimir Zachar2 1Department of Ophthalmology, Aalborg University Hospital, 9000 Denmark 2Laboratory for Stem Cell Research, Aalborg University, Fredrik Bajers Vej 3B, 9220 Aalborg, Denmark 3Animal Reproduction Institute, Guangxi University, China 4Department of Ophthalmology, Aarhus University Hospital, 8000 Aarhus, Denmark Abstract Limbal epithelial stem cells (LESCs) maintain the corneal epithelium through- out life and are crucial for both corneal integrity and vision. In this study, LESCs were expanded in either a culture system using 3T3 feeder cells in growth medium supplemented with serum, or in a culture system without feeder cells using commercially available serum-free medium (EpiLife). Cells were maintained at an ambient oxygen concentration of 20% or at various levels of hypoxia (15%, 10%, 5%, and 2%) throughout the period of expansion. The effect of ambient oxygen concentration on growth, cell cycle, colony forming efficiency (CFE), and expression of stem cell markers ABCG2 and p63α and differentiation marker CK3 were determined at different time points. Low oxygen levels were found to maintain a stem cell phenotype with low proliferative rate, high CFE, and high expression of ABCG2 and p63α as well as low expression of CK3. The relation between degree of differentiation and ambient oxygen concentration in the culture system seems to mirror the natural environment of the limbal niche. Hypoxic culture could therefore potentially improve stem cell grafts for cultured limbal epithelial transplantation (CLET). 1 2 Selective Expansion of Limbal Epithelial Stem Cells in Culture Using Hypoxia Keywords: Limbus cornea, Adult stem cells, Regenerative medicine, Cell hypoxia, Primary cell culture. -

Induced Pluripotent Stem Cells As a Potential Therapeutic Source for Corneal Epithelial Stem Cells
iPSCs for corneal diseases ·Review· Induced pluripotent stem cells as a potential therapeutic source for corneal epithelial stem cells Jie Zhu1, Mark Slevin2,3, Bao-Qiang Guo2,3, Shou-Rong Zhu4 1Queen Mary School, Medical College of Nanchang Citation: Zhu J, Slevin M, Guo BQ, Zhu SR. Induced pluripotent University, Nanchang 330006, Jiangxi Province, China stem cells as a potential therapeutic source for corneal epithelial stem 2School of Healthcare Science, Faculty of Science and cells. Int J Ophthalmol 2018;11(12):2004-2010 Engineering, Manchester Metropolitan University, Chester Street, Manchester M15GD, United Kingdom INTRODUCTION 3Research Institute of Brain Vascular Disease, Weifang Medical luripotent stem cells are primitive cells that are able University, Weifang 261000, Shandong Province, China P to be self-renewing, proliferating indefinitely in their 4Department of Ophthalmology, Affiliated Hospital of Weifang undifferentiated state, and differentiate into different cell [1-2] Medical University, Weifang 261000, Shandong Province, types . They can efficiently differentiate into specific cell China types under defined conditions. Therefore, stem cells have Correspondence to: Bao-Qiang Guo. Research Institute of been regarded as unlimited source of cell transplantation. Brain Vascular Disease, Weifang Medical University, Weifang Over the last decade, stem or progenitor cells transplantation 261000, Shandong Province, China. [email protected]; as a means of replacing tissue have evolved rapidly. There are Shou-Rong Zhu. Department of Ophthalmology, Affiliated distinct kinds of stem cells according to their differentiation Hospital of Weifang Medical University, Weifang 261000, potential. It has already been found that embryonic stem cells Shandong Province, China. [email protected]. (ESCs) and mesenchymal stem cells (MSCs) can directly Received: 2018-08-21 Accepted: 2018-10-12 differentiate into specialized cells, which attracted considerable interest. -

Simple Limbal Epithelial Transplantation Method in the Treatment of Unilateral Limbal Stem Cell Deficiency Due to Chemical Burn
DOI: 10.14744/eer.2021.32032 Eur Eye Res 2021;1(1):31–36 ORIGINAL ARTICLE Simple limbal epithelial transplantation method in the treatment of unilateral limbal stem cell deficiency due to chemical burn Dilay Ozek, Emine Esra Karaca, Ozlem Evren Kemer Department of Opthalmology, Ankara City Hospital, Ankara, Turkey Abstract Purpose: The objectives of the study were to evaluate the success of the simple limbal epithelial transplantation (SLET) method in the treatment of unilateral limbal stem cell deficiency (LSCD) due to chemical burn. Methods: Seventeen patients with unilateral LSCD due to chemical burn were included in this retrospective study. Mean age of patients was 50.3±20.8 (28–75) years. Mean duration of follow was 18.9±6.9 (12–24) months. In the recipient eye follow- ing peritomy, pannus tissue was cleared and covered with amniotic membrane with fibrin glue. Limbal stem cell received from the fellow eye was implanted cornea surface 2–3 mm inside limbus with fibrin glue on the amniotic membrane and placed contact lens. In control examination of all patients who completed minimum 12 months postoperatively, regression in corneal vascularization, duration of epithelial healing, visual acuity, need for keratoplasty, and complications (dropping of contact lenses, separation of amniotic membrane, and graft failure) were evaluated. Results: Corneal epithelization was completed between 4 and 6 weeks in all patients. Total and partial separations in the amniotic membrane occurred in two patients. Marked regression in corneal vascularization and increase in visual acuity was observed in all patients. Five patients (29.4%) underwent keratoplasty in the follow-up period. -

J·-·. Universidad
Universidad ,.,. I ::::.�j:.� �·-·. :::t.,.•• de Alcala COMISIÓN DE ESTUDIOS OFICIALES DE POSGRADO Y DOCTORADO ACTA DE EVALUACIÓN DE LA TESIS DOCTORAL Año académico 2016/17 DOCTORANDO: RODRÍGUEZ PÉREZ, MARÍA ISABEL D.N.1./PASAPORTE: ****779T PROGRAMA DE DOCTORADO: D325 DOCTORADO EN CIENCIAS DE LA SALUD DEPARTAMENTO DE: CIRUGÍA, CIENCIAS MÉDICAS Y SOCIALES TITULACIÓN DE DOCTOR EN: DOCTOR/A POR LA UNIVERSIDAD DE ALCALÁ En el día de hoy 13/09/17, reunido el tribunal de evaluación nombrado por la Comisión de Estudios Oficiales de Posgrado y Doctorado de la Universidad y constituido por los miembros que suscriben la presente Acta, el aspirante defendió su Tesis Doctoral, elaborada bajo la dirección de MIGUEL ÁNGEL TESUS GUEZALA // JUAN GROS OTERO. o < -o Sobre el siguiente tema: SEGURIDAD, EFICACIA Y PREDICTIBILIDAD EN CIGURÍA CON LÁSER EXCIMER: LASIK z MECÁNICO, LASIK FEMTOSEGUNDOY LASEK < ::,; ::, :,: Finalizada la defensa y discusión de la tesis, el tribunal acordó otorgar la CALIFICACIÓN GLOBAL6 de (no apto, < ..J aprobado, notable y sobresaliente): ____5 _t0_S_�_'.f,_o_(/2_�_1C___________ ____ o"' o z o ::,; Alcalá de Henares, .. Á.J..... de .. ?.fp.h...�-�- de _'!:-:!__1)- -< ..J< u ..J< "' EL PRESIDENTE EL SECRETARIO EL VOCAL o o < o "'- """' > z ::, Con fccha_� __ dc_�e.___de � lTia Comisión Delegada de la Comisión de Estudios Oficialesde Posgrado, a la vista de los votos emitidos de manera anónima por el tribunal que ha juzgado la tesis, resuelve: � Conceder la Mención de "Cum Laude" O No conceder la Mención de "Cum Laude" La Secretariade la Comisión Delegada 6 La calificación podrá ser "no apto" "aprobado" "notable" y "sobresaliente". -

Current Perspectives on Tissue Engineering for the Management of Limbal Stem Cell Deficiency
Open Access Journal of Stem Cells Research, Reviews & Reports Review Article Current Perspectives on Tissue Engineering for the Management of Limbal Stem Cell Deficiency Bakiah Shaharuddin1,2* and Annette Meeson2 1Advanced Medical and Dental Institute, Universiti Sains Abstract Malaysia, Malaysia Limbal Stem Cell Deficiency (LSCD) encompasses a group of eye disorders 2Institute of Genetic Medicine, Faculty of Medical characterized by abnormal maintenance of the limbal stem cells. This painful Sciences, Newcastle University, UK and potentially blinding condition poses a challenge in transplantation biology; *Corresponding author: Bakiah Shaharuddin, whereby whole corneal transplantation would normally fail due to the depletion of Advanced Medical and Dental Institute, Universiti Sains the recipients’ limbal stem cells. The most preferred technique of management is Malaysia, Kepala Batas, 13200 Pulau Pinang, Malaysia transplantation of ex vivo expanded limbal stem cells to the damaged eyes. This and Institute of Genetic Medicine, Newcastle University, article discusses the therapy options for unilateral and bilateral cases of LSCD, International Centre for Life, Newcastle Upon-Tyne, NE1 the clinical outcomes, components of cells and substrates that are currently 3BZ, UK; Email: [email protected] being investigated or have been utilized by this technique, and brings into focus the newer therapy of using a scaffold-free cell delivery system to treat LSCD. Received: June 15, 2015; Accepted: October 01, 2015; Published: October 08, 2015 Keywords: Limbal stem cells; Limbal stem cell deficiency; Tissue engineering; Cell sheet Abbreviations i.e Steven-Johnson syndrome, ocular cicatricial phemphigoid and chronic limbitis. Trauma, surgery and cryotherapy to the limbus, AM: Amniotic Membrane; BM: Bone Marrow; EGF: Epidermal radiation and topical instillation or subconjunctival injection of toxic Growth Factor; ECM: Extracellular Matrix; ESC: Embryonic Stem drugs are some iatrogenic causes. -

View the Abstracts
SPECIAL TALKS 29 th July, 2018 ST3 KERATOCONUS INTERNATIONAL CONSORTIUM TO COMBAT THE NEED FOR CORNEAL TRANSPLANTATION Srujana Sahebjada University of Melbourne, Melbourne, Victoria, Australia. Keratoconus is a devastating and potentially blinding eye disease affecting 1 in 375 people. It is typically diagnosed during early teenage years and has a significant lifetime burden on an individual. While corneal cross-linking treatment is now available to slow disease progression, poor outcomes still persist due to delay in diagnosis or treatment, or other unknown factors that can ultimately lead to the need for corneal transplantation. Our research team has conducted a pilot study wherein we have recruited 400 subjects from public and private clinics in Melbourne to begin to address these issues. As a result, we have obtained extensive knowledge regarding a range of biomarkers from clinical features, imaging and genetic through to studying its impact on quality of life, economic burden, risk factors and treatment modalities. To take this research further, we established Keratoconus international consortium (KIC), with the main aim to produce a more streamlined and concerted effort for better understanding the condition and ultimately curing keratoconus. This global collaborative initiative is a game-changer- with already on board 15 national and international corneal specialists, willing to collect and share data and thus contribute to expanding our knowledge about keratoconus. KIC will be a first worldwide study in KC that will allow us to undertake a unified analysis to enable better diagnosis of individuals at early risk of disease, explore a therapeutic algorithm, identify biomarkers to be targeted for future therapy and thus potentially avoiding graft surgery. -

CVN De FECYT Fecha Del Documento: 15/01/2020 V 1.4.0 733513B2ee09064ccf5bd412636c83db
Miguel Angel Teus Guezala Generado desde: Editor CVN de FECYT Fecha del documento: 15/01/2020 v 1.4.0 733513b2ee09064ccf5bd412636c83db Este fichero electrónico (PDF) contiene incrustada la tecnología CVN (CVN-XML). La tecnología CVN de este fichero permite exportar e importar los datos curriculares desde y hacia cualquier base de datos compatible. Listado de Bases de Datos adaptadas disponible en http://cvn.fecyt.es/ 733513b2ee09064ccf5bd412636c83db Resumen libre del currículum Descripción breve de la trayectoria científica, los principales logros científico-técnicos obtenidos, los intereses y objetivos científico-técnicos a medio/largo plazo de la línea de investigación. Incluye también otros aspectos o peculiaridades importantes. Catedrático de Universidad del área de conocimiento de Oftalmología, adscrito al Departamento de Cirugía de la Facultad de Medicina de la Universidad de Alcalá. Patrono de la Fundación de Investigación Biomédica del Hospital Príncipe de Asturias, desde 2005. Coordinador del grado de optometría en el centro CUNIMAD, adscrito a la UAH (desde julio 2019). Su trayectoria investigadora se orienta en torno a tres líneas principales: Cirugía refractiva láser corneal, biomecánica corneal y el glaucoma. Ha participado en múltiples proyectos de investigación, entre sus publicaciones destaca la producción en artículos en revistas internacionales y los capítulos de libro editados por instituciones y editoriales de reconocido prestigio internacional, como es el caso de la Agencia Laín Entralgo de la Comunidad de Madrid o Elsevier. Es miembro evaluador de trabajos científicos de diversas revistas nacionales e internacionales. Ha dirigido un total de 29 Tesis Doctorales (entre los años 2003 a 2019). Ha sido director externo en el Máster Universitario en Optometría Clínica de la Universidad Europea de Madrid. -

Long-Term Results of Allogenic Penetrating Limbo-Keratoplasty
Eye (2017) 31, 372–378 © 2017 Macmillan Publishers Limited, part of Springer Nature. All rights reserved 0950-222X/17 www.nature.com/eye 1 1 2 CLINICAL STUDY Long-term results of SJ Lang , D Böhringer , G Geerling and T Reinhard1 allogenic penetrating limbo-keratoplasty: 20 years of experience Abstract Aim The objective of the study was to in the case of conjunctivalization of the visual evaluate the long-term results of allogenic axis. This may restore a clear corneal centre in penetrating limbo-keratoplasy. This method those cases without the need for stem cells. allows simultaneous transplantation of a Amniotic membrane transplantation is an corneal graft and limbal stem cells of the additional method.3 Total failure of the limbal donor by means of eccentric trephination of stem cells results in severe alteration of the the donor button. corneal surface, and may lead to complete Method The data of 192 consecutive cases of conjunctivalisation of the cornea, with recurrent allogenic penetrating limbo-keratoplasty from ulcerations.4 This results in corneal opacification 1995 to 2015 were reviewed. These had been and visual impairment. There are a multitude of performed exclusively in eyes with complete causes for complete limbal stem cell failure. failure of the limbal stem cells, in Chemical burns can produce severe damage to combination with deep corneal scarring. the corneal limbus, the corneal stroma, and the Indications were predominantly eye burns, anterior ocular segment. Thus, the degree of fl in ammatory conditions, and congenital ischemia and necrosis in limbus, conjunctiva, aniridia. Graft survival and rejection rates and sclera may permit the estimation of the – were assessed using Kaplan Meier analysis. -

The Stroma and Keratoconus: a Review
S Afr Optom 2007 66(3) 87-93 The stroma and keratoconus: a review WDH Gillan* Optometric Science Research Group, Department of Optometry, University of Johannesburg, PO Box 524, Auckland Park, 2006 South Africa <[email protected]> Introduction The cornea is the transparent anterior portion of the fibrous coat of the eye1. In humans the cornea averages 0.52 mm in thickness centrally thickening to 0.65 mm in the periphery2-5. The human cornea consists of five layers: the epithelium, Bowman’s membrane, the stroma, Descemets’s membrane and the endothelium2-5. The stroma makes up approximately 90% of the thickness of the cornea and is the major structural component. The cornea’s strength, shape and transparency can be attributed to the anatomic and metabolic properties of the stroma3, 4. The stroma consists of collagen, glycosaminoglycans, keratocytes and nerves. Two to three percent of the stroma consists of cellular components (keratocytes). Collagen makes up approximately 70% of the dry weight of the cornea. Type I collagen makes up the majority of the collagen in the stroma with types III, IV and VI also being present4. Keratoconus is a developmental or dystrophic deformity of the cornea in which it becomes cone-shaped due to thinning and stretching of the tissue in its central area1. Depending on the diagnostic criteria used, keratoconus has a prevalence between 50 and 230 people per 100 000.4 Keratoconus occurs in all races and there is no gender preference4. An association between connective tissue disease and keratoconus has been suggested4. Connective tissue diseases like Ehlers-Danlos syndrome, Marfans’ syndrome, osteogenesis imperfecta, Reiger’s syndrome, among others, have been associated with keratoconus4, 6. -

Quantitative Analysis of Corneal Microstructure in Keratoconus KH Weed Et Al 615
Eye (2007) 21, 614–623 & 2007 Nature Publishing Group All rights reserved 0950-222X/07 $30.00 www.nature.com/eye 1 1 1 CLINICAL STUDY Quantitative KH Weed , CJ MacEwen , A Cox and CNJ McGhee2 analysis of corneal microstructure in keratoconus utilising in vivo confocal microscopy Abstract presence of keratoconus did not affect the endothelial cell density (P ¼ 0.54). Purpose To establish and quantify the in vivo Conclusion In vivo confocal microscopy confocal microscopic features of moderate to can provide insight into the microstructural advanced keratoconus. changes that occur in keratoconus. Methods Nineteen keratoconus subjects were Eye (2007) 21, 614–623. doi:10.1038/sj.eye.6702286; catergorised using Orbscan-derived corneal published online 24 February 2006 apex power and pachymetry as exhibiting moderate (n ¼ 7) and advanced (n ¼ 12) Keywords: in vivo confocal microscopy; keratoconus. Control subjects included 23 keratoconus; cornea; contact lens noncontact lens wearers (Group A) and 15 contact lens wearers (Group B). All subjects Introduction underwent Confoscan slit scanning in vivo confocal microscopy. Keratoconus is a noninflammatory corneal Results Compared with Group A ectasia which is usually bilateral and 1 (49127434 cells/mm2), basal epithelial density progressive. The incidence of this ocular 1Ophthalmology was significantly lower in both moderate disease is approximately 1 per 2000 in the 2 Department, Ninewells (45927414 cells/mm2, Po0.05) and advanced general population ; however, the precise 3 Hospital and Medical keratoconus -
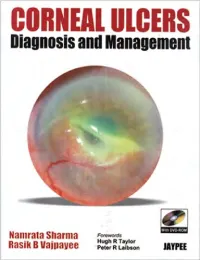
CORNEAL ULCERS Diagnosis and Management
CORNEAL ULCERS Diagnosis and Management System requirement: • Windows XP or above • Power DVD player (Software) • Windows Media Player 10.0 version or above • Quick time player version 6.5 or above Accompanying DVD ROM is playable only in Computer and not in DVD player. Kindly wait for few seconds for DVD to autorun. If it does not autorun then please do the following: • Click on my computer • Click the drive labelled JAYPEE and after opening the drive, kindly double click the file Jaypee CORNEAL ULCERS Diagnosis and Management Namrata Sharma MD DNB MNAMS Associate Professor of Ophthalmology Cornea, Cataract and Refractive Surgery Services Dr. Rajendra Prasad Centre for Ophthalmic Sciences All India Institute of Medical Sciences, New Delhi India Rasik B Vajpayee MS FRCSEd FRANZCO Head, Corneal and Cataract Surgery Centre for Eye Research Australia Royal Victorian Eye and Ear Hospital University of Melbourne Australia Forewords Hugh R Taylor Peter R Laibson ® JAYPEE BROTHERS MEDICAL PUBLISHERS (P) LTD New Delhi • Ahmedabad • Bengaluru • Chennai • Hyderabad • Kochi • Kolkata • Lucknow • Mumbai • Nagpur Published by Jitendar P Vij Jaypee Brothers Medical Publishers (P) Ltd B-3 EMCA House, 23/23B Ansari Road, Daryaganj New Delhi 110 002, India Phones: +91-11-23272143, +91-11-23272703, +91-11-23282021, +91-11-23245672 Rel: +91-11-32558559, Fax: +91-11-23276490, +91-11-23245683 e-mail: [email protected] Visit our website: www.jaypeebrothers.com Branches • 2/B, Akruti Society, Jodhpur Gam Road Satellite Ahmedabad 380 015, Phones: +91-79-26926233,