Suramin Pharmacokinetics After Regional Or Systemic
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Theranostics Characterization of Drug-Induced Human Mitochondrial ADP/ATP Carrier Inhibition
Theranostics 2021, Vol. 11, Issue 11 5077 Ivyspring International Publisher Theranostics 2021; 11(11): 5077-5091. doi: 10.7150/thno.54936 Research Paper Characterization of drug-induced human mitochondrial ADP/ATP carrier inhibition Stephany Jaiquel Baron1, Martin S. King1, Edmund R.S. Kunji1, and Tom J.J. Schirris1,2 1. Medical Research Council Mitochondrial Biology Unit, University of Cambridge, Cambridge Biomedical Campus, Keith Peters Building, Hills Road, Cambridge, CB2 0XY, United Kingdom. 2. Department of Pharmacology and Toxicology, Radboud Institute for Molecular Life Sciences, Radboud Center for Mitochondrial Medicine, Radboud University Medical Center, Nijmegen, The Netherlands. Corresponding authors: Prof. Dr. Edmund R.S. Kunji, MRC Mitochondrial Biology Unit, University of Cambridge, Keith Peters Building, Cambridge Biomedical Campus, Hills Road, Cambridge, CB2 0XY, United Kingdom; Phone: +44 12 232 52 850; Fax: +44 12 232 52 875; Email: [email protected]; Dr. T.J.J. Schirris, ERT, Department of Pharmacology and Toxicology, Radboud University Medical Center, PO Box 9101, 6500 HB Nijmegen, The Netherlands; Phone: +31 61 517 63 47; E-mail: [email protected] © The author(s). This is an open access article distributed under the terms of the Creative Commons Attribution License (https://creativecommons.org/licenses/by/4.0/). See http://ivyspring.com/terms for full terms and conditions. Received: 2020.10.24; Accepted: 2021.01.18; Published: 2021.03.05 Abstract An increasing number of commonly prescribed drugs are known to interfere with mitochondrial function, causing cellular toxicity, but the underlying mechanisms are largely unknown. Although often not considered, mitochondrial transport proteins form a significant class of potential mitochondrial off-targets. -
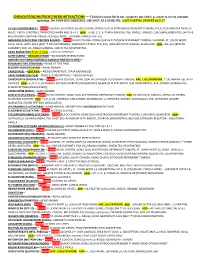
CHEMO/FOOD/NUTRIENT/HERB INTERACTIONS ***This List Is Most Likely Not Complete, Not 100% Accurate & Needs Constant Updating
CHEMO/FOOD/NUTRIENT/HERB INTERACTIONS ***This list is most likely not complete, not 100% accurate & needs constant updating. DO YOUR DUE DILIGENCE, USE ONLY AS A GUIDLINE. LAST PARTIAL UPDATE 10.5.17 5-FU (5-FLUOROURACIL)—AVOID ALCOHOL (GI UPSET), BLACK COHOSH, DONG QUAI IN ESTROGEN DEPENDANT TUMORS, FOLIC ACID GREATER THAN 15 MG/D, ? BETA-CAROTENE, PROBIOTICS WHEN WBC IS <2.5. ADD—A, B6, C, E, K, PANAX GINSENG, PSK, GARLIC, GINKGO, CURCUMIN, GREEN TEA, SHITAKE MUSHROOM-LENTINAN, PROBIOTICS GLUTAMINE, AVEMAR, GINGER, FISH OIL. ABRAXANE (PACLITAXEL PROTEIN BOUND)— AVOID BLACK COHOSH, DONG QUAI IN ESTROGEN-DEPENDANT TUMORS, VALERIAN, ST. JOHNS WORT, KAVA- KAVA, GOTU KOLA (MAY ↑CNS DEPRESSION). SUBSTRATE CPY2CA, 2C9, 3A4; INDUCER CYP3A4 (WEAK), ECHINACEA. ADD—B6, GLA [EPO OR CURRANT], FISH OIL, PANAX GINSENG, GREEN TEA, RESVERATROL. ACNU NIMUSTINE) Phase 2 StUdy—USED IN GERMANY ALTRETAMINE—HEXALEN (HMM)—NO KNOWN INTERACTIONS AMRUBICIN-HYDROCHLORIDE (CALSED) (FOREIGN NAME)— BENDAMUSTINE (TREANDA)—NONE AT THIS TIME BLEOMYCIN (BLENOXANE)—NONE KNOWN. CABAZITAXEL—(JEVTANA)—AVOID GRAPEFRUIT, CYP3A METABOLIZE. CAPECITABINE (XELODA)—FOOD ↓’S ABSORPTION, ? AND ECHINACEA. CARBOPLATIN (PARAPLATIN)— AVOID BLACK COHOSH, DONG QUAI IN ESTROGEN-DEPENDANT TUMORS, NAC, L-GLUTATHIONE, ?? SILYMARIN USE WITH CAUTION. ADD—C, D, E, K, SILYMARIN, POLYSACCHARIDES [MUSHROOMS AGARICUS BLAZEI (ROYAL SUN FROM BRAZIL), ALA, GINGER, ASTRAGALUS, SPLEEN PEPTIDES (DESICCATED)], CARMUSTINE (BCNU)—NONE KNOWN. CISPLATIN (PLATINOL)—AVOID BLACK COHOSH, DONG QUAI IN ESTROGEN-DEPENDANT TUMORS, NAC, B6 300 MG/D, GINKGO + REGULAR ASPIRIN, SILYMARIN CAUTION. ADD—A, E, K, B6 <300MG/D, MELATONIN, MAGNESIUM, L-CARNITINE, GINGKO, ASTRAGALUS, PSK, SILYMARIN, GINGER QUERCETIN, SPLEEN PEPTIDES [DESICCATED]. CHLORAMBUCIL (LEUKERAN)—NONE KNOWN, ABSORPTION IS DECREASED WITH FOOD CLADRIBINE (LEUSTATIN)— AVOID ALCOHOL GI UPSET. -

Suramin Sodium Salt
Suramin sodium salt Product Number S 2671 Store at room temperature Product Description Precautions and Disclaimer Molecular Formula: C51H34N6Na6O23S6 For Laboratory Use Only. Not for drug, household or Molecular Weight: 1429 other uses. CAS Number: 129-46-4 Preparation Instructions Suramin inhibits parasite and human enzymes The product is soluble in water (50 mg/ml), yielding a including trypanosoma glycolytic enzymes, human clear, faint yellow solution. It is also soluble in DNA and RNA polymerases, human reverse physiological saline, sparingly soluble in 95% ethanol, transcripase, ATPase, protein kinase C, and human insoluble in benzene, ether, petroleum ether, and 3 lysosomal enzymes such as β-glucuronidase. chloroform. Suramin is a trypanocide used in the treatment of the early stages of African trypanosomiasis and is Storage/Stability effective as an anthelmintic in the treatment of Solutions deteriorate on storage and should be used onchocerciasis.1 It has been shown to have activity immediately after preparation. Protect product from against HIV, but with disappointing results and has light. been reported to have some antineoplastic activity.2 In in vitro studies, suramin inhibited the reverse References transcriptase of HIV,2,3,4 HIV infectivity, and the 1. Martindale The Extra Pharmacopoeia, 30th ed., cytopathic effect on helper/inducer T cells.5 Reynolds, J. E. F., ed., The Pharmaceutical Press (London, England: 1993), p. 528. Suramin is a hexasulfonated naphthylurea compound 2. Stein, C. A., et al., Suramin: an Anticancer Drug used as an anti-tumor drug and is a potent inhibitor of with a Unique Mechanism of Action. J. Clin. human neutrophil elastase, cathepsin G, and Oncol.,7(4), 499-508 (1989). -

Suramin As a Chemo- and Radio-Sensitizer
SURAMIN AS A CHEMO- AND RADIO-SENSITIZER: PRECLINICAL TRANSLATIONAL STUDIES DISSERTATION Presented in Partial Fulfillment of the Requirements for the Degree Doctor of Philosophy in the Graduate School of The Ohio State University By Yan Xin, M.S. ***** The Ohio State University 2006 Dissertation Committee: Dr. M. Guillaume Wientjes, Adviser Approved by Dr. Jessie L.-S. Au ____________________________________ Adviser Dr. Duxin Sun Graduate Program in Pharmacy ABSTRACT Previous studies in our laboratory showed that low-dose suramin, an inhibitor of fibroblast growth factor action, enhances sensitivity of various human tumors in preclinical and clinical studies to chemotherapy. Chemosensitization required apoptosis, and increased the extent and duration of the induction of apoptosis. The primary focus of this dissertation research was to explore, in preclinical studies, therapeutic approaches for therapy enhancement based on this mechanism. A phase III clinical trial in superficial bladder cancer, which emanated from our laboratory, showed that optimizing mitomycin C delivery nearly doubled the recurrence- free survival of treated patients to 40%. Tumor sensitization with suramin might yield further therapeutic improvements, and was investigated in in vitro and in vivo studies. Studies in Chapter 2 demonstrated enhanced antitumor activity of mitomycin C, administered at subtherapeutic and therapeutic regimens. Various preclinical and clinical studies determined that suramin sensitized tumor tissue at low but not at high concentrations, presumably due to additional pharmacologic effects at elevated concentrations. Studies to overcome this limitation, especially in tumors containing high fibroblast growth factor concentrations, used pentosan polysulfate, another nonspecific FGF inhibitor. This agent was also a chemosensitizer, but combined use with suramin did not increase the overall efficacy (Chapter 3). -

World Health Organization Model List of Essential Medicines, 21St List, 2019
World Health Organizatio n Model List of Essential Medicines 21st List 2019 World Health Organizatio n Model List of Essential Medicines 21st List 2019 WHO/MVP/EMP/IAU/2019.06 © World Health Organization 2019 Some rights reserved. This work is available under the Creative Commons Attribution-NonCommercial-ShareAlike 3.0 IGO licence (CC BY-NC-SA 3.0 IGO; https://creativecommons.org/licenses/by-nc-sa/3.0/igo). Under the terms of this licence, you may copy, redistribute and adapt the work for non-commercial purposes, provided the work is appropriately cited, as indicated below. In any use of this work, there should be no suggestion that WHO endorses any specific organization, products or services. The use of the WHO logo is not permitted. If you adapt the work, then you must license your work under the same or equivalent Creative Commons licence. If you create a translation of this work, you should add the following disclaimer along with the suggested citation: “This translation was not created by the World Health Organization (WHO). WHO is not responsible for the content or accuracy of this translation. The original English edition shall be the binding and authentic edition”. Any mediation relating to disputes arising under the licence shall be conducted in accordance with the mediation rules of the World Intellectual Property Organization. Suggested citation. World Health Organization Model List of Essential Medicines, 21st List, 2019. Geneva: World Health Organization; 2019. Licence: CC BY-NC-SA 3.0 IGO. Cataloguing-in-Publication (CIP) data. CIP data are available at http://apps.who.int/iris. -

WO 2017/123633 Al 20 July 2017 (20.07.2017) W P O P C T
(12) INTERNATIONAL APPLICATION PUBLISHED UNDER THE PATENT COOPERATION TREATY (PCT) (19) World Intellectual Property Organization Illl ll II 11III I II I ill llll II III II I II International Bureau (10) International Publication Number (43) International Publication Date WO 2017/123633 Al 20 July 2017 (20.07.2017) W P O P C T (51) International Patent Classification: DO, DZ, EC, EE, EG, ES, FI, GB, GD, GE, GH, GM, GT, C07K 14/705 (2006.01) A61K 31/00 (2006.01) HN, HR, HU, ID, IL, IN, IR, IS, JP, KE, KG, KH, KN, CO 37/10 (2006.01) KP, KR, KW, KZ, LA, LC, LK, LR, LS, LU, LY, MA, MD, ME, MG, MK, MN, MW, MX, MY, MZ, NA, NG, (21) International Application Number: NI, NO, NZ, OM, PA, PE, PG, PH, PL, PT, QA, RO, RS, PCT/US2017/013015 RU, RW, SA, SC, SD, SE, SG, SK, SL, SM, ST, SV, SY, (22) International Filing Date: TH, TJ, TM, TN, TR, TT, TZ, UA, UG, US, UZ, VC, VN, 11 January 2017 ( 11.01 .2017) ZA, ZM, ZW. (25) Filing Language: English (84) Designated States (unless otherwise indicated, for every kind of regional protection available): ARIPO (BW, GH, (26) Publication Language: English GM, KE, LR, LS, MW, MZ, NA, RW, SD, SL, ST, SZ, (30) Priority Data: TZ, UG, ZM, ZW), Eurasian (AM, AZ, BY, KG, KZ, RU, 62/277,422 11 January 2016 ( 11.01.2016) U S TJ, TM), European (AL, AT, BE, BG, CH, CY, CZ, DE, DK, EE, ES, FI, FR, GB, GR, HR, HU, IE, IS, IT, LT, LU, (71) Applicant: DIGNITY HEALTH [US/US]; 3033 N . -

Overview of Planned Or Ongoing Studies of Drugs for the Treatment of COVID-19
Version of 16.06.2020 Overview of planned or ongoing studies of drugs for the treatment of COVID-19 Table of contents Antiviral drugs ............................................................................................................................................................. 4 Remdesivir ......................................................................................................................................................... 4 Lopinavir + Ritonavir (Kaletra) ........................................................................................................................... 7 Favipiravir (Avigan) .......................................................................................................................................... 14 Darunavir + cobicistat or ritonavir ................................................................................................................... 18 Umifenovir (Arbidol) ........................................................................................................................................ 19 Other antiviral drugs ........................................................................................................................................ 20 Antineoplastic and immunomodulating agents ....................................................................................................... 24 Convalescent Plasma ........................................................................................................................................... -

Caffeine Consumption with Relevance to Type 3 Diabetes and Accelerated Brain Aging
View metadata, citation and similar papers at core.ac.uk brought to you by CORE provided by Research Online @ ECU Edith Cowan University Research Online ECU Publications Post 2013 2017 Caffeine consumption with relevance to Type 3 diabetes and accelerated brain aging I. J. Martins Edith Cowan University, [email protected] Follow this and additional works at: https://ro.ecu.edu.au/ecuworkspost2013 Part of the Diseases Commons Martins. I. J. (2017). Caffeine consumption with relevance to Type 3 diabetes and accelerated brain aging. Research & Reviews: Neuroscience, 1(1), 1-5. Available here This Editorial is posted at Research Online. https://ro.ecu.edu.au/ecuworkspost2013/3780 Research & Reviews: Neuroscience Caffeine Consumption with Relevance to Type 3 Diabetes and Accelerated Brain Aging Martins IJ* Centre of Excellence in Alzheimer’s Disease Research and Care, School of Medical Sciences, Edith Cowan University, Australia Editorial Article Received date: 20/10/2016 *For Correspondence Accepted date: 21/10/2016 School of Medical Sciences, Edith Cowan University, 270 Joondalup Drive, Published date: 22/10/2016 Joondalup, Western Australia 6027, Australia, Ph: +61863042574, E-mail: [email protected] Keywords: Caffeine, diabetes, Sirtuin 1 EDITORIAL The main constituent of plaques in the brain of Alzheimer’s disease (AD) individuals namely amyloid beta (Aβ) [1] is a pro- teolytic product of a larger protein, the amyloid precursor protein (APP) protein. Carriers of the apo E4 allele are at greater risk of developing AD with increased deposition of amyloid beta plaques in Western countries. Apo E4 is also a major risk factor for cardiovascular disease linked to defective cholesterol metabolism [2,3]. -

Suramin: a Novel Antineoplastic Agent with Multiple Potential Mechanisms of Action1
[CANCER RESEARCH 53. 2239-2248. May 15. 1993] Perspectives in Cancer Research Suramin: A Novel Antineoplastic Agent with Multiple Potential Mechanisms of Action1 C. A. Stein n?partmenl of Medicine. Columbia University. College of Physicians and Surgeons. New York. New York In the June 1992 edition of the Journal of Clinical Oncology, Myers Hawking (6). He noted that the drug could bind to and inhibit the el al. ( 1) reported on 38 cases of metastatic hormone refractory pros function of a wide variety of enzymes and proteins, although he could tate cancer treated with suramin, a bis-polysulfonated naphthylurea. In detect no underlying unifying themes. These enzymes included hy- the accompanying editorial. Pinedo and van Rijswijk (2) state that aluronidase, fumarase, urease, hexokinase, Na+-K^ ATPase and RNA "there can be little doubt that suramin represents an important new polymerase. Suramin was also a potent in vitro anticoagulant, and an group of anticancer agents." In fact, the recent encouraging results in vivo teratogen. Its clinical pharmacology and toxicology were, in with suramin as an antineoplastic agent have occurred as a result of retrospect, not understood well. decades of patient groundwork, followed by a few key observations in In 1979, DeClerq (7) appreciated that suramin could inhibit the patients with acquired immunodeficiency syndrome being treated activity of the reverse transcriptase found in RNA tumor viruses, such with suramin as part of a clinical therapeutic trial. The drug is highly as the murine leukemia. Moloney sarcoma, and avian myeloblastosis unusual, both in its biological properties and in the story of its devel viruses. -

The Effect of Suramin (A Calmodulin Antagonist) on Caffeine-Induced Ca2+-Release in Mechanically Skinned Fast-Twitch Skeletal Mu
The effect of suramin (a calmodulin antagonist) on caffeine-induced Ca2+-release in mechanically skinned fast-twitch skeletal muscle fibres of the rat D.W.Williams, G.S. Posterino and D.G. Stephenson, Department of Zoology,Latrobe University,VIC 3086, Australia. Calmodulin (CaM) is a ubiquitous, multifunctional calcium binding protein, which binds to the ryanodine receptor (RyR1) in skeletal muscle (Tripathy et al.,1995). Ca2+-free CaM binds to RYR1 and increases RYR1s affinity for calcium, while Ca2+-bound CaM inhibits RYR1s affinity for calcium (Rodney et al.,2000). The precise role of CaM in the regulation of calcium release in physiological preparations remains unknown. Suramin is a broad acting CaM antagonist known to displace bound CaM from RyRs (Sigalas et al.,2009). In this study we investigated the effects of suramin on Ca2+ release from the sarcoplasmic reticulum (SR) in freshly mechanically skinned muscle fibres where the SR is intact under conditions where the suramin treatment did not affect the ability of the contractile apparatus to develop force. All experiments conducted were approvedbythe La Trobe University Animal Ethics committee. Rats were killed by an overdose of isoflurane (4% volume: volume) and whole EDL muscles were removedand pinned out on a bed of Sylgard at resting length under paraffin oil. Single fibres were then isolated under a dissecting microscope, mechanically skinned, and mounted between a pair of forceps and a sensitive force transducer.After mounting to the force recording apparatus, fibres were bathed in a K-based solution that mimics the normal intracellular environment with respect to pH (7.10); monovalent ions (137 mM); Mg2+ (1 mM); divalent cations (60 mM); total ATP (8 mM); osmolality (295 mOsm/L); [Ca2+] ∼100 nM. -

Guidelines for the Diagnosis, Treatment and Control of Canine Endoparasites in the Tropics. Second Edition March 2019
Tro CCAP Tropical Council for Companion Animal Parasites Guidelines for the diagnosis, treatment and control of canine endoparasites in the tropics. Second Edition March 2019. First published by TroCCAP © 2017 all rights reserved. This publication is made available subject to the condition that any redistribution or reproduction of part or all of the content in any form or by any means, electronic, mechanical, photocopying, recording, or otherwise is with the prior written permission of TroCCAP. Disclaimer The guidelines presented in this booklet were independently developed by members of the Tropical Council for Companion Animal Parasites Ltd. These best-practice guidelines are based on evidence-based, peer reviewed, published scientific literature. The authors of these guidelines have made considerable efforts to ensure the information upon which they are based is accurate and up-to-date. Individual circumstances must be taken into account where appropriate when following the recommendations in these guidelines. Sponsors The Tropical Council for Companion Animal Parasites Ltd. wish to acknowledge the kind donations of our sponsors for facilitating the publication of these freely available guidelines. Contents General Considerations and Recommendations ............................................................................... 1 Gastrointestinal Parasites .................................................................................................................... 3 Hookworms (Ancylostoma spp., Uncinaria stenocephala) .................................................................... -

Suramin Inhibits Cell Proliferation in Ovarian and Cervical Cancer By
Li et al. Cancer Cell International (2015) 15:52 DOI 10.1186/s12935-015-0196-y PRIMARY RESEARCH Open Access Suramin inhibits cell proliferation in ovarian and cervical cancer by downregulating heparanase expression HuaPing Li1, HuaLi Li2, HongJie Qu3, MingZhu Zhao1, Bo Yuan3, MingHua Cao1 and JinQuan Cui3* Abstract Background: Aberrant expression of heparanase (Hpa) is associated with apoor prognosis in ovarian and cervical cancer patients. Inhibitors of Hpa can prevent the growth and metastasis of malignant tumor cells, and suramin may be such a compound that has strong anti-proliferative effects on several kinds of cancer cells. We have therefore tested whether the growth inhibiting effect of suramin on ovarian and cervical cancer cells is due to downregulation of Hpa expression. Results: Suramin at 300–600 μg/ml significantly inhibited HO-8910 PM and HeLa cell growth at 24 h, in both a time-dependent and dose-dependent manner, with an IC50 of 320 μg/ml and 475 μg/ml, respectively. Suramin at 300 μg/ml significantly decreased the expression of Hpa mRNA (P < 0.005) and protein (P < 0.005) in both HO-8910 PM and HeLa cells at 48 h. Conclusions: The inhibitory effect of suramin on Hpa enzyme may be due to downregulating of its expression in cancer cells. These findings confirm the importance of Hpa in tumor growth and the potential clinical application of Hpa inhibitors in the treatment of ovarian and cervical cancer. Keywords: Suramin, Inhibition, Heparanase, Ovarian cancer, Cervical cancer Background no truly effective second and third line therapeutic regi- Ovarian cancer is the fifth most common cause of can- mens are in place.