A Dissertation Entitled Characterization of the Anti-Obesity and Anti-Adipogenic Effects of the Limonoid Prieurianin by Rudel A
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-
PDF Document Created by Pdffiller
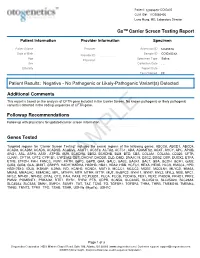
Patient: 1234567843314948-COtGx0053 CLIA ID#: 11D2066426 Larry Hung, MD, Laboratory Director GxTM Carrier Screen Testing Report Patient Information Provider Information Specimen Patient Name Haley Papevies Provider Harbin Clinic Women's Accession ID 1234567843314948 Center Cartersville Date of Birth Apr 16, 1998 Sample ID COtGx0053XX Provider ID 1124488556 Age 19 Specimen Type Saliva Physician Vicki Yates Sex female Collection Date Jul 20, 2017 Ethnicity Report Date Aug 5, 2017 Test Ordered CF Patient Results: Negative - No Pathogenic or Likely-Pathogenic Variant(s) Detected Additional Comments This report is based on the analysis of CFTR gene included in the Carrier Screen. No known pathogenic or likely pathogenic variant(s) detected in the coding sequences of CFTR gene. Followup Recommendations Follow up with physicians for updated carrier screen information. The sequencing for CFTR gene was carried out with the other genes included in the Carrier Screen Testing (listed below). The analysis of the other genes in the Carrier Screen could be ordered through your physicians. Genes Tested Targeted regions for “Carrier Screen Testing” includes the exonic regions of the following genes: ABCC8, ABCD1, ABCD4, ACAD8, ACADM, ACADS, ACADSB, ACADVL, ACAT1, ACSF3, ACTA2, ACTC1, ADA, ADAMTS2, AGXT, AHCY, APC, APOB, ARG1, ASL, ASPA, ASS1, ATP7B, AUH, BCKDHA, BBS2, BCKDHB, BLM, BTD, CBS, COL3A1, COL4A3, CD320, CFTR, CLRN1, CPT1A, CPT2, CYP1B1, CYP21A2, DBT, DHCR7, DHDDS, DLD, DMD, DNAJC19, DSC2, DSG2, DSP, DUOX2, ETFA, ETFB, ETFDH, FAH, FANCC, FBN1, -

Identification of Ataxia-Associated Mtdna Mutations (M.4052T>C And
tapraid5/za3-mus/za3-mus/za300909/za32342d09g knepper1 Sϭ7 7/20/09 11:41 Art: 08-0574 ABSTRACT: The potential pathogenicity of two homoplasmic mtDNA point mu- tations, 9035TϾC and 4452TϾC, found in a family afflicted with maternally trans- mitted cognitive developmental delay, learning disability, and progressive ataxia was evaluated using transmitochondrial cybrids. We confirmed that the 4452TϾC transition in tRNAMet represented a polymorphism; however, 9035TϾC conversion in the ATP6 gene was responsible for a defective F0-ATPase. Accordingly, mutant cybrids had a reduced oligomycin-sensitive ATP hydrolyzing activity. They had less than half of the steady-state content of ATP and nearly an 8-fold higher basal level of reactive oxygen species (ROS). Mutant cybrids were unable to cope with addi- tional insults, i.e., glucose deprivation or tertiary-butyl hydroperoxide, and they succumbed to either apoptotic or necrotic cell death. Both of these outcomes were prevented by the antioxidants CoQ10 and vitamin E, suggesting that the abnormally high levels of ROS were the triggers of cell death. In conclusion, the principal metabolic defects, i.e., energy deficiency and ROS burden, resulted from the 9035TϾC mutation and could be responsible for the development of clinical symp- toms in this family. Furthermore, antioxidant therapy might prove helpful in the management of this disease. Muscle Nerve 39: 000–000, 2009 IDENTIFICATION OF ATAXIA-ASSOCIATED mtDNA MUTATIONS (m.4052T>C and m.9035T>C) AND EVALUATION OF THEIR PATHOGENICITY IN TRANSMITOCHONDRIAL CYBRIDS MARIANNA SIKORSKA, PhD,1 JAGDEEP K. SANDHU, PhD,1 DAVID K. SIMON, MD, PhD,2 VIMUKTHI PATHIRAJA, MD,2 CAROLINE SODJA, MSc,1 YAN LI, MD,1 MARIA RIBECCO-LUTKIEWICZ, PhD,1 PATRICIA LANTHIER, BSc,1 HENRYK BOROWY-BOROWSKI, PhD,1 ADRIAN UPTON, MD, PhD,3 SANDEEP RAHA, PhD,4 STEFAN M. -
Massive Parallel Sequencing As a New Diagnostic Approach For
Chaiyasap et al. BMC Medical Genetics (2017) 18:102 DOI 10.1186/s12881-017-0464-x RESEARCH ARTICLE Open Access Massive parallel sequencing as a new diagnostic approach for phenylketonuria and tetrahydrobiopterin-deficiency in Thailand Pongsathorn Chaiyasap1, Chupong Ittiwut1,2, Chalurmpon Srichomthong1,2, Apiruk Sangsin3, Kanya Suphapeetiporn1,2,4* and Vorasuk Shotelersuk1,2 Abstract Background: Hyperphenylalaninemia (HPA) can be classified into phenylketonuria (PKU) which is caused by mutations in the phenylalanine hydroxylase (PAH) gene, and BH4 deficiency caused by alterations in genes involved in tetrahydrobiopterin (BH4) biosynthesis pathway. Dietary restriction of phenylalanine is considered to be the main treatment of PKU to prevent irreversible intellectual disability. However, the same dietary intervention in BH4 deficiency patients is not as effective, as BH4 is also a cofactor in many neurotransmitter syntheses. Method: We utilized next generation sequencing (NGS) technique to investigate four unrelated Thai patients with hyperphenylalaninemia. Result: We successfully identified all eight mutant alleles in PKU or BH4-deficiency associated genes including three novel mutations, one in PAH and two in PTS, thus giving a definite diagnosis to these patients. Appropriate management can then be provided. Conclusion: This study identified three novel mutations in either the PAH or PTS gene and supported the use of NGS as an alternative molecular genetic approach for definite diagnosis of hyperphenylalaninemia, thus leading to proper management of these patients in Thailand. Keywords: Next generation sequencing, Exome, Hyperphenylalaninemia, Phenylketonuria, Tetrahydrobiopterin deficiency, Newborn screening Background 120 μmol/l (2 mg/dl), the individual is considered to be Phenylketonuria (PKU) is an autosomal recessive metabolic hyperphenylalaninemia (HPA) and needs further diagnosis disorder, characterized by progressive intellectual disability, [4]. -

Blueprint Genetics Hyperphenylalaninemia Panel
Hyperphenylalaninemia Panel Test code: ME2001 Is a 6 gene panel that includes assessment of non-coding variants. Is ideal for patients with a clinical suspicion of hyperphenylalaninaemias including hyperphenylalaninemia due to BH4 deficiency. The genes on this panel are included in the Comprehansive Metabolism Panel. About Hyperphenylalaninemia Hyperphenylalaninemias (HPA) are errors in metabolism resulting in characterics of elevated levels of phenylalanine amino acid in the blood. Phenylketonuria (PKU) results in hyperphenylalaninemia if left untreated. Elevated levels if phenylalanine will make a severe risk of intellectual disability for a child. Unborn babies with mutation in homozygous state are unaffected as mother’s circulation prevents buildup. After birth, phenylalanine-restricted diet prevents intellectual problems and the persons with homozygous mutated genotype have normal mental development. However, maternal PKU without metabolic control predisposes babies to severe mental retardation and heart defects. This is an example of a genetic disease of a baby based on mother’s genotype. Classical PKU is caused by mutations in PAH, but some 2% of all HPAs result from impaired synthesis or recycling of tetrahydrobiopterin (BH4). Causative mutations in these cases are in GCH1, PCBD1, PTS or QDPR genes. The worldwide prevalence of PKU is estimated at 1:10 000 births having, however, rather big variation in different populations. The prevalence of tetrahydrobiopterin is estimated at <1:500 000 newborns. However, in certain populations -

Cldn19 Clic2 Clmp Cln3
NewbornDx™ Advanced Sequencing Evaluation When time to diagnosis matters, the NewbornDx™ Advanced Sequencing Evaluation from Athena Diagnostics delivers rapid, 5- to 7-day results on a targeted 1,722-genes. A2ML1 ALAD ATM CAV1 CLDN19 CTNS DOCK7 ETFB FOXC2 GLUL HOXC13 JAK3 AAAS ALAS2 ATP1A2 CBL CLIC2 CTRC DOCK8 ETFDH FOXE1 GLYCTK HOXD13 JUP AARS2 ALDH18A1 ATP1A3 CBS CLMP CTSA DOK7 ETHE1 FOXE3 GM2A HPD KANK1 AASS ALDH1A2 ATP2B3 CC2D2A CLN3 CTSD DOLK EVC FOXF1 GMPPA HPGD K ANSL1 ABAT ALDH3A2 ATP5A1 CCDC103 CLN5 CTSK DPAGT1 EVC2 FOXG1 GMPPB HPRT1 KAT6B ABCA12 ALDH4A1 ATP5E CCDC114 CLN6 CUBN DPM1 EXOC4 FOXH1 GNA11 HPSE2 KCNA2 ABCA3 ALDH5A1 ATP6AP2 CCDC151 CLN8 CUL4B DPM2 EXOSC3 FOXI1 GNAI3 HRAS KCNB1 ABCA4 ALDH7A1 ATP6V0A2 CCDC22 CLP1 CUL7 DPM3 EXPH5 FOXL2 GNAO1 HSD17B10 KCND2 ABCB11 ALDOA ATP6V1B1 CCDC39 CLPB CXCR4 DPP6 EYA1 FOXP1 GNAS HSD17B4 KCNE1 ABCB4 ALDOB ATP7A CCDC40 CLPP CYB5R3 DPYD EZH2 FOXP2 GNE HSD3B2 KCNE2 ABCB6 ALG1 ATP8A2 CCDC65 CNNM2 CYC1 DPYS F10 FOXP3 GNMT HSD3B7 KCNH2 ABCB7 ALG11 ATP8B1 CCDC78 CNTN1 CYP11B1 DRC1 F11 FOXRED1 GNPAT HSPD1 KCNH5 ABCC2 ALG12 ATPAF2 CCDC8 CNTNAP1 CYP11B2 DSC2 F13A1 FRAS1 GNPTAB HSPG2 KCNJ10 ABCC8 ALG13 ATR CCDC88C CNTNAP2 CYP17A1 DSG1 F13B FREM1 GNPTG HUWE1 KCNJ11 ABCC9 ALG14 ATRX CCND2 COA5 CYP1B1 DSP F2 FREM2 GNS HYDIN KCNJ13 ABCD3 ALG2 AUH CCNO COG1 CYP24A1 DST F5 FRMD7 GORAB HYLS1 KCNJ2 ABCD4 ALG3 B3GALNT2 CCS COG4 CYP26C1 DSTYK F7 FTCD GP1BA IBA57 KCNJ5 ABHD5 ALG6 B3GAT3 CCT5 COG5 CYP27A1 DTNA F8 FTO GP1BB ICK KCNJ8 ACAD8 ALG8 B3GLCT CD151 COG6 CYP27B1 DUOX2 F9 FUCA1 GP6 ICOS KCNK3 ACAD9 ALG9 -

Comparative Modeling of Methylentetrahydrofolate Reductase (MTHFR) Enzyme and Its Mutational Assessment: in Silico Approach
International Journal of Bioinformatics Research, ISSN: 0975–3087, Volume 2, Issue 1, 2010, pp-05-09 Comparative modeling of methylentetrahydrofolate reductase (MTHFR) enzyme and its mutational assessment: in silico approach Dowlathabad Muralidhara Rao 1*, Anuraj Nayarisseri 2, Mukesh Yadav 2, Showmy K.S.3, Disha Patel 4 1Department of Biotechnology, Bioinformatics Laboratory Sri Krishnadevaraya University, Anantapur, AP, India, [email protected] Ph.08554 255544 Fax.08554 255720 2Eminent Biosciences, Bioinformatics Research Laboratory, Indore, Madhyapradesh, India 3Sree Narayana Guru Institute of Science and Technology, North Paravur, Cochin, Kerala, India 4Softvision College, Viajaynagar, Indore, Madhyapradesh, India Abstract - DNA-synthesis, DNA-repair, and DNA imprinting processes require efficient conversion of homocysteine to methionine. This methylation is catalyzed by methylentetrahydrofolate reductase through reduction of 5,10-methylenetetrahydrofolate into 5-methyltetrahydrofolate. Normal DNA synthesis is considered critical for physiological functions of body. The enzyme is coded by the gene with the symbol MTHFR on chromosome 1 location p36.3 in humans. At least 24 mutations in the MTHFR gene have been identified in people with homocystinuria. There is DNA sequence variants (genetic polymorphisms) associated with this gene. Two of the most investigated are C677T (rs1801133) and A1298C (rs1801131) single nucleotide polymorphisms (SNP). Mutations at C677T and A1298C which confer amino acid substitution Ala222Val and Glu429Ala respectively with a considerable reduced activity. This polymorphism and mild hyperhomocysteinemia are associated with neural tube defects in offspring, arterial and venous thrombosis, and cardiovascular disease. 677TT individuals are at a decreased risk for certain leukemia and colon cancer. The MTHFR gene could be one of the factors of overall schizophrenia risk. -

Molecular Diagnostic Requisition
BAYLOR MIRACA GENETICS LABORATORIES SHIP TO: Baylor Miraca Genetics Laboratories 2450 Holcombe, Grand Blvd. -Receiving Dock PHONE: 800-411-GENE | FAX: 713-798-2787 | www.bmgl.com Houston, TX 77021-2024 Phone: 713-798-6555 MOLECULAR DIAGNOSTIC REQUISITION PATIENT INFORMATION SAMPLE INFORMATION NAME: DATE OF COLLECTION: / / LAST NAME FIRST NAME MI MM DD YY HOSPITAL#: ACCESSION#: DATE OF BIRTH: / / GENDER (Please select one): FEMALE MALE MM DD YY SAMPLE TYPE (Please select one): ETHNIC BACKGROUND (Select all that apply): UNKNOWN BLOOD AFRICAN AMERICAN CORD BLOOD ASIAN SKELETAL MUSCLE ASHKENAZIC JEWISH MUSCLE EUROPEAN CAUCASIAN -OR- DNA (Specify Source): HISPANIC NATIVE AMERICAN INDIAN PLACE PATIENT STICKER HERE OTHER JEWISH OTHER (Specify): OTHER (Please specify): REPORTING INFORMATION ADDITIONAL PROFESSIONAL REPORT RECIPIENTS PHYSICIAN: NAME: INSTITUTION: PHONE: FAX: PHONE: FAX: NAME: EMAIL (INTERNATIONAL CLIENT REQUIREMENT): PHONE: FAX: INDICATION FOR STUDY SYMPTOMATIC (Summarize below.): *FAMILIAL MUTATION/VARIANT ANALYSIS: COMPLETE ALL FIELDS BELOW AND ATTACH THE PROBAND'S REPORT. GENE NAME: ASYMPTOMATIC/POSITIVE FAMILY HISTORY: (ATTACH FAMILY HISTORY) MUTATION/UNCLASSIFIED VARIANT: RELATIONSHIP TO PROBAND: THIS INDIVIDUAL IS CURRENTLY: SYMPTOMATIC ASYMPTOMATIC *If family mutation is known, complete the FAMILIAL MUTATION/ VARIANT ANALYSIS section. NAME OF PROBAND: ASYMPTOMATIC/POPULATION SCREENING RELATIONSHIP TO PROBAND: OTHER (Specify clinical findings below): BMGL LAB#: A COPY OF ORIGINAL RESULTS ATTACHED IF PROBAND TESTING WAS PERFORMED AT ANOTHER LAB, CALL TO DISCUSS PRIOR TO SENDING SAMPLE. A POSITIVE CONTROL MAY BE REQUIRED IN SOME CASES. REQUIRED: NEW YORK STATE PHYSICIAN SIGNATURE OF CONSENT I certify that the patient specified above and/or their legal guardian has been informed of the benefits, risks, and limitations of the laboratory test(s) requested. -

Human Induced Pluripotent Stem Cell–Derived Podocytes Mature Into Vascularized Glomeruli Upon Experimental Transplantation
BASIC RESEARCH www.jasn.org Human Induced Pluripotent Stem Cell–Derived Podocytes Mature into Vascularized Glomeruli upon Experimental Transplantation † Sazia Sharmin,* Atsuhiro Taguchi,* Yusuke Kaku,* Yasuhiro Yoshimura,* Tomoko Ohmori,* ‡ † ‡ Tetsushi Sakuma, Masashi Mukoyama, Takashi Yamamoto, Hidetake Kurihara,§ and | Ryuichi Nishinakamura* *Department of Kidney Development, Institute of Molecular Embryology and Genetics, and †Department of Nephrology, Faculty of Life Sciences, Kumamoto University, Kumamoto, Japan; ‡Department of Mathematical and Life Sciences, Graduate School of Science, Hiroshima University, Hiroshima, Japan; §Division of Anatomy, Juntendo University School of Medicine, Tokyo, Japan; and |Japan Science and Technology Agency, CREST, Kumamoto, Japan ABSTRACT Glomerular podocytes express proteins, such as nephrin, that constitute the slit diaphragm, thereby contributing to the filtration process in the kidney. Glomerular development has been analyzed mainly in mice, whereas analysis of human kidney development has been minimal because of limited access to embryonic kidneys. We previously reported the induction of three-dimensional primordial glomeruli from human induced pluripotent stem (iPS) cells. Here, using transcription activator–like effector nuclease-mediated homologous recombination, we generated human iPS cell lines that express green fluorescent protein (GFP) in the NPHS1 locus, which encodes nephrin, and we show that GFP expression facilitated accurate visualization of nephrin-positive podocyte formation in -

Vitamin D in Critically Ill Patients
Thesis/Dissertation Sheet Surname/Family Name : Nair Given Name/s : Priya Abbreviation for degree as give in the University calendar : PhD Faculty : Medicine School : St. Vincent’s Clinical School Thesis Title : Vitamin D in critically ill patients The pleiotropic functions of vitamin D, the clinical impact of deficiency and effect of supplementation have been a research focus in many specialties of ambulatory medicine. However, its prevalence in critical illness was not known. The parathyroid-vitamin D- calcium axis is the only endocrine axis that had not been previously described in critically ill patients. To study the effects of correction of deficiency, the dose, route and method of vitamin D supplementation needed investigation. Critically ill patients are heterogeneous and response to supplementation may not be consistent in all cohorts. This information is key to inform the design of a randomised controlled trial of supplementation. This thesis was a program of research that included a prospective observational study to describe serial changes in the parathyroid-vitamin D-calcium axis and the association with clinical outcomes in a sample of critically ill patients. This was followed by a randomised trial comparing two doses of intramuscular vitamin D to study the effectiveness and safety of supplementation. Subsequently, a sample of patients requiring life- sustaining extracorporeal support (ECMO) was studied to study pharmacokinetic profiles of vitamin D in patients with extreme disease severity. The observational study found marked changes in the parathyroid-vitamin D-calcium axis, which was associated with adverse outcomes. The supplementation study showed that a single intramuscular injection of cholecalciferol corrected vitamin D deficiency safely in critically ill patients. -

CENTOGENE's Severe and Early Onset Disorder Gene List
CENTOGENE’s severe and early onset disorder gene list USED IN PRENATAL WES ANALYSIS AND IDENTIFICATION OF “PATHOGENIC” AND “LIKELY PATHOGENIC” CENTOMD® VARIANTS IN NGS PRODUCTS The following gene list shows all genes assessed in prenatal WES tests or analysed for P/LP CentoMD® variants in NGS products after April 1st, 2020. For searching a single gene coverage, just use the search on www.centoportal.com AAAS, AARS1, AARS2, ABAT, ABCA12, ABCA3, ABCB11, ABCB4, ABCB7, ABCC6, ABCC8, ABCC9, ABCD1, ABCD4, ABHD12, ABHD5, ACACA, ACAD9, ACADM, ACADS, ACADVL, ACAN, ACAT1, ACE, ACO2, ACOX1, ACP5, ACSL4, ACTA1, ACTA2, ACTB, ACTG1, ACTL6B, ACTN2, ACVR2B, ACVRL1, ACY1, ADA, ADAM17, ADAMTS2, ADAMTSL2, ADAR, ADARB1, ADAT3, ADCY5, ADGRG1, ADGRG6, ADGRV1, ADK, ADNP, ADPRHL2, ADSL, AFF2, AFG3L2, AGA, AGK, AGL, AGPAT2, AGPS, AGRN, AGT, AGTPBP1, AGTR1, AGXT, AHCY, AHDC1, AHI1, AIFM1, AIMP1, AIPL1, AIRE, AK2, AKR1D1, AKT1, AKT2, AKT3, ALAD, ALDH18A1, ALDH1A3, ALDH3A2, ALDH4A1, ALDH5A1, ALDH6A1, ALDH7A1, ALDOA, ALDOB, ALG1, ALG11, ALG12, ALG13, ALG14, ALG2, ALG3, ALG6, ALG8, ALG9, ALMS1, ALOX12B, ALPL, ALS2, ALX3, ALX4, AMACR, AMER1, AMN, AMPD1, AMPD2, AMT, ANK2, ANK3, ANKH, ANKRD11, ANKS6, ANO10, ANO5, ANOS1, ANTXR1, ANTXR2, AP1B1, AP1S1, AP1S2, AP3B1, AP3B2, AP4B1, AP4E1, AP4M1, AP4S1, APC2, APTX, AR, ARCN1, ARFGEF2, ARG1, ARHGAP31, ARHGDIA, ARHGEF9, ARID1A, ARID1B, ARID2, ARL13B, ARL3, ARL6, ARL6IP1, ARMC4, ARMC9, ARSA, ARSB, ARSL, ARV1, ARX, ASAH1, ASCC1, ASH1L, ASL, ASNS, ASPA, ASPH, ASPM, ASS1, ASXL1, ASXL2, ASXL3, ATAD3A, ATCAY, ATIC, ATL1, ATM, ATOH7, -

Nutrition Journal of Parenteral and Enteral
Journal of Parenteral and Enteral Nutrition http://pen.sagepub.com/ Micronutrient Supplementation in Adult Nutrition Therapy: Practical Considerations Krishnan Sriram and Vassyl A. Lonchyna JPEN J Parenter Enteral Nutr 2009 33: 548 originally published online 19 May 2009 DOI: 10.1177/0148607108328470 The online version of this article can be found at: http://pen.sagepub.com/content/33/5/548 Published by: http://www.sagepublications.com On behalf of: The American Society for Parenteral & Enteral Nutrition Additional services and information for Journal of Parenteral and Enteral Nutrition can be found at: Email Alerts: http://pen.sagepub.com/cgi/alerts Subscriptions: http://pen.sagepub.com/subscriptions Reprints: http://www.sagepub.com/journalsReprints.nav Permissions: http://www.sagepub.com/journalsPermissions.nav >> Version of Record - Aug 27, 2009 OnlineFirst Version of Record - May 19, 2009 What is This? Downloaded from pen.sagepub.com by Karrie Derenski on April 1, 2013 Review Journal of Parenteral and Enteral Nutrition Volume 33 Number 5 September/October 2009 548-562 Micronutrient Supplementation in © 2009 American Society for Parenteral and Enteral Nutrition 10.1177/0148607108328470 Adult Nutrition Therapy: http://jpen.sagepub.com hosted at Practical Considerations http://online.sagepub.com Krishnan Sriram, MD, FRCS(C) FACS1; and Vassyl A. Lonchyna, MD, FACS2 Financial disclosure: none declared. Preexisting micronutrient (vitamins and trace elements) defi- for selenium (Se) and zinc (Zn). In practice, a multivitamin ciencies are often present in hospitalized patients. Deficiencies preparation and a multiple trace element admixture (containing occur due to inadequate or inappropriate administration, Zn, Se, copper, chromium, and manganese) are added to par- increased or altered requirements, and increased losses, affect- enteral nutrition formulations. -

PTS Gene 6-Pyruvoyltetrahydropterin Synthase
PTS gene 6-pyruvoyltetrahydropterin synthase Normal Function The PTS gene provides instructions for making an enzyme called 6- pyruvoyltetrahydropterin synthase. This enzyme is involved in the second of three steps in the production of a molecule called tetrahydrobiopterin (BH4). Other enzymes help carry out the first and third steps in this process. Tetrahydrobiopterin plays a critical role in processing several protein building blocks ( amino acids) in the body. For example, it works with the enzyme phenylalanine hydroxylase to convert an amino acid called phenylalanine into another amino acid, tyrosine. Tetrahydrobiopterin is also involved in reactions that produce chemicals called neurotransmitters, which transmit signals between nerve cells in the brain. Because it helps enzymes carry out chemical reactions, tetrahydrobiopterin is known as a cofactor. Health Conditions Related to Genetic Changes Tetrahydrobiopterin deficiency More than 45 mutations in the PTS gene have been found to cause tetrahydrobiopterin deficiency. When this condition is caused by PTS gene mutations, it is known as 6- pyruvoyltetrahydropterin synthase (PTS) deficiency. PTS deficiency accounts for more than half of all cases of tetrahydrobiopterin deficiency. Most PTS gene mutations change single amino acids in 6-pyruvoyltetrahydropterin synthase, although some mutations insert or delete small amounts of DNA in the PTS gene or disrupt the way the gene's instructions are used to make the enzyme. Changes in 6-pyruvoyltetrahydropterin synthase greatly reduce or eliminate the enzyme's activity. Without enough of this enzyme, little or no tetrahydrobiopterin is produced. As a result, this cofactor is not available to participate in chemical reactions such as the conversion of phenylalanine to tyrosine.